A Conservative Orthograde Approach for Successful Nonsurgical Management of Mandibular Central Incisor with Large Periapical Lesion and Inflammatory Root Resorption
Division of Endodontics, Dentistry Program, Batterjee Medical College, KSA, Email: gufaran.ali@bmc.edu.sa
Citation: Baragaa E, et al. A Conservative Orthograde Approach for Successful Nonsurgical Management of Mandibular Central Incisor with Large Periapical Lesion and Inflammatory Root Resorption. Ann Med Health Sci Res. 2021;11:1424-1427.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Due to trauma, teeth can have an extensive lesion along with external inflammatory resorption, with no history of pain or mobility, which can be discovered in routine dental examination only. Depends on the case, treatment options of such teeth may vary, and can include both, surgical or nonsurgical approach. Various clinical studies have confirmed that with simple nonsurgical root canal treatment, even large periapical lesions can be treated successfully, if the lesion is in direct communication with the root canal system. Recently, few cases have been published, in which large periapical lesions with external inflammatory resorption has been successfully treated by nonsurgical root canal treatment. This article also reports a case in which a mandibular central incisor with a large periapical lesion and inflammatory root resorption has been treated successfully with nonsurgical endodontic therapy.
Keywords
Nonsurgical root canal treatment; Large periapical lesion; Inflammatory root resorption; MTA
Introduction
Root resorption in permanent teeth is uncommon, [1] pathological [1,2] dental complication, [3] that involves the interaction between inflammatory cells, hard tissue structure, and resorbing cells. [2] Root resorption can even lead to tooth extraction, [3] as it is not only difficult to predict and diagnose, but also quite difficult to treat. [2] Active resorption is seen because of stimulation of osteoclastic cells by pressure or infection, and if the etiological factor is removed completely, resorption can be reversed. [3]
Amongst all etiological factors, pulpal infection is the most common factor that not only leads to the formation of periapical lesions, [3-5] but also leads to tooth resorption, [3] which are mainly, more than 90%, are classified into radicular cysts (6%- 55%), periapical granuloma (9.3%-87.1%), and periapical abscess (28.7%-70.7%). [4] Radiographically, periapical lesions cannot be differentiated between cyst or granuloma. [5] However, studies showed that incidence of cyst is more than 92%, if radiographic lesion size is 200 mm2 or more. [4,5]
Treatment approaches for large periapical lesions range from tooth extraction to nonsurgical root canal treatment with or without endodontic surgery. [4] Various clinical studies have confirmed that with simple nonsurgical root canal treatment, even large periapical lesions can be treated successfully, if the lesion is in direct communication with the root canal system. [4,5]
Thus, the purpose of this article is to report the clinical case of a lower anterior (tooth #41) with pulp necrosis, large periradicular lesion, and inflammatory apical root resorption, which has been managed successfully by simple nonsurgical root canal treatment.
Case Report
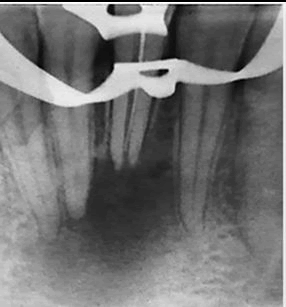
A 27-year-old male patient came to the Endodontic division at A Conservative Orthograde Approach for Successful Nonsurgical Management of Mandibular Central Incisor with Large Periapical Lesion and Inflammatory Root Resorption Emtinan Baragaa1 and Gufaran Ali Syed2* 1 Dentistry, KSA; 2 Batterjee Medical College with a chief complaint of discolored lower front tooth due to a history of trauma 10 years ago. Clinical examination with #41 revealed brown discoloration of the tooth, no response to the cold test, no mobility, no sinus opening, and the canal was open to the oral cavity (as RCT has been attempted by other dentist before). Pain on percussion and palpation was absent. Radiographic examination showed a large periapical lesion and inflammatory apical root resorption of tooth #41 [Figure 1]. Radiographically it was appearing as if the periapical lesion was involving the root of tooth #31 and #42 [Figure 1], but with vitality test, both tooth #31 and #42 were vital with normal response. After clinical and radiographic examination, tooth #41 was diagnosed as previously initiated with asymptomatic apical periodontitis.
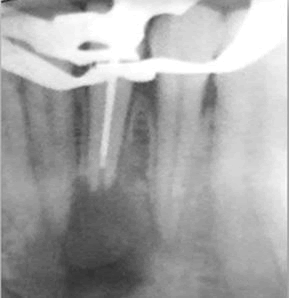
After careful evaluation and discussion with the patient, nonsurgical root canal treatment was planned. After administering local anesthesia, 4% Articaine with 1:100.000 epinephrine (Septodont, France), rubber dam was placed and the access cavity was modified with Endo access bur (Dentsply Maillefer, Switzerland) and Endo-Z bur (DentsplyMaillefer, Switzerland) using high speed hand-piece (Sirona Dental Systems. Fabrikstrabe 31). Two canal orifices were identified (Buccal and Lingual), and the working length was determined using an apex locator (Dentaport ZX, J. Morita, Japan) and periapical x-ray, as 12 mm for the buccal canal and 13 mm for the lingual canal [Figure 2].
Cleaning and shaping for both canals was done using the hybrid technique till #60 K-file as the master apical file. During the entire cleaning and shaping procedure, copious irrigation was done using 5.25% sodium hypochlorite (NaOCl) (Clorox, Saudi Arabia). After completion of cleaning and shaping, final irrigation was done using 17% aqueous EDTA (Pyrax, India) and 5.25% NaOCl to remove the smear layer. After cleaning and shaping calcium hydroxide with iodoform (Meta Biomed Co. Ltd, Korea) was placed as an intracanal medicament, and then the cotton pellet was placed on the orifice and the access opening was closed using the glass ionomer cement (GC Fuji IX, GC Corporation, Japan). Patient was recalled after 4 weeks.
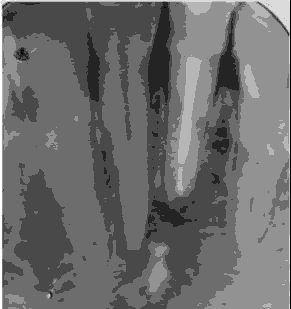
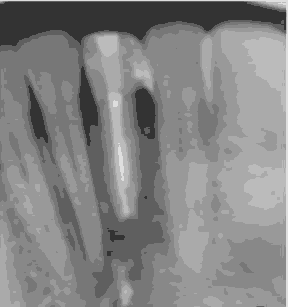
During the second visit, after application of the rubber dam, the intracanal dressing was removed and all canals were irrigated with 5.25% NaOCl and dried with sterile paper points (Meta Biomed Co. Ltd, Korea). The canals were then obturated with the lateral condensation technique, using guttapercha points (Meta Biomed Co. Ltd, Korea), and MTA Fillapex sealer (MTA Fillapex, Angelus, Brazil), and then the access opening was closed with composite restoration (3 M, restoration) and a postoperative radiograph was taken [Figure 3]. To assess healing, radiographs were taken when the patient came for follow-up visits after 6 months [Figure 4], 12 months [Figure 5], and 18 months [Figure 6].
Discussion
Dental trauma, which causes pulp necrosis with exposed dentinal tubules on the the damaged root surface, is the most common cause for external root resorption. [2] There are different treatment options for large periradicular lesions ranging from
nonsurgical root canal treatment to surgical procedure. We did the nonsurgical root canal treatment, because studies have shown that nonsurgical root canal treatment must be done first and reports have shown that 42% to 72 % of these lesions healed after sufficient root canal debridement and obturation, which is the key for successful endodontic treatment. [4]
We kept the working length short by 2 mm from the radiographic apex, because according to Weine’s subtraction rules, the working length should be shortened by 2 mm from the radiographic apex, if both, bone and external root resorption are present. [6] During cleaning and shaping, we have used 5% NaOCl for irrigation, because apart from flushing out the debris, it efficiently dissolves the organic material, and has an excellent antimicrobial property, [7] as it causes biosynthetic alterations in cellular metabolism and phospholipid destruction, forms chloramines that conflict in cellular metabolism, has oxidative action with irreversible enzymatic inactivation in bacteria, and causes lipid and fatty acid degradation. [8]
After completing the cleaning and shaping, we have used aqueous EDTA in combination with NaOCl, to remove the smear layer, which blocks the penetration of resin into the dentinal tubules that jeopardized the sealing efficiency of the obturation of the root canal. [8] After removing the smear layer, we placed calcium hydroxide as an intracanal medicament, because it promotes periapical healing by inhibiting the bacterial enzymes, [9] preventing proliferation of microorgamisms, [10] killing the bacteria, [2] increasing the pH of dentin, [2,11-13] causing necrosis of resorptive cells present in Howship’s lacunae, [10] inhibiting the osteoclastic acid hydrolases, [2] and activating alkaline phosphatases. [2,9]
We used glass ionomer cement to temporize the tooth, as it can prevent bacterial penetration to the periapex of root-filled teeth over a 1 month period. [11] While obturation, we used resin sealer with MTA, as it not only have good radiopacity, better flow, high pH, short setting time and lower water absorption, but also produced less inflammatory reaction and demonstrate the superior biocompatibility that can stimulate tissue mineralization. [12,13] In present case, obturation was done with lateral condensation technique because it provides better length control than the other obturation techniques. [6]
After completing the obturation, we closed the access opening with composite resin filling material and we chose not to place a fixed prosthesis, because the extra-coronal crown preparation combined with endodontic access preparation significantly weakens the cervical area of the anterior teeth. [14] Follow-up radiographs were taken after 6 months, and another one after 1 year interval, because healing of teeth with periapical lesion is most marked from 3 months to 2 years. [15]
Conclusion
All extensive periradicular lesions with external root resorption don’t need surgical intervention. Teeth with extensive lesions and inflammatory root resorptions can be successfully managed by nonsurgical root canal treatment, using suitable materials such as MTA Fillapex, and monitory follow-up.
Conflict of Interests
The authors declare that they have no conflict of interest.
REFERENCES
- Bansal P, Nikhil V, Kapur S. Multiple idiopathic external apical root resorption: A rare case report. J Conserv Dent. 2015;18:70-72.
- Gilda AJ, Thomasnainan M, Kamat S, Mangala TM. External apical root resorption: Two case reports. IntEndod J. 2009;21:75-79.
- Fuss Z, Tsesis I, Lin S. Root resorption diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol. 2003;19:175-182.
- Ghorbanzadeh S, Ashraf H, Hosseinpour S, Ghorbanzadeh F. Nonsurgical management of a large periapical lesion: A case report. Iran Endod J.2017;12:253-256.
- Saatchi M. Healing of large periapical lesion: A non‐surgical endodontic treatment approach. Aust Dent J. 2007;33:136-140.
- Hargreaves KM, Berman LH. Cohen's Pathways of the Pulp. (11th ed.). St. Louis, MO: Elsevier. 2016.
- Siqueira JF Jr, Rôças IN, Favieri A, Lima KC. Chemo mechanical reduction of the bacterial population in the root canal after instrumentation and irrigation with 1%, 2.5%, and 5.25% sodium hypochlorite. J Endod. 2000;26:331-334.
- Estrela C, Estrela CRA, Barbin EL, Spano J, Marchesan M, Pecora J. Mechanism of action of sodium hypochlorite. Braz Dent J. 2002;13:113-117.
- Şen BH, Wesselink PR, Türkün M. The smear layer: A phenomenon in root canal therapy. IntEndod J.1995;28:141-148.
- Machado R, Chrun ES, Tomazinho LF, Garcia LFR. Endoodntic treatment of a toot with pulp necrosis and severe inflammatory external apical root resorption in a single session: Is it possible? A case report. J Endod. 2017;28:28-31.
- Barthel CR, Strobach A, Briedigkeit H, Gobel UB, Roulet JF. Leakage in roots coronally sealed with different temporary fillings. JEndod.1999;25:731-734.
- Gomes-Filho JD, Watanabe S, Cintra LTA, Nery MJ, Dezan-Junior E, Queiroz IOA, et al. Effect of MTA-based sealer on the healing of periapical lesions. J Appl Oral Sci. 2013;21:235-242.
- Shakya VK, Gupta P, Tikku AP, Pathak AK, Chandra A, Yadav RK, et al. An invitro evaluation of antimicrobial efficacy and flow characteristics for AH Plus, MTA Fillapex, CRCS and gutta flow 2 root canal sealer. J ClinDiagn Res.2016;10:104 -108.
- McComb D. Restoration of the endodontically treated tooth. Royal college of dental surgeons of Ontario. Practice Enhance Knowl. 2008;22:1-20.
- Huumonen S, Ørstavik D. Radiographic follow-up of periapical status after endodontic treatment of teeth with and without apical periodontitis. Clin Oral Investig. 2013;17:2099-2104.






 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.