A Prospective Study of Spectrum, Risk Factors and Immediate Outcome of Congenital Anomalies in Bida, North Central Nigeria
- *Corresponding Author:
- Dr. Adeboye MAN
Department of Pediatrics, College of Health Sciences, University of Ilorin Teaching Hospital, PMB 1459, Ilorin, Kwara State, Nigeria.
E-mail: adeboyeman@yahoo.co.uk
This is an open access article distributed under the terms of the Creative Commons Attribution�Non Commercial�Share Alike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Background: Congenital disorders are structural, metabolic, behavioral and functional disorders that are present at birth. Their manifestations are protean ranging from mild anomalies to life‑threatening conditions. Aim: The objectives of this study were to describe the congenital anomalies in children seen at Federal Medical Center, Bida over a 12 month period, determine possible factors associated with these anomalies; and their short term outcome. Subjects and Methods: Children with clinically recognized congenital malformations were recruited consecutively over a 12 month period and socio‑demographic, etiologic and other relevant clinical data were obtained. A detailed examination was also performed and abnormalities documented. The data was analyzed using Epi‑info version 6 (Atlanta, USA). The Chi‑square was used to identify significant differences for categorical variables. Mid‑P and Fisher’s exact tests were utilized as appropriate. A P < 0.05 was considered to be significant. Results: A total of 46 children with congenital anomalies were seen during the study period, all which were recruited into the study. The hospital based prevalence amongst neonates was 111/1000 neonates. The most common system affected was the digestive system (50.0%) followed by the central nervous system and head and neck anomalies. There was no significant difference in distribution of anomalies amongst the various ethnic groups. About 22% of families were consanguineous, all being first cousins and 8.7% of mothers were greater than 35 years of age. The case fatality rate for congenital malformations was 2.2%, while 60.9% were referred to other hospitals for further care. Conclusion: The study has demonstrated a wide variety of congenital anomalies in Bida, North‑Central Nigeria with the digestive system anomalies being the most frequent. The findings of this study strengthen the need for empowerment of the institution in appropriate management of these disorders.
Keywords
Anomalies, Bida, Congenital malformations
Introduction
Congenital disorders are structural, metabolic, behavioral and functional disorders that are present at birth; [1] however, manifestations of some of these disorders may not be obvious until later childhood or in adulthood. These comprise the various categories of disruptions, malformations, deformations and association syndromes. [1,2] These disorders frequently result from genetic abnormalities and insults to the developing fetus. About 2-3% of births are associated with major congenital anomalies diagnosed at or soon after birth. [1] An additional 2-3% are recognized by the age of 5 years. [1] Dastgiri et al. [3] in Glasgow in an 18 year review of congenital anomalies reported prevalence of 324/10,000 births, most common of which were congenital heart diseases, anomalies of the limbs and digestive system anomalies. In Canada, 2-3% of the 350,000 babies born each year will be delivered with a serious congenital anomaly. [4] Tomatir et al. [5] in Turkey reported prevalence of 2.9/1000 live births with central nervous system anomalies being the most common, followed by cleft lip and palate and musculoskeletal anomalies.
The varying prevalence of these disorders may be explained by racial, ethnic, sociocultural and economic differences between the various countries. In Nigeria, there is a dearth of local data on the incidence of these anomalies. Sunday-Adeoye et al. [6] in Delta state, Nigeria in a retrospective study reported incidence of external congenital anomalies of 110.8/10,000 live births. Musculoskeletal system anomalies were the most common followed by central nervous system anomalies. [6] The single most common anomaly described was ulnar polydactyly. [6] Furthermore, they found that twin gestations were associated with a significantly higher incidence of congenital anomalies compared with singleton pregnancies. [6] Bakare et al. [7] in South Western Nigeria in a prospective study of external birth defects in neonates reported incidence of 6.9%. Musculoskeletal disorders were the most prevalent seen in 3.5% of the newborns studied, followed by external genitalia abnormalities (1.4%), head abnormalities (1.3%) and abdominal defects in 1.1% of the newborns studied. Recognized risk factors include but not limited to poverty, consanguinity, ethnicity, advanced maternal age and maternal illiteracy. [8]
The absence of a comprehensive study on both internal and external congenital anomalies forms the justification for this prospective study which aims to describe the spectrum, distribution and demographic characteristics of congenital anomalies in children seen at Federal Medical Centre, Bida over a 12 month period (September 2009-August 2010); and to determine possible factors associated with these anomalies; and their short term outcome.
Subjects and Methods
The study was a prospective descriptive study carried out over a period of 12 month from September 2009 to August 2010. The study was carried out at the pediatric wards, neonatal unit and outpatient clinics of the Federal Medical Center, Bida. The hospital is a tertiary medical center, located in Bida in Niger State and serves as a referral center for most of Niger State and some surrounding states. All patients with clinically recognized congenital malformations seen at the hospital were recruited into the study. Informed consent was obtained from parents of all the subjects, according to standard ethical practice. Ethical clearance was obtained from the ethical review committee of the hospital.
Socio-demographic characteristics, such as, age, social status, family type and size, ethnic group and area of residence were recorded. Information was also obtained on common risk factors, including consanguinity and exposure to radiation. A detailed examination was performed to document all abnormalities by the team of researchers and immediate outcome measures were determined. The anomalies were grouped according to organ systems and where multiple anomalies were present; records were duplicated in the systems affected. The data was analyzed using Epi-info version 6 (Atlanta, USA). Frequency distribution tables and cross-tabulation of variables were generated. Measures of central tendency and dispersion of quantitative variables, as well as proportion and percentages for qualitative variables were also determined. The Chi-square was used to identify significant differences for categorical variables. Mid-P and Fisher’s exact tests were utilized as appropriate. Mean, standard deviations and range were provided as appropriate. Confidence intervals were calculated for the various risk factors. A P < 0.05 was considered to be significant.
Results
A total of 46 children with congenital anomalies were seen during the study period, all of which were recruited into the study. The mean (SD) age was 21 (81.3) days and ranged from 1 day to 16 months. There were 27 males and 19 females with a male:female of 1.4:1. Most 67.4% (31/46) of the children studied were of the Nupe ethnic group. A majority 78.3% (36/46) of the children belonged to families of low socio-economic status. Table 1 shows the socio-demographic characteristics of the children studied.
| Characteristic | Frequency | Percentage |
|---|---|---|
| Age | ||
| <24 h | 23 | 50.0 |
| 2-6 days | 17 | 37 |
| 1-4 weeks | 4 | 8.7 |
| 1-12 months | 1 | 2.2 |
| >1 year | 1 | 2.2 |
| Gender | ||
| Male | 27 | 58.7 |
| Female | 19 | 41.3 |
| Ethnic group | ||
| Nupe | 31 | 67.4 |
| Fulani | 5 | 10.9 |
| Hausa | 2 | 4.3 |
| Gwari | 2 | 4.3 |
| Ibo | 2 | 4.3 |
| Others | 4 | 8.7 |
| Social class | ||
| High | 4 | 8.7 |
| Middle | 6 | 13.0 |
| Low | 36 | 78.3 |
| Systems affected* | ||
| Digestive system | 23 | 50.0 |
| Musculoskeletal system | 8 | 17.4 |
| Central nervous system | 8 | 17.4 |
| Genitourinary | 5 | 10.9 |
| Head and neck | 6 | 13.0 |
| Cardiovascular system | 3 | 6.5 |
| Down syndrome | 1 | 2.2 |
*Seven patients had major anomalies in more than one system
Table 1: Socio-demographic characteristics and pattern of major anomalies of the children
A total of 44 of the patients belonged to the neonatal age group. A total of 396 neonates were seen/admitted in the neonatal unit over the 1 year study period giving a hospital based prevalence of 111/1000 neonates admitted. The most common 50.0% (23/46) group of congenital anomalies seen was digestive system anomalies. The digestive system anomalies were imperforate anus 52.2% (12/23), omphalocele major 34.8% (8/23), omphalocele minor 8.7% (2/23) and gastroschisis 4.3% (1/23). The least affected 6.5% (3/46) system was the cardiovascular system while a suspected chromosomal anomaly (Down syndrome) was seen in only one child [Table 1].
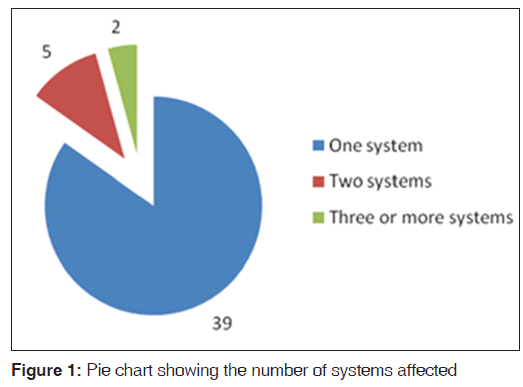
The most common system affected amongst both male and female children was the digestive system [Table 2], followed by the central nervous system among males and head and neck anomalies among the females. There was no significant difference in the distribution of the systems affected amongst both male and female children. Most of the patients had only one system affected, however seven patients had affectation of two or more systems [Figure 1]. Table 3 shows the distribution of selected risk factors amongst the children. About 22% (10/46) of families were consanguineous, all being first cousins and 8.7% (4/46) of mothers were greater than 35 years of age. There was no history of congenital anomalies in the first degree relatives of all the children studied. There was no significant difference between proportions of congenital anomalies amongst children of low and high socio-economic status [Table 4].
| System affected | Male (%) | Female (%) | Frequency (%) | P |
|---|---|---|---|---|
| Digestive | 13 (56.5) | 10 (43.5) | 23 (100) | 0.76 |
| system | ||||
| Musculoskeletal | 4 (50.0) | 4 (50.0) | 8 (100) | 0.87 |
| system | ||||
| Central nervous | 7 (87.5) | 1 (12.5) | 8 (100) | 0.15 |
| system | ||||
| Genitourinary | 4 (80.0) | 1 (20.0) | 5 (100) | 0.60 |
| Head and neck | 1 (16.7) | 5 (83.3) | 6 (100) | 0.07 |
| Cardiovascular | 2 (66.7) | 1 (33.3) | 3 (100) | 0.99 |
| system | ||||
| Down | 0 | 1 (100) | 1 (100) | 0.99 |
| syndrome |
Table 2: Gender distribution of congenital anomalies
The distribution of the major congenital anomalies in relation to maternal ethnic group is as shown in Table 3. There was no significant difference in frequencies of digestive, central nervous and musculoskeletal anomalies between Nupes and the other ethnic groups taken as one. During the period of the review, only one patient died giving a case fatality rate from congenital anomalies of 2.2% (1/46). This patient had multiple anomalies in the musculoskeletal system (polydactyly), central nervous system (congenital cataracts, plagiocephaly) and urogenital system (bilateral undescended testes, hypospadias with micropenis). A majority 60.9% (28/46) of the patients seen were referred to other hospitals as a result of a lack of personnel and/or facilities for managing these conditions. Three of the patients departed against medical advice. Of the 14 patients that were managed successfully and discharged, only 50% (7/46) were seen subsequently seen at a follow-up clinic.
| System | Nupe | Others | χ2 | P |
|---|---|---|---|---|
| Digestive system | ||||
| Digestive system | 14 | 9 | 0.89 | 0.35 |
| Other system | 17 | 6 | ||
| Central nervous system | 6 | 2 | 0.2551 | 0.66* |
| Other system | 25 | 13 | ||
| Musculoskeletal system | ||||
| Musculoskeletal system | 7 | 1 | 1.782 | 0.21* |
| Other system | 24 | 14 | ||
| *Mid-P exact |
*Mid-P exact
Table 3: Ethnic distribution of the most frequent anomalies
| Risk factor | Yes | No | 95% CI |
|---|---|---|---|
| Maternal age >35 years | 4 (8.7) | 42 (91.3) | 2.82-19.65 |
| Maternal alcohol | 0 (0.0) | 46 (100.0) | 0.00-6.31 |
| consumption | |||
| Maternal cigarette | 1 (2.2) | 45 (97.8) | 0.11-10.26 |
| smoking | |||
| Family history of | 0 (0.0) | 46 (100.0) | 0.00-6.31 |
| congenital anomaly | |||
| Polygamous family setup | 19 (41.3) | 27 (58.7) | 27.82-55.86 |
| Exposure to X-rays in | 0 (0.0) | 46 (100.0) | 0.00-6.31 |
| pregnancy | |||
| Consanguinity | 10 (21.7) | 36 (78.3) | 11.6-35.34 |
| Low socio-economic | 36 (78.3) | 10 (21.7) | 64.66-88.4 |
| status |
CI: Confidence interval
Table 4: Distribution of selected socio-demographic factors and risk factors for congenital anomalies
Discussion
Congenital anomalies are a common cause of morbidity and mortality world-wide. [9] The degree of disability may be determined by the system affected, the severity of anomalies, adequacy of healthcare/support services and cost. [9,10] The most frequently affected system in this study was the digestive system, followed by the central nervous system and musculoskeletal system. This is similar to the findings of Ekwere et al. [11] in Jos, North-Central Nigeria where gastrointestinal anomalies were most frequently seen however, is different from the reports from Bakare et al. [7] in Southwestern Nigeria. This may be related to sociocultural similarities between the current study site and Jos, both in North-Central Nigeria. It may also be attributable to the fact that congenital anomalies affecting the gastrointestinal system will often present early with disruption in function such as intestinal obstruction, persistent vomiting or choking episodes prompting early presentation. The influence of sociocultural factors in congenital anomalies has been described previously by several authors. [12,13] Another possible contributory factor is the effect of poverty and illiteracy in this study as parents of children with non-life-threatening musculoskeletal anomalies may not present at hospital unless complications arise. This is supported by the higher mean age at presentation for musculoskeletal anomalies compared to the digestive system anomalies. Central nervous system, genitourinary and cardiovascular anomalies were more common in males than females while head and neck anomalies (largely cleft lip and palate) were commoner in females. However, the differences were not statistically significant. This is similar to reports by Tomatir et al. [5] in Turkey.
In this study, about 22% of parents were consanguineous, with all being first cousins. This reflects the practice of consanguineous marriages amongst the Nupe ethnic group. [14] Though the study design did not allow a determination of significance of the consanguinity, it is similar to about 15% reported by Tomatir et al. [5] Maternal age plays an important role in the etiology of congenital anomalies, especially in relation to chromosomal disorders. [1,2,4] Maternal age greater than 35 years is associated with increased risk of chromosomal disorders, such as Down syndrome. [1,2,4] This is supported by the finding in this study that the mother of the only child with a suspected chromosomal disorder (Down syndrome) was greater than 35 years of age. However, it is likely that if chromosomal studies were performed in all the patients, a significant number of genetic abnormalities may have been detected. Cigarette smoking was not a significant contributor to congenital anomalies in this study as only one mother smoked cigarettes in this study. This is probably related to the negative cultural view of women smoking in a typical Nigerian community. Interestingly, in this study, socio-economic status did not appear to have a significant impact on distribution of congenital anomalies; however, the obvious limitation of the study design without a control group limits the significance of this observation. Olesen et al. [13] in Denmark and Azimi and Lotfi [15] in Iran found socio-economic status and particularly maternal educational status to have a significant impact on the occurrence of congenital anomalies. This is contrary to the findings of Varela et al. [12] in Spain who found no such significant relationship. Further studies would be required in this environment to examine the impact of this risk factor.
The mortality rate amongst patients with congenital anomalies was low at 2.2%. This is much lower than 14.7% in Turkey. [5] However, it is important to note that over 60% of patients were referred to other hospitals, another seven were lost to follow-up following discharge and three were discharged from care against medical advice. Thus, the overall mortality may probably be higher than the derived figure.
Conclusion
The study has demonstrated a wide variety of congenital anomalies in Bida, North-Central Nigeria with the digestive system anomalies being the most frequent. The findings of this study suggest the necessity for a support for the families of children with these disorders so that problems especially - financial and social may be anticipated and prompt and appropriate support instituted. Early detection would facilitate early counseling, such that parents are aware and prepared for the challenges of a child with a congenital anomaly. The burden of congenital anomalies in this study (111/1000 neonatal admissions) emphasizes the need to develop local capacity in institutions with similar statistics of congenital anomalies in terms of manpower and equipment for the management of these disorders.
A limitation of the study includes no active search for hidden congenital anomalies or inborn errors of metabolism.
Financial support and sponsorshipNil.
Conflicts of interest
There are no conflicts of interest.
References
- Sadler TW. Birth defects and prenatal diagnosis. In: Sadler TW, editor. Langman’s Medical Embryology. 9th ed. Philadelphia: Lippincott Williams and Wilkins; 2004. p. 149-68.
- Wynshaw-Boris A, Biesecker LG. Dysmorphology. In: Kliegman RM, Behrman RE, Jenson HB, Stanton BF, editors. Nelson’s Textbook of Pediatrics. 18th ed. Philadelphia: Saunders Elsevier; 2007.
- Dastgiri S, Stone DH, Le-Ha C, Gilmour WH. Prevalence andsecular trend of congenital anomalies in Glasgow, UK. Arch Dis Child 2002;86:257-63.
- Lowry RB. Introduction to congenital anomalies. In: Lowry RB,editor. Congenital Anomalies in Canada: A Perinatal Health Report 2002. 1st ed. Ottawa: Minister of Public Works and Government Services Canada; 2002. p. xi-xvii.
- Tomatir AG, Demirhan H, Sorkun HC, Köksal A, Ozerdem F, Cilengir N. Major congenital anomalies: A five-year retrospective regional study in Turkey. Genet Mol Res 2009;8:19-27.
- Sunday-Adeoye I, Okonta PI, Egwuatu VE. Congenital malformations in singleton and twin births in rural Nigeria. Niger Postgrad Med J 2007;14:277-80.
- Bakare TI, Sowande OA, Adejuyigbe OO, Chinda JY, Usang UE. Epidemiology of external birth defects in neonates in Southwestern Nigeria. Afr J Paediatr Surg 2009;6:28-30.
- Sheridan E, Wright J, Small N, Corry PC, Oddie S, Whibley C, et al. Risk factors for congenital anomaly in a multiethnic birthcohort: An analysis of the Born in Bradford study. Lancet 2013; http://dx.doi.org/10.1016/S0140-6736(13)61132-0.
- Dastgiri S, Gilmour WH, Stone DH. Survival of children born with congenital anomalies. Arch Dis Child 2003;88:391-4.
- Rosano A, Botto LD, Botting B, Mastroiacovo P. Infant mortality and congenital anomalies from 1950 to 1994: An international perspective. J Epidemiol Community Health 2000;54:660-6.
- Ekwere OE, Mcneil R, Agim BP, Jeminiwa B, Oni O, Pam S. A retrospective study of congenital anomalies presented at tertiary health facilities in Jos, Nigeria. J Phys Chem Solids 2011;3:24-8.
- Varela MM, Nohr EA, Llopis-González A, Andersen AM, Olsen J. Socio-occupational status and congenital anomalies. Eur J Public Health 2009;19:161-7.
- Olesen C, Thrane N, Rønholt AM, Olsen J, Henriksen TB. Association between social position and congenital anomalies: A population-based study among 19,874 Danish women. Scand J Public Health 2009;37:246-51.
- Nadel SF. Morality and language among the nupe. Man1954;54:55-7.
- Azimi C, Lotfi M. Association of socioeconomic status and fetal congenital abnormalities. Am J Sci Res 2012;58:148-54.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.