A Type‑II First Branchial Cleft Anomaly Presenting as a Post‑Auricular Salivary Fistula: A Rare Presentation
- *Corresponding Author:
- Dr. Shraddha Jain
Department of Otorhinolaryngology and Head and Neck Surgery, Jawahar Lal Nehru Medical College, DMIMSU, Sawangi, Wardha, Maharashtra, India.
E-mail: sjain_med@yahoo.co.in
Abstract
First branchial cleft anomalies are rare with the average age of presentation as 19 years. There is an average delay of 3.5 years between initial presentation and adequate treatment due to diagnostic dilemma. A very rare variant of first branchial cleft anomaly presenting as a post‑auricular salivary fistula is reported. A 12‑year‑old girl presented with a history of intermittent watery discharge, more so at the time of meals from a right post‑auricular opening for last 3 years. Computed tomography sialography revealed a fistulous tract connecting the sub segmental duct of the parotid gland extending along the pre‑tragus region in subcutaneous plane up to mastoid tip after passing inferior to external auditory canal. Superficial parotidectomy with identification of facial nerve branches was carried out for excision of the tract. Histopathology revealed sinus tract comprising of ectodermal components and acini of the parotid gland. We classified our case into work’s type‑2 based on anatomical location at an angle of mandible, its relationship to parotid gland and facial nerve and previous history of ear discharge. To the best of our knowledge, this is the first case of its type to be reported.
Keywords
Branchial cleft fistula, First branchial anomaly, Salivary fistula
Introduction
First branchial cleft anomalies are rare accounting for <8% of all branchial anomalies.[1] The average age of presentation is 19 years with an average delay of 3.5 years between initial presentation and adequate treatment due to diagnostic dilemma.[2] The spectrum of first branchial cleft anomalies includes cysts, sinuses, and fistulas, and various combinations of these entities. The usual site of presentation is in the lateral neck below the external ear canals, above the hyoid bones. They are twice more common in women as compared to men with the left side predominance for fistulas.[2]
Here, we report an extremely rare variant of first branchial cleft anomaly of type-2 presenting as a salivary fistula near mastoid tip in a young female patient. To the best of our knowledge, this is probably the first case of this type to be reported.
Case Report
A 12-year-old female presented to Otolaryngology Department of our hospital with a history of intermittent watery discharge at the time of meals from an opening behind her right ear for last 3 years. It began with a swelling behind the ear with intermittent pus discharge from the right ear. After some days, the post-auricular swelling spontaneously ruptured with pus discharge. The same site was then marked by a persistent small opening in the skin which discharged clear fluid intermittently, more at the time of meals. The ear discharge stopped, once the discharge began from the post-auricular region. There was no history of purulent discharge from the opening. She denied any history of trauma, hearing loss or any other swelling. On examination, there was a small cutaneous opening near mastoid tip behind the ear lobule, which discharged clear fluid (saliva) on pressing the parotid gland [Figure 1]. External auditory canal and tympanic membrane were normal. Audiological tests were normal.
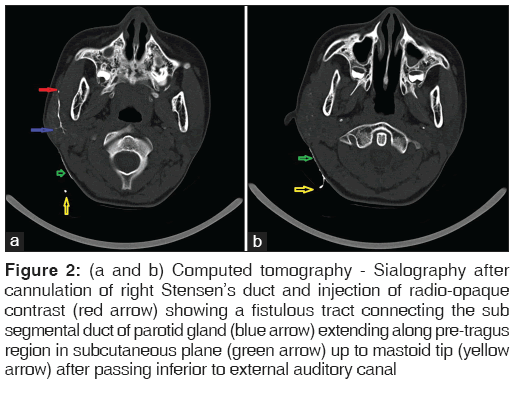
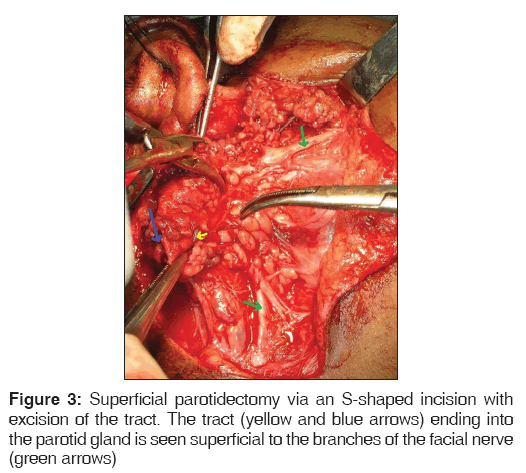
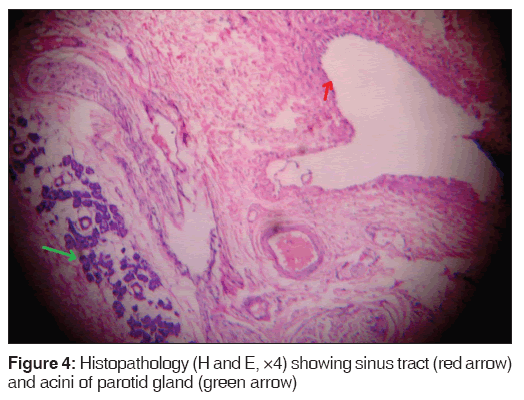
Computed tomography (CT) sialography carried out after cannulation of right Stensen’s duct and injection of radio-opaque contrast revealed a fistulous tract connecting the sub segmental duct of the parotid gland extending along the pre-tragus region in subcutaneous plane up to mastoid tip after passing inferior to external auditory canal [Figure 2a and b]. The patient underwent superficial parotidectomy through an S-shaped incision with excision of the tract. The tract was superficial to the branches of the facial nerve and ended into the parotid gland [Figure 3]. The facial nerve branches were completely visualized and preserved. Histopathology revealed sinus tract comprising of ectodermal components and acini of the parotid gland [Figure 4].
Figure 2: (a and b) Computed tomography - Sialography after cannulation of right Stensen’s duct and injection of radio-opaque contrast (red arrow) showing a fistulous tract connecting the sub segmental duct of parotid gland (blue arrow) extending along pre-tragus region in subcutaneous plane (green arrow) up to mastoid tip (yellow arrow) after passing inferior to external auditory canal
Discussion
Anomalies of the first branchial cleft result from duplication of membranous external auditory canal. First branchial cleft is unique in being the only cleft that does not become obliterated completely.[3] The dorsal portion of the first branchial cleft deepens to form the external auditory meatus, whereas the ventral portion disappears. Incomplete closure of the ventral portions of the first branchial cleft or buried ectodermal cell rests is said to result in first branchial cleft anomalies. During development, closure of the clefts is concurrent with both; the emergence of the developing parotid gland, which appears as an ectodermal ingrowth of local surface ectoderm of the mouth, extending into adjacent mesenchyme, and with migration of the facial nerve, which originates from the second branchial arch. Hence, first branchial cleft anomalies are closely related to these structures.[4]
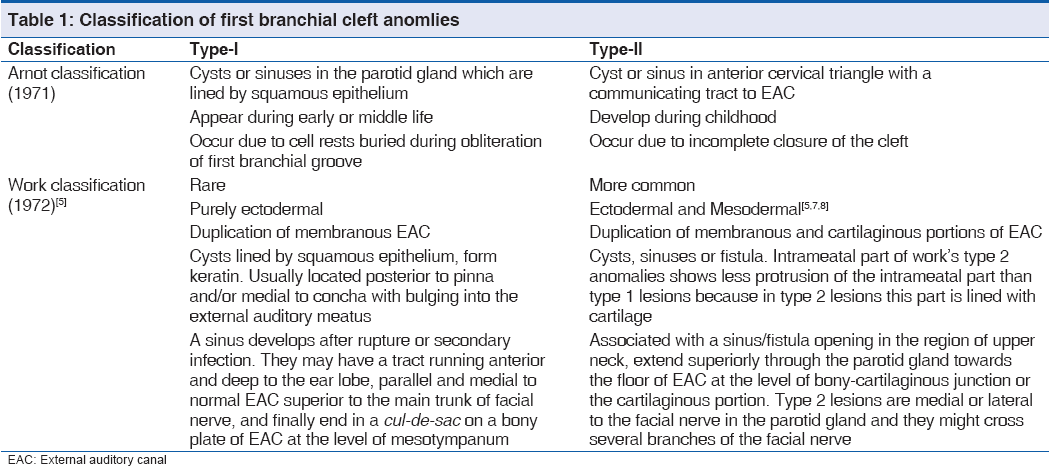
Various confusing classifications have been proposed for first branchial cleft anomalies. The extreme rarity of this condition and the occurrence of variants are responsible for this confusion. There are two main types of first branchial cleft anomalies – type-1 and type-2 on the basis of anatomical location proposed by Arnot (1971) and both location and histology by work (1972) [Table 1]. Olsen et al. (1980) classified the first branchial cleft anomalies into cysts, sinuses or fistulas of the post-auricular region, lobule, canal or angle of the jaw to avoid confusion.[3] Arnot’s type-1 lesions included cysts or sinuses in the parotid gland, whereas type-2 were found between upper neck and external auditory canal (EAC).[3] Work’s type 1 lesions were adjacent to the EAC, whereas type 2 were in the upper neck near the angle of the mandible.[4,5] Type-1 lesions of work occur medial to concha and frequently extend to the post-auricular crease or supra-auricular region.[5,6] They are superior to the main trunk of the facial nerve in contrast to type 2 lesions, which pass through parotid gland and have close, but variable relationship to the facial nerve. Embryologically, it appears that the point of time at which the disorder developed dictates whether the malformation is of type 1 or 2. We classified our case into work’s type-2 based on the anatomical location at angle of mandible, its relationship to parotid gland and facial nerve and previous history of ear discharge.
Different clinical presentations have been described for type-2 first branchial cleft anomaly, which include chronic purulent discharge from the ear with sinus opening in the ear canal floor, peri-auricular cysts or swelling in the parotid area that increase in size during an inflammatory period, and abscess or persistent fistula in the neck located above a horizontal plane passing through the hyoid bone, anterior to the sternocleidomastoid muscle, in the Poncet’s triangle.[7,8] The location in neck is variable from submandibular region in front of the auricle to retro-infra-auricular region as in our case. A membranous attachment between the floor of the EAC and the tympanic membrane is also observed in few cases.[7-9] Rare variants have been described with fistulous opening in lateral nasopharyngeal wall anterior to fossa of rosenmuller.[10] In our patient, there was prior history of ear discharge, which stopped once the swelling ruptured and started draining clear fluid. There was no fistulous opening in the floor of EAC of our patient and at the time of surgery only a single tract was found away from the cartilage of EAC ending superficially into parotid tissue. There must have been two tracts initially, one of which must have undergone fibrosis leading to stoppage of ear discharge. Association of type-2 first branchial cleft lesions with parotid gland is well-known, but first branchial cleft anomaly presenting with communication with sub segmental parotid duct has probably not been previously described.
The sinus tract in case of type-2 first branchial cleft anomaly runs through the parotid gland with variable relationship between the tract and the facial nerve,[8] The fistulous tracts are more likely to lie deep to the facial nerve compared to sinus tracts. Lesions with openings in the external auditory meatus have been found to be associated with a tract superficial to the facial nerve.[11] Rarely, the tract may go in between the branches of the facial nerve.
The occurrence of such high variability in the course of these lesions leads to complications such as facial nerve injury during the surgery and recurrence following incomplete excision due to failure to identify the variable course of the sinus or fistula tract. Hence, radiographic visualization is extremely crucial in planning surgery. Very few reports mention the radiographic analyses of first branchial cleft anomalies with role of CT fistulography.[4,6] We found CT sialography highly useful in identifying the variant of first branchial cleft anomaly in our patient. So, CT fistulography should be the imaging modality of choice for sinuses or fistulas of peri-auricular region.
We broadly agree with work classification, but suggest a slight modification considering the existing confusion as it may be helpful in management. Arnot’s type-1 lesions were found in parotid and both Arnot and work emphasized on fistulous tract opening in EAC in type-2 lesions. We suggest that the classification be carried out on the basis of imaging. In case, they are related to the parotid gland and facial nerve, they should be labeled as type-2 irrespective of the location of sinus or fistulous opening-post-auricular or cervical. The communication with EAC may or may not be present in type-2 lesions. The surgical exposure in such cases will require parotidectomy incision and superficial parotidectomy for identification and preservation of facial nerve where needed. Rest peri-auricular lesions including cysts, sinuses of concha, pinna, and fistulas of peri-auricular region, which open in middle-ear cavity should be labeled as type-1. Simple excision of the sinus tract with cuff of ear cartilage may be adequate for most type-1 first branchial cleft lesions due to their peri-auricular location with the tract passing superior to facial nerve parallel to external auditory canal. Type-1 anomalies may be associated with other congenital anomalies such as microtia and canal atresia, though this association is extremely rare and should be differentiated from acquired sinuses or fistulae.[6,12,13] The articles don’t mention that it was type-1 anomaly, but their description matches work’s type-1. Further research is needed in this highly debatable issue.
Conclusion
Since, first branchial cleft anomalies are usually not associated with other facial malformations; it could be difficult to recognize them leading to wrong diagnosis and treatment. A careful history, a thorough ontological examination and CT/Magnetic Resonance Imaging with/without CT-fistulography should be carried out in every case of peri-auricular swelling, cysts, sinuses or fistulas. Superficial parotidectomy may be required for most type-2 branchial cleft sinuses or fistulas.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Ku WY, Wang KJ, Jou YL, Chang YH, Chou CS. Type II first branchial cleft anomaly: A case report. Tzu Chi Med J 2005;17:357-60.
- D’Souza AR, Uppal HS, De R, Zeitoun H. Updating concepts of first branchial cleft defects: A literature review. Int J Pediatr torhinolaryngol 2002;62:103-9.
- Olsen KD, Maragos NE, Weiland LH. First branchial cleft anomalies. Laryngoscope 1980;90:423-36.
- Whetstone J, Branstetter BF 4th, Hirsch BE. Fluoroscopic and CT fistulography of the first branchial cleft. AJNR Am J Neuroradiol 2006;27:1817-9.
- Work WP. Newer concepts of first branchial cleft defects.Laryngoscope 1972;82:1581-93.
- Jain S, Kumar S, Deshmukh PT, Yohannan D, Sudarshan K. Congenital aural stenosis with first branchial cleft fistula, presenting with recurrent facial nerve palsy, in an elderly patient. J Clin Gerontol Geriatr 2012;3:42-4.
- Triglia JM, Nicollas R, Ducroz V, Koltai PJ, Garabedian EN. First branchial cleft anomalies: A study of 39 cases and a review of the literature. Arch Otolaryngol Head Neck Surg 1998;124:291-5.
- Tham YS, Low WK. First branchial cleft anomalies have relevance in otology and more. Ann Acad Med Singapore 2005;34:335-8.
- Ebelhar AJ, Potts K. An unusual otoscopic finding associated with a type II first branchial cleft anomaly. J Laryngol Otol 2012;126:316-8.
- Ramnani S, Mungutwar V, Goyal NK, Bansal A. A rare variant of first branchial cleft fistula. J Laryngol Otol 2009;123:1387-9.
- Solares CA, Chan J, Koltai PJ. Anatomical variations of the facial nerve in first branchial cleft anomalies. Arch Otolaryngol Head Neck Surg 2003;129:351-5.
- Yalçin S, Karlida? T, Kaygusuz I, Demirba? E. First branchial cleft sinus presenting with cholesteatoma and external auditory canal atresia. Int J Pediatr Otorhinolaryngol 2003;67:811-4.
- Blevins NH, Byahatti SV, Karmody CS. External auditory canal duplication anomalies associated with congenital aural atresia. J Laryngol Otol 2003;117:32-8.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.