Acid Base Electrolyte Imbalance and Survival Outcome of Low Glasgow Coma Scale (GCS) patients in the Medical Intensive Care Unit
2 Minimally Invasive Section, Department of surgical Oncology, King Fahad Medical City, Riyadh, Saudi Arabia
3 Department of Pediatrics, Pioneer Hospital, Ramanathapuram, India
4 Department of Surgery, Ibn Sina hospital, Kuwait
5 Department of Surgery, Saveetha Medical College, Chennai, India
6 Department of Pulmonary and critical care, King Fahad Medical City, Riyadh, KSA
Citation: Buhary B, et al. Acid Base Electrolyte Imbalance and Survival Outcome of Low Glasgow Coma Scale (GCS) patients in the Medical Intensive Care Unit. Ann Med Health Sci Res. 2017; 7: 10-15
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Acid-base and electrolytes disorders are commonly seen in critically ill patients. Electrolyte abnormalities were the most frequent extra cranial occurrence of altered consciousness. There are multiple studies which reported altered survival outcome in low GCS patient and some did not. Aims: To assess the survival outcome of acid-base electrolyte imbalance associated with low GCS patients in the medical ICU. Methods: This retrospective, cohort study conducted in the medical ICU of a tertiary center in Chennai, India, for a period of six months included patients above 18 years old with various acid-base and electrolyte imbalances. During the study period of six months, a total of 276 patients were admitted in the medical ICU. Among these 100 patients were included in the study after excluding the patients who didn’t meet the inclusion criteria and those that had incomplete medical records. Following data were collected from medical records admission history, age, sex, anion gap, serum electrolytes, ABG, BUN, creatinine, PCO2, PO2, GCS and days in ICU. Results were analyzed and outcomes were noted (patient discharged, dies or seeks discharge against medical advice). Results: The study population included 68 male and 32 female with a mean age of 47.24±17.54 years. Metabolic acidosis was seen in 67% of patients. Mortality was significantly higher in patients with low GCS (51.06% vs. 20.75%, p<0.0001). Sodium and chloride increased significantly (p=0.0126, 0.0464 respectively) and potassium decreased significantly (p=0.0008) when GCS was low. The patients with hypernatremia and metabolic acidosis had 71.44% mortality rate. The patients with a low GCS have a higher incidence for multiple electrolyte disturbances. Low GCS leads mostly to an increased mortality especially in the patients with acid base disorders with electrolyte disorders compared to those with pure acid-base disturbances. To identify prognostic factors of the patients in the ICU, we performed multiple regression analysis using the data we collected. Among all the variables only three independent factors (GCS, BUN and Creatinine) significantly correlated with the criterion. Conclusions: Electrolyte and acid base disturbances should be seriously considered in low GCS patients to allow timely and appropriate therapeutic intervention to improve survival outcome.
Keywords
p>Acid base disorder; Anion gap; Electrolyte imbalance; GCS; ICUKey Message
Acid base disorders and electrolyte imbalance are the primary contribution to mortality in the ICU. A crucial issue in these disorders is predicting its outcome when GCS is low. It was found that survival outcome of acid base electrolyte patients is based on GCS.
Introduction
Acid-base and electrolytes disorders are commonly seen in critically ill patients. Acid base disturbances cause blood pH to shift away from normal range when renal or respiratory function is abnormal or when an acid/base load overwhelms excretory capacity. This evokes compensatory responses by the body that returns pH toward near normal to maintain the PCO2/ [HCO3] ratio. [1-3] A drop or rise in PCO2 will result in a drop or rise in hydrogen respectively. The HCO3/ PCO2 relationship in extracellular fluids is useful in classifying disorders of acid base balance namely acidosis due to gain of acid or loss of alkali, i.e., fall in HCO3/ PCO2 ratio and alkalosis due to gain of base or loss of acid, i.e., rise in HCO3/ PCO2 ratio. [1,2,4]
Acid base and electrolyte disturbances are found in many ICU patients mostly with increased anion gap reflecting inorganic acidosis and serious disease. [5] These disturbances need to be immediately analyzed to provide information about changes in respiratory function, electrolyte imbalance and underlying disease and, also to find out the combination of disorders they have.
GCS (Glasgow Coma Scale) is a 15-point objective clinical scoring system for assessing changes in a patients’ conscious level. [6] The GCS tool enables one to effectively monitor the level of consciousness and provides a common language to improve communication in reporting neurological findings among healthcare professionals. [7,8] Causes for altered consciousness which causes low GCS include intra cranial causes such as head injuries, tumours, haemorrhages, seizures and degenerative conditions. Metabolic causes (acid base and fluid/electrolyte imbalances) are one of the extra cranial causes that can cause altered consciousness in a patient. Other extra cranial causes include hypoxia, sedative drug overdose, cardiovascular instability, sepsis, shock, trauma; liver, renal and endocrine dysfunction and multi-organ dysfunction. [9-11] The GCS grades severity of coma according to three categories of responsiveness: eye opening, motor, and verbal responses. The admission GCS has been linked to prognosis prediction for many conditions, including traumatic brain injury, subarachnoid hemorrhage, and bacterial meningitis and other. [12-15]
Some studies show electrolyte abnormalities were the most frequent occurrence (59% of patients) of low GCS but did not alter outcome. [16,17] According to the study by Sh. Pomernaz et al, hypokalaemia is the large catecholamine discharge that is known to accompany severe head trauma, with resultant β2 adrenergic stimulation of the Na+-K+ pump, which reflects poor survival outcome in critically ill patients. [18]
The primary objective of this study is to assess the survival outcome of acid-base electrolyte imbalance associated with low GCS patients in the medical ICU. The secondary objective was to analyze the pattern of electrolyte and acid base imbalances commonly seen in the ICU.
Subjects and Methods
During the study period of six months, a total of 276 patients were admitted in the medical ICU. Among these 100 patients were included in the study after excluding the patients who didn’t meet the inclusion criteria and those that had incomplete medical records. This retrospective study was done in a tertiary center in Chennai, India after approval of Institutional ethical committee clearance. Informed consent was waived because of the retrospective nature of the study. Patients above 18 years admitted to the medical ICU with electrolyte and acid base abnormality were included. Patients without any acid base disturbance on arrival to the ICU were excluded from the study. Patients with trauma and head injury, major surgeries, sedative overdose, septic shock, renal and hepatic failure, cardiogenic shock and multisystem organ failure were excluded from the study.
The clinical characteristics of the study population included patients with sepsis and severe sepsis, Diabetic ketoacidosis, Hyperosmolar hyperglycemic state, pancreatitis, poisoning, pneumonia, urinary tract infection, soft tissue infection, fungal infection, clostridium deficile and oncology patients.
The following data were recorded from patients’ medical record: cause of admission age, sex and days in ICU and the possible outcomes were recorded (discharge from the ICU (improved), or patient discharges against medical advice due to personal reasons (DAMA) or patient dies (death)). Results of sodium, potassium, chloride, bicarbonate, Blood Urea Nitrogen (BUN), creatinine, pH, PCO2 and PO2 were recorded. Arterial Blood Gas (ABG) results (from Siemens 238 Blood Gas Analyzer System) were recorded for analysis of electrolyte imbalance and acid base imbalance.
Sample analysis was done; values falling outside normal ranges for sodium, potassium and bicarbonate are described as abnormally high or low. Each patient’s ABG result was analyzed to identify the single or mixed acid-base disorder and the anion gap was calculated. [5]
Patients were categorized based on their GCS into two groups (GCS ≤ 10 and GCS >10) and this factor was studied to find out the effect on mortality. They were also compared by categorizing them into three groups, those that improved, died or went DAMA.
Data was presented as percentage (%) for frequencies and mean and, standard deviation for continuous variables. Independent Student’s T-test was done for comparison of continuous variables, and Chisquare test for frequencies using SPSS 13 software. A multivariate regression analysis was done to evaluate the role of confounding factors on final prognosis. Odds ratio and 95% confidence intervals were calculated using logistic regression. A p-value ≤ 0.05 was considered statistically significant.
Results
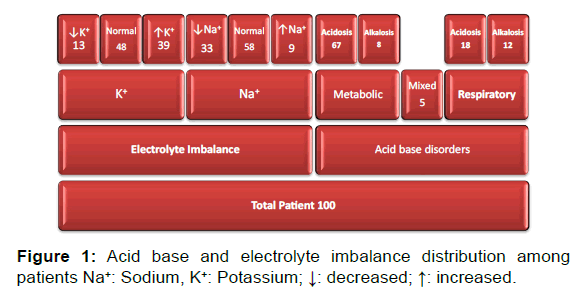
During the study period of six months, total of 276 patients were admitted in the medical ICU. After excluding the patients that didn’t meet the inclusion criteria and those that had incomplete medical records, the total study population was 100 patients (68 male and 32 female). The average age of the patients was 47.24±17.54 years. Patients were compared by various baseline characteristics [Table 1]. The study consisted of patients with metabolic acidosis (n=67), metabolic alkalosis (n=8), respiratory acidosis (n=18), respiratory alkalosis (n=12), and mixed acid base disorders (n=5). Since five patients had mixed acid base disorder total count is coming to 110 [Figure 1]. In terms of electrolyte imbalance, the study included patients with normal sodium (n=58%), hyponatremia (n=33%), hypernatremia (n=9%) and patients with normal potassium (n=48%), hypokalemia (n=13%), and hyperkalemia (n=39%).
| Total | Improved | Death | DAMA | ∞p-value | |
|---|---|---|---|---|---|
| Number of Patients (%) | |||||
| Total | 100 | 58 | 35 | 7 | |
| Age | |||||
| <40 | 34 | 22 (64.71%) | 12 (35.29%) | 0.135** | |
| ≥ 40 | 66 | 36 (54.55%) | 23 (34.85%) | 7 (10.6%) | |
| Sex | |||||
| Male | 68 | 40 (60%) | 23 (33.3%) | 5 (6.7%) | 0.9291** |
| Female | 32 | 18 (63.6%) | 12 (31.8%) | 2 (9.1%) | |
| GCS | |||||
| GCS ≤ 10 | 47 | 20 (42.55%) | 24 (51.06%) | 3 (6.39%) | <0.0001* |
| GCS>10 | 53 | 38 (71.7%) | 11 (20.75%) | 4 (7.55%) | |
*: Significant finding
** : Non significant finding
∞ p-value between groups improved and death
There were significantly higher mortality in patients with low GCS (p<0.0001)
Table 1: Characteristics of the study population.
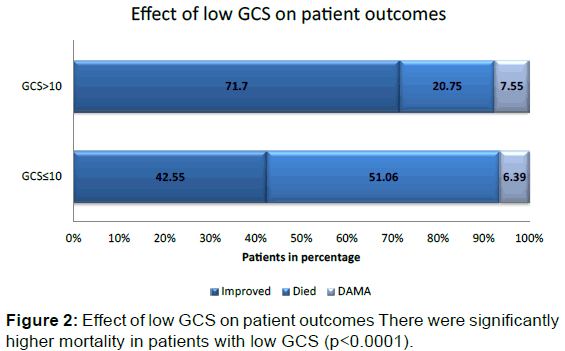
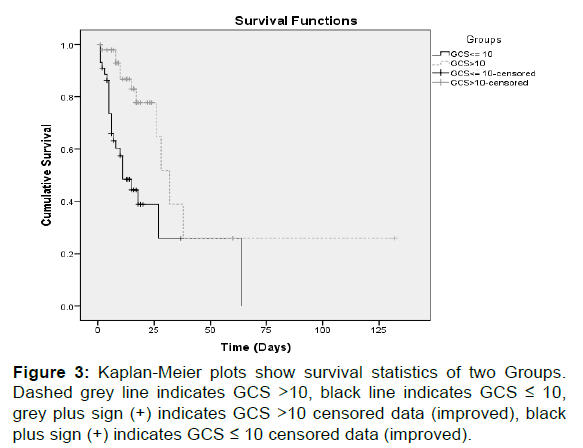
Mortality was significantly higher in patients with low GCS (51.06% vs. 20.75%, p< 0.0001) [Figure 2]. Survival statistics of the two groups is shown in Figure 3. However, there is no significant difference in values obtained for gender.
Comparison between the patients on basis of GCS was statistically significant for mean sodium, potassium and chloride, while other mean serum values or factors were not different [Table 2]. Sodium and chloride significantly increased (p=0.0126, 0.0464 respectively) and potassium significantly decreased (p=0.0008) when GCS was low.
| GCS ≤ 10 (n=47) | GCS>10 (n=53) | p-value | |
|---|---|---|---|
| Mean ± SD | |||
| Age (years) | 44.7 ± 16.86 | 49.49 ± 18.14 | 0.1764** |
| S. Sodium (136-145 mmol/L) | 138.02 ± 11.57 | 131.72 ± 10.44 | 0.0126* |
| S. Potassium (3.5-5 mmol/L) | 4.214 ± 1.386 | 5.26 ± 1.606 | 0.0008* |
| S. Chloride (98-106 mmol/L) | 102.85 ± 13.35 | 98.02 ±10.58 | 0.0464* |
| S. Bicarbonate (24-30 mmol/L) | 16.974 ± 6.284 | 16.421 ± 6.334 | 0.6624** |
| Anion Gap (8-14.9 mmol/L) | 18.104 ± 10.233 | 17.277 ± 8.807 | 0.6650** |
| BUN (10-20 mg/dl) | 37.149 ± 31.706 | 45.502 ± 32.260 | 0.1957** |
| Creatinine (<1.5 mg/dl) | 2.5021± 3.13 | 3.643 ± 4.374 | 0.1413** |
| pH (7.38-7.44) | 7.297 ± 0.199 | 7.283 ± 0.185 | 0.7101** |
| PCO2 (35-45 mm/Hg) | 35.951 ± 20.665 | 30.536 ± 15.466 | 0.1385** |
| PO2 (80-100 mm/Hg) | 104.97 ± 63.875 | 88.445 ± 36.898 | 0.1115** |
| Days in hospital | 11.36 ± 11.01 | 15.91 ± 19.23 | 0.1572** |
*: Significant finding
** : Non significant finding
There were statistically significant differences between patients with low GCS and higher GCS in terms of mean sodium, potassium and chloride.
Table 2: Outcome of study participants between the groups.
Metabolic acidosis was the most prevalent disorder (n=27) among the patients with GCS ≤ 10. Mortality was also significantly higher in the GCS ≤ 10 group with metabolic acidosis (55.6% vs. 17.5%, p=0.0013) compared to the patients with GCS >10 and metabolic acidosis [Table 3].
| Metabolic Acidosis | Total | Improved | Death | DAMA | p∞value |
|---|---|---|---|---|---|
| Number of Patients (%) | |||||
| Total | 67 | 40 (59.7%) | 22 (32.84%) | 5 (7.46%) | |
| Sex | |||||
| Male | 45 (67.2%) | 27 (60%) | 15 (33.34%) | 3 (6.66%) | 1 |
| Female | 22 (32.8%) | 13 (59.1%) | 7 (31.8%) | 2 (9.1%) | |
| GCS | |||||
| GCS ≤ 10 | 27 (40.29%) | 10 (37%) | 15 (55.6%) | 2 (7.4%) | 0.0013 |
| GCS>10 | 40 (59.71%) | 30 (75%) | 7 (17.5%) | 3 (7.5%) | |
Table 3: Characteristics of the study participants with metabolic acidosis.
Among the GCS ≤ 10 patients there were patients with metabolic acidosis (n=27), metabolic alkalosis (n=3), respiratory acidosis (n=9) and respiratory alkalosis (n=9) and mixed base disorders (n=1). The most common electrolyte disorder among patients with GCS ≤ 10 is hyperkalemia, hyponatremia and hypernatremia. Another common disorder found among all the patients was the combined disorder of metabolic acidosis, hyperkalemia and hyponatremia (n=14.9%). The patients with hypernatremia and metabolic acidosis had 71.44% mortality rate. The patients with a low GCS have a higher incidence for multiple electrolyte disturbances. Low GCS leads mostly to an increased mortality especially in the patients with acid base disorders with electrolyte disorders compared to those with pure acid-base disturbances.
To identify prognostic factors of the patients in the ICU, we performed multiple regression analysis using the data we collected. Among all the variables only three independent factors (GCS, BUN and Creatinine) significantly correlated with the criterion. Thus the multiple regression model with all three predictors produced R² =0.138473, F(3,89) =4.768334, p =0.003959. As can be seen in Table 4, GCS had significant positive regression weights, indicating patients with better GCS score were expected to have better chances of improving, after controlling for the other variables in the model. The BUN and creatinine have a significant negative weight (opposite in sign from its correlation with the criterion), indicating that after accounting for GCS and other variables those patients with higher BUN scores and higher Creatinine results were expected to have a negative prognosis (a suppressor effect). This model indicates those with higher GCS resulted in better prognosis in the medical ICU, while higher Creatinine readings and higher BUN have an opposite result on prognosis. This was represented by the model as follows: prognoses=0.025994 × GCS (1 unit change) –0.00683× BUN (mg/dl)-0.042533 × Creatinine (md/ dl) +0.460593. The prognosis of patients in the medical ICU with low GCS have a variety of factors, GCS, BUN and Creatinine were found to be potential factors influencing prognosis in the medical ICU. Monitoring these factors may be helpful to get a better outcome in the medical ICU.
| Variable | Multiple regression weights | P value | Lower 95% | Upper 95% |
|---|---|---|---|---|
| GCS | 0.025949 | 0.02963 | 0.002634 | 0.049265 |
| BUN | -0.00683 | 0.010394 | -0.01201 | -0.00165 |
| Creatinine | -0.04255 | 0.043128 | -0.001349 | -0.083758 |
Table 4: Multivariate regression analysis results.
Discussion
Acid base disorders often seen in patients in the ICU, are a major health problem and are the primary contribution to morbidity and mortality in the ICU. [5] In this regard, one of the crucial issues in acid base and electrolyte imbalance is predicting its outcome when GCS is low. Studies by Demetriades et al. and Weir et al. show that low GCS implies poor prognosis in patients with head injuries and stroke. [19,20] Studies by Choi et al. and Piek et al. showed electrolyte abnormalities were the most frequent occurrence (59% of patients) but did not alter outcome. [16,17] while another study by Pomeranz et al. shows poor outcome in low GCS patient associated with acid base disorder. [18]
Sodium is involved in the transmission of nerve impulses and muscle contraction. [21] Symptoms of hypernatremia include restlessness, seizures and coma which affect GCS. People with low GCS have loss of consciousness and this leads to inability to express the feeling of thirst and consequently a low intake of free water. This inability to drink water causes increase in sodium (eg. Diabetes Insipidus). [21,22] Hypernatremia is associated with increased mortality in hospitalized patients and in medical intensive care units. In a study by Aiyagiri, hypernatremic patients had a lower median admission GCS score (8 vs. 14, P< 0.001), and those patients with low GCS admission scores were independently associated with increased mortality. [23] A study by Amini et al. also showed the mortality rate was higher in head trauma patients with more severe hypernatremia with lower GCS. [24] This present study, shows significant sodium increase and increased mortality when GCS was low.
Hyponatraemia is under-documented, inaccurately investigated and sub optimally managed, leading to poor patient outcomes. There is a well-recognised association with inpatient morbidity and mortality. Frequently, insufficient diagnostic assessment and investigations take place, and this can affect both patient management and outcomes. [25] Critical care patients being treated for hyponatremia require diligent monitoring. Depending on the severity of the condition and the selected treatments, serum sodium levels should be measured every 1 to 2 hours during initial treatment and then at least every 4 hours until signs and symptoms resolve. [26] Therapy must then be dictated not only by recognised reversible causes, such as advanced hypothyroidism, adrenal insufficiency, diuretics or other medicines, but also by whether the hyponatraemia occurs acutely or chronically and the degree of symptoms related to it. [27]
In cancer patients, hyponatremia is a serious comorbidity that needs special care as its treatment varies by pathophysiologic groups, and its consequences can have a deleterious effect on the patient’s health. [28] Critically, most evidence suggests that overenthusiastic treatment of SIADH is considerably more dangerous than treatment that is slow or relatively ineffective. It is vital that all doctors should be aware of the need for a slow pace of normalization of serum sodium except in the most extreme circumstances. [25]
Whether hyponatraemia in a patient with cancer is just an indicator of poor prognosis or whether its presence may alter the patient’s quality of life has not been definitively proven, but increasing evidence shows that hyponatraemia must not be taken lightly. [29]
The balance of chloride is closely regulated by the body. Significant increases or decreases in chloride can have deleterious or even fatal consequences: Chloride is also involved in regulating blood pressure. Hyperchloremia, can be caused by kidney failure, kidney dialysis, and an overproduction of parathyroid hormone. In this study, chloride significantly increased (p=0.0464) when GCS was low.
Potassium ions play a major role in regulating fluid balance in cells, the transmission of nerve impulses, and in muscle contractions. [30] A symptom of hypokalemia is confusion or disorientation which in turn is related to the low GCS. A study by Sh. Pomernaz et al. concluded that hypokalaemia is the large catecholamine discharge that is known to accompany severe head trauma, with resultant β2 adrenergic stimulation of the Na+-K+ pump, which reflects poor survival outcome in critically ill patients [19]. The present study concurs, when GCS is low due to electrolyte imbalance potassium significantly decreased (p=0.0008) [Table 2].
Though the two groups were not statistically different in other aspects apart from sodium, potassium and chloride, the results strongly indicate that once GCS is below ten, a poor prognosis is more likely especially in patients with significant acid base disorders with electrolyte disorders compared to patients with only acid base disturbances. The odds for mortality are significantly higher when GCS is low. Early intervention is essential to rectify acid base and electrolyte imbalance to prevent episodes of altered consciousness and avoid poor patient outcomes.
Admissions to the ICU are a traumatic time for patients and their family members. The cases where the patients are in an altered state of consciousness, combined with their unstable nature and strong probability of death, makes the families of patients with such long-term illness vulnerable and under extreme stress. The severity of the disease may place demands on patients’ families beyond the families’ ability to cope. [31]
In the cases of patients with chronic or terminal illness, the patient and health care provider roles need to be modified in the treatment of a chronic condition. The patient has to take a more proactive role in managing their condition and preventing complications, health care providers act as consultants, interpreters of symptoms, resource persons, and offer treatment suggestions. The care manager works directly with the families of ICU and terminal patients, helping the families throughout the hospital stay, as the families deal with severe illness and sometimes death. The role of care managers is serving as a bridge between physicians, specialists, and patients, collaborating with the patients’ doctors while working directly with patients. In cases where the patient is not in state to take decisions they help and guide the family members on the situation in a way that is less stressful. [32] Family advocates/care managers’ care for families just as nurses and physicians care for the critically ill patient. [33] The task of the care manager is mainly to help the patient individually or his family members in helping to adopt behaviors and lifestyles suitable to the patient’s health condition, and encouraging greater self-sufficiency in the monitoring of the parameters through the knowledge of the disease in order to achieve better outcomes. [34]
Conclusion
In this retrospective analysis, we assessed the outcome of low Glasgow Coma Scale (GCS) patients associated with acid base and electrolyte imbalance in the medical ICU and found a strong association between low GCS and mortality.
Electrolyte and acid base disturbances should be seriously considered in low GCS patients to allow timely and appropriate therapeutic intervention to improve survival outcome.
Research Limitations
The strengths of this study are that the population was a homogenous one, representing the general medical ICU population excluding any cases with trauma. Though the study is retrospective in nature and we had to rely on previously recorded data we have reduced selection bias to the best of our ability. While the study reached its aims, its retrospective nature implies that associated factors of other co morbid conditions can affect study outcomes, so we are suggesting a randomized prospective study to assess survival outcome of low GCS patients associated with acid base and electrolyte imbalance in the ICU with a larger sample size and observed for a longer duration.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Richard J. Haber. A practical approach to acid-base disorders. West J Med. 1991; 155: 146-151.
- Horacio J. Adrogué, Nicolaos E. Madias. Management of life-threatening acid–base disorders. N Engl J Med 1998; 338: 26-34.
- Kraut JA, Madias NE. Serum anion gap: Its uses and limitations in clinical medicine. Clin Jour American Society of Nephrology CJASN 2007; 2: 162-174
- Ishihara K, Szerlip HM. Anion gap acidosis. Seminar Nephrology 1998; 18: 83-97.
- Fulop M. Flow diagrams for the diagnosis of acid base disorders. Journal of Emergency Medicine 1998; 16: 97-109.
- Wiese MF. Different versions of the Glasgow Coma Scale: telephone survey. BMJ 2003; 327: 782-783.
- Aird T. McIntosh M. Nursing tools and strategies to assess cognition and confusion. Br J Nurs 2004; 13: 621-626.
- Fischer J. Mathieson C. The history of the Glasgow Coma Scale: implications for practice. Crit Care Nurs Q. 2001; 23: 52-58.
- Jennet B. Altered consciousness and coma. In: Crockhard A. Harward R. Hoff JT (eds). Neurosurgery: The scientific basis of clinical practice: Blackwell Science, Oxford 1986: 117-26.
- Teasdale GM, Jennett B. Assessment of the coma and impaired consciousness: A practical scale. Lancet 1974; 2: 81-84.
- Gabbe BJ, Cameron PA, Finch CF. The status of the Glasgow Coma Scale. Emergency Medicine 2003; 15: 353-360.
- Van de Beek D, De Gans J, Spanjaard L, et al. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med 2004; 351: 1849.
- Servadei F, Nasi MT, Cremonini AM, Giuliani G, Cenni P, Nanni A. Importance of a reliable admission Glasgow Coma Scale score for determining the need for evacuation of post-traumatic subdural hematomas: A prospective study of 65 patients. J Trauma 1998; 44: 868.
- Qureshi AI, Sung GY, Razumovsky AY, Lane K, Straw RN, Ulatowski JA. Early identification of patients at risk for symptomatic vasospasm after aneurysmal subarachnoid hemorrhage. Crit Care Med 2000; 28: 984.
- Booth CM, Boone RH, Tomlinson G, Detsky AS. Is this patient dead, vegetative, or severely neurologically impaired? Assessing outcome for comatose survivors of cardiac arrest. JAMA 2004; 291: 870.
- Choi SW, Koh HS, Yeom JY, Kim SH, Song SH, Kim Y. Clinical analysis of the risk factors and prognostic factors of delayed deterioration following mild head injury. J Korean Neurosurg Soc, 1999: 1316-1323.
- Piek J, Chesnut RM, Marshall LF, Berkum-Clark MV, Klauber MR, Blunt BA, et al. Extracranial complications of severe head injury, Journal of Neurosurgery, 1992; 77: 901-907.
- Pomeranz SH, Constantini SH, Rappaport ZH. Hypokalaemia in severe head trauma, Acta Neurochirurgica, 1989; 97: 62-66.
- Demetriades D, Kuncir E, Velmahos GC, Rhee P, Alo K, Chan LS. Outcome and prognostic factors in head injuries with an admission Glasgow Coma Scale Score of 3. Arch Surg. 2004; 139:1066-1068.
- Weir CJ, Bradford AP, Lees KR. The prognostic value of the components of the Glasgow Coma Scale following acute stroke. QJM 2003; 96: 67-74.
- Kumar S, Berl T. Sodium. The Lancet 1998; 352: 220-228.
- Fried LF, Palevsky PM. Hyponatremia and hypernatremia. Med Clin North Am 1997; 81 (3): 585-609.
- Aiyagari V, Deibert E, Diringer MN. Hypernatremia in the neurologic intensive care unit: How high is too high? J Crit Care. 2006; 21: 163-172.
- Amini SH, Heydari Z. Sodium disturbances and its relation with mortality and morbidity in head trauma patients admitted to general ICU at Zahedan Khatam-Al-Anbia Hospital from May 2003 to September 2004. Journal of Iranian Society Anaesthesiology and Intensive Care 2007; 29: 24-30.
- Grant P, Ayuk J, Bouloux PM, Cohen M, Cranston I, Murray RD, et al. The diagnosis and management of inpatient hyponatraemia and SIADH. European Journal of Clinical Investigation. 2015; 45: 888-894.
- Decaux G, Soupart A. Treatment of symptomatic hyponatremia. Am J Med Sci. 2003; 326: 25-30.
- Verbalis JG, Goldsmith SR, Greenberg A, Korzelius C, Schrier RW, Sterns RH, et al. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations. Am J Med 2013; 126: S1-S42.
- Onitilo AA, Kio E, Doi SA. Tumor-related hyponatremia. Clinical Medicine & Research, 2007; 5: 228-237
- Schrier RW, Sharma S, Shchekochikhin D. Hyponatraemia: More than just a marker of disease severity? Nat Rev Nephrol 2013; 9:37-50
- Halperin ML, Kamel KS. Potassium. The Lancet 1998; 352: 220-228.
- Medland JJ, Ferrans CE. Effectiveness of a structured communication program for family members of patients in an ICU. Am J Crit Care. 1998; 7: 24-29.
- Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, Mola E, et al. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vascular Health and Risk Management. 2010; 6: 297-305.
- Washington GT. Family advocates: Caring for families in crisis. Dimens Crit Care Nurs. 2001; 20: 36-40.
- Cecere A, Scicchitano P, Zito A, Sassara M, Bux F, Caldarola P, et al. Role of care manager in chronic cardiovascular diseases. Ann Gerontol Geriatric Res, 2014; 1: 1005.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.