Actualities of Management of Aural, Nasal, and Throat Foreign Bodies
- *Corresponding Author:
- Dr. Titus S Ibekwe
Department of ENT, University of Abuja Teaching Hospital, PMB 228, Abuja, Nigeria.
E-mail: ibekwets@yahoo.com
Abstract
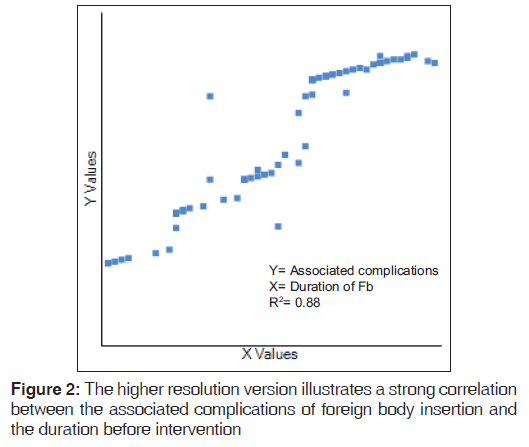
Background: Foreign bodies (Fbs) in the ear, nose, and throat (ENT) are common presentations in healthcare settings worldwide. Aim: This study was carried out to review the modes of presentation, management, and outcome of inserted Fbs in our setting. Subjects and Methods: A 5‑year retrospective study of cases of ENT Fbs managed at two referral hospitals in Abuja Nigeria. The analysis was done with Chi‑square and Pearson correlation. Results: Five hundred and ninety‑four patients aged 0–75 years, M:F = 1.1 (295 vs. 299) were reviewed. Prevalence was predominantly among the under 5 s; 286/594 (P = 0.001). ENT Fbs were 356/594 (59.9%), 167/594 (28.1%) and 71/59 (12.0%), respectively. Cotton wool 133/356 (37.4%) and beads 75/356 (21.1%) constituted most aural Fbs. Beads 45/167 (27.0%) and grains/seed 37/167 (22.1%) were the most common nasal Fbs while fish bones 38/71 (53.5%) and piece of metals 12/71 (16.9%) were dominant in the throat. Most cases of aural and nasal Fbs were asymptomatic. Ear syringing was the most common method for removal of aural Fbs 216/594 (60.7%) and instrumentation under direct vision for nasal Fbs 153/167 (91.6%). Furthermore, 52/71 (73.2%) of throat Fbs were removed under general anesthesia. ENT complications observed included bruises, lacerations, perforations, Epistaxis, and a case of respiratory failure. Delayed presentation (beyond 24 h) was seen in 489/594 (82.3%) of cases while failed previous attempts by untrained hands constituted 353/594 (59.4%). A strong correlation between complications and duration of Fbs insertion (R2 = 0.8759) was established. Conclusions: Fbs in ENT are common especially among children below 5 years. Majority presented beyond 24 h, and there was a strong correlation between duration of Fbs insertion and associated complications. Repeated failed attempts and delayed referrals to otorhinolaryngologists from peripheral centers were also contributing factors to increased morbidity and hence the need for awareness.
Keywords
Aural, Foreign bodies, Laryngeal, Nasal, Otorhinolaryngologist, Pharyngeal, Throat
Introduction
Foreign bodies (Fbs) in the ear, nose, and throat (ENT) are commonly seen in the medical practice by Otorhinolaryngologists, Pediatricians, Emergency Department Surgeons, Physicians and even in the primary care setting. [1] If not properly managed, it has high potentials for morbidity/mortality and huge costs of management. [2-4]
Loose Fbs in the postnasal space can be accidentally aspirated or even pushed back into the respiratory tree during attempts at removal leading to respiratory obstruction. [5] In addition, Fbs in the nose have been implicated as carriers of diphtheria and other infectious diseases. [6]
Several reports have been written, describing the removal of Fbs from the ear, nasal cavity, and throat. [5] However, few have comprehensively reviewed this vital subject and served as a motivation to conduct this retrospective analysis on the ages at presentation, modes of presentation, and management options available for the removal of Fbs from the ENT.
We reviewed cases of Fbs in the ENT over a 5 year period with the aim of auditing current practice, suggesting possible areas of improvement and raising awareness on this problem with particular reference to developing health care settings like Nigeria.
Subjects and Methods
This is a 5-year retrospective study (January 2009 to December 2013) of Fbs in the ENT of patients who presented in the ENT Specialist Clinics of University of Abuja Teaching Hospital, Gwagwalada and Garki Hospital, Abuja – both tertiary health institutions in Nigeria’s Federal Capital Territory with patient loads from mainly four neighboring states in the middle belt and Northern region of the Federation and even from the Southern region.
The patients’ registers from the ENT Clinics were consulted. All relevant cases were listed. Then the case files and clinic notes of patients were retrieved from the Medical Records Departments. Information obtained from the case files include: Age at presentation, gender, type of foreign body, sites of presentation, signs and symptoms, duration of insertion, previous attempts at removal, management practices, outcomes, and observed complications.
Simple descriptive analyses (Chi-square and Pearson correlation) were used to analyze the data generated. Permission was sought and obtained from the relevant hospital authorities for use of the data.
Results
A total of 629 patients was enrolled for the study out of 5152 patients managed in the ENT clinics of both hospitals in the review period. However, 35 had to be excluded due to misplaced case records or insufficient data. Only 594 patients had their data analyzed and formed the basis for this study representing 594/5152 (11.5%) of patients seen in the ENT clinic. Two hundred and eighty-six, 286/594 (48.1%) of the patients were aged 0–5 years old, 119/594 (20.0%) 6–15 years old and the rest as in Table 1a.
| Age | Frequency (%) |
|---|---|
| 0-5 | 286(48.1) |
| 6-15 | 119(20.0) |
| 16-39 | 118(19.9) |
| 40-64 | 57(9.6) |
| 65-75 | 14(2.4) |
| Total | 594 (100.0) |
Table 1a: Age distribution
The under 5 years were significantly preponderant, and this is in consonance with earlier reports in favor of children.
Three hundred and fifty-six (59.9%) presented with Fbs in the ear, 167 (28.1%) in the nose, and 71 (12.0%) in the throat. Two hundred and ninety-nine (50.3%) patients were female and 295 (49.7%) were male.
The 0–5 year group was most likely to insert Fbs into the ears and nose. However, the incidence of Fbs in the nose showed a decline with increasing age. For Fbs in the throat on the other hand, it was observed that there was an increase in incidence from the 0 to 5 year group to the 6–15 years group and subsequent decrease with increasing age [Table 1b].
| Age | Ear FB | Nose FB | Throat FB | Total |
|---|---|---|---|---|
| 0-5 years | 124 | 146 | 16 | 286 |
| 6-15 years | 77 | 20 | 22 | 119 |
| 16-39 years | 96 | 1 | 21 | 118 |
| 40-64 years | 45 | ‑ | 12 | 57 |
| 65-75 years | 14 | ‑ | ‑ | 14 |
| Column totals | 356 | 167 | 71 | 594 |
FB: Foreign body
Table 1b: Age distribution according to location
Varieties of Fbs were recorded from the ENT [Table 2]. Cotton wool (37.4%), beads (27.0%), and fish bones (53.5%) constituted the most common Fbs in the ENT, respectively. Unusual Fbs like zippers, hooks, button batteries, insects, etc., were also recorded. The details are in Table 2.
| Type | Frequency (%) |
|---|---|
| Aural FBs | |
| Cotton wool | 133 (37.4) |
| Beads | 75 (21.1) |
| Grains and seeds | 41 (11.5) |
| Stones | 31 (8.7) |
| Pieces of metal | 17 (4.8) |
| Insects | 16 (4.5) |
| Foam | 15 (4.2) |
| Pieces of wood | 10 (2.8) |
| Pencil lead | 8 (2.2) |
| Erasers | 5 (1.4) |
| Crayon | 3 (0.8) |
| Paper | 2 (0.6) |
| Total | 356 (100.0) |
| Nasal FBs | |
| Grains and seeds | 45 (27.0) |
| Beads | 37 (22.1) |
| Cotton wool | 22 (13.2) |
| Foam | 12 (7.2) |
| Unspecified | 19(11.3) |
| Pieces of metal | 7(4.2) |
| Pieces of wood | 6(3.6) |
| Stones and pebbles | 5(3.0) |
| Crayons | 5(3.0) |
| Pieces of cloth | 3(1.8) |
| Erasers | 3(1.8) |
| Pencil lead | 2(1.2) |
| Paper | 1(0.6) |
| Total | 167(100.0) |
| Throat FBs | |
| Fish bone | 38(53.5) |
| Pieces of metal | 12(16.9) |
| Cotton wool | 8 (11.2) |
| Dentures | 4(5.6) |
| Unspecified | 3(4.2) |
| Pieces of cloth | 1(1.4) |
| Grains and seeds | 1(1.4) |
| Stone and pebbles | 1(1.4) |
| Beads | 1(1.4) |
| Pencil lead | 1(1.4) |
| Pieces of wood | 1(1.4) |
| Total | 71 (100.0) |
FBs: Foreign bodies
Table 2: Types of FBs
Of the Fbs lodged in the ear, 63.4% were in the right ear, 30.2% in the left, and 6.4% bilateral. For nasal Fbs, 79.3% were in the right nasal cavity and 20.7% in the left. Most of the patients with aural Fbs (56.0%) were asymptomatic at presentation. Others had otalgia, otorrhea, tinnitus, etc., [Table 3]. The features for nose and throat Fbs are highlighted in Table 3.
| Presentation | Frequency (%) | |
|---|---|---|
| Aural FBs | ||
| Asymptomatic | 199 | (56.0) |
| Otalgia | 119 | (33.4) |
| Otorrhea | 20 | (5.6) |
| Tinnitus | 18 | (5.0) |
| Total | 356 | (100.0) |
| Nasal FBs | ||
| Asymptomatic | 120 | (71.9) |
| Rhinorrhea | 47 | (28.1) |
| Total | 167 | (100.0) |
| Throat FBs | ||
| Persistent throat pain | 53 | (74.6) |
| Difficulty breathing | 18 | (25.4) |
| Total | 71 (100.0) | |
FBs: Foreign bodies
Table 3: Signs and symptoms
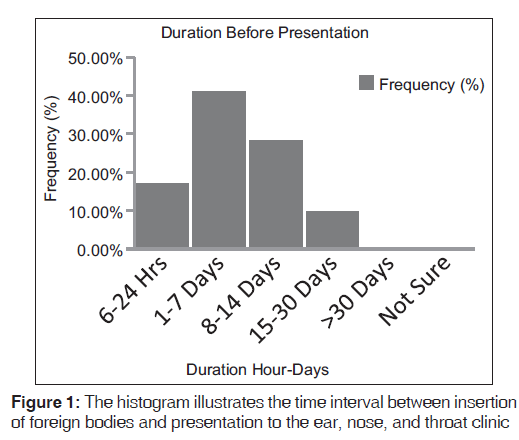
In 63.1% of cases, parents observed the presence of a foreign body in children, and in 36.9% was self-reported by the patients. Then, 17.7% presented within 24 h of insertion, 41.5% within 1 week, 28.7% within 2 weeks and 10.2% within 1 month [Figure 1].
Previous attempts at removal of aural, nasal, and throat Fbs had been made in (210/594) 59.4% of patients before presenting in the ENT Clinic.
A total of (224/356) 62.9% of the aural Fbs was removed by ear syringing, (94/356) 26.4% with the use of Jobson Horne’s probe under direct vision, and (38/356) 10.7% were removed under general anesthesia in the surgical theater. Nasal Fbs were, however removed with the use of a probe under direct vision in (153/167) 91.6% of cases, whereas 8.4% had theirs removed under general anesthesia. Fbs lodged in the throat had 73.2% removed in the surgical theater under general anesthesia whereas out of the 26.8% that were managed in the clinic, 19.5% were not seen after thorough examination in the clinic needing no further management than symptomatic medical treatment after no objects were seen on radiology; with 7.3% of the Fbs manually removed [Table 4a].
| Treatment | Frequency (%) |
|---|---|
| Aural FBs | |
| Removal without general anesthesia | |
| Ear syringing | 224 (62.9) |
| Instrumentation under direct vision | 94(26.4) |
| Removal under general anesthesia | |
| Deeply impacted FB | 38(10.7) |
| Trauma from prior attempts at removal | 25 (7.0) |
| Total | 356(100.0) |
| Nasal FBs | |
| Removal without general anesthesia | |
| Instrumentation under direct vision | 153 (91.6) |
| Removal under general anesthesia | |
| Deeply impacted FB | 14 (8.4) |
| Trauma from prior attempts at removal | 17(10.2) |
| Total | 167(100.0) |
| Throat FBs | |
| Removal without general anesthesia | |
| Instrumentation under direct vision | 19(26.8) |
| and medical management | |
| Removal under general anesthesia | |
| Deeply impacted FB | 52(73.2) |
| Total | 71 (100.0) |
FBs: Foreign bodies
Table 4a: Modalities of treatment
It can be significantly deduced from the above chart [Figure 1] that most complications correlated with delayed presentations beyond 24 h of insertion of Fbs, whereas the very few seen within early referrals followed failed attempts at removal by untrained hands.
Among the cases in whom complications were observed, they included bruises, lacerations, perforations, and otitis externa for aural Fbs 195/356 (54.9%) and bruises, lacerations and epistaxis for nasal Fbs 72/167 (43.1%) especially in those with previous failed attempts at removal. For throat Fbs, one case was complicated by respiratory failure despite intensive care majorly following delayed presentation [Table 4b].
| Complication | 0-24 h | 2-7 days | 8-14 days | 15-30 days | Row totals |
|---|---|---|---|---|---|
| Ear bruises and lacerations | 4 | 6 | 11 | 0 | 21 |
| Tympanic perforations | 0 | 1 | 3 | 4 | |
| Otitis externa | 0 | 0 | 2 | 1 | 3 |
| Nasal bruises and lacerations | 1 | 2 | 14 | 0 | 17 |
| Epistaxis | 0 | 5 | 0 | 0 | 5 |
| Respiratory failure | 0 | 0 | 0 | 1 | 1 |
| Column totals | 5 | 14 | 30 | 2 | 51 |
FB: Foreign body
Table 4b: Complications recorded against the duration of FB insertion
Majority of cases were treated on an out-patient basis – 318/356 (89.3%) for ear Fbs and 153/167 (91.6%) for nose Fbs. 38/356 (10.7%) of ear Fbs and 14/167 (8.4%) of nose Fbs had to be admitted for a duration not exceeding 12 h following removal under general anesthesia. For throat Fbs however, the reverse was the case with 52/71 (73.2%) being admitted on account of the need for removal under general anesthesia due to deeply impacted Fbs and only 19/71 (26.8%) managed on an out-patient basis.
Discussion
The insertion of Fbs into the ENT has been acknowledged to be a common presentation among children, the elderly, and mentally retarded. Commonly identified inanimate foreign objects include rubber erasers, pebbles, beads, safety pins, sponges, and chalk. [7-9]
The most common presentations in our series were seen in children below 5 years of age [Tables 1a and b] and the items inserted were objects commonly found around them. [10-13] This higher occurrence in children especially the “under 5s” is due mainly to curiosity, restlessness, and zeal toward exploration leading to the probing of the various orifices within their bodies including the ear and nose. They are more likely to insert small objects into their ears, nose or even those of their playmates. [14] It is for this reason that parents should be vigilant about the items that can be reached easily by young children. Items such as beads, whistles, and other small toys should be kept out of reach. Even the insertion of grains and seeds into the cavities points at the fact that children should to some extent be supervised by adults during meals. Modern day society with increasingly busy and occupied mothers has led to a higher incidence of children not being monitored as closely as possible.
With increasing age, however, this energy dissipation is expected to decrease with a resultant decrease in the incidence of foreign body insertion. This expectation is in keeping with our findings and the findings of other studies. [11,12,15]
An interesting finding which is uncommon and not encountered in previous series on Fbs was the insertion of pencil lead observed in 2.4% of aural Fbs, 1.2% of nasal and 1.4% of throat Fbs [Table 2]. Among patients under the age of 5 years, the most common item inserted into the ears or the nose was beads, making up 19.3% of aural Fbs (47.1% of aural Fbs in children) and 27.0% of nasal Fbs [Table 2]. This is in keeping with a study on aural Fbs conducted by Fasunla et al. in Ibadan, 2006 which found beads to be the most common foreign body inserted by children, as against grains and seeds reported by previous studies. [4,11,12,15-17]
Beads from hair accessories commonly used to adorn children’s hair, as part of necklaces and prayer beads for those of the Catholic or Muslim faith are, therefore, quite easily accessible in the home. Their bright and colorful nature would also be attractive to children. It is worthy of note that among the metal objects detected in Table 2, were six incidences of small button batteries – 5 (0.8%) of whom lodged these batteries in the nose, and 1 (0.17%) in the ear. Such batteries are known to break down and cause rapid alkaline tissue injury following delay in removal. However, none of our patients experienced this.
In adults, the predominant foreign body observed was cotton buds used to clean ear wax. A study conducted by Ologe et al. in Ilorin, Nigeria in 2002 found cotton buds to be an important etiological factor in the traumatic perforation of the tympanic membrane. [16] It is necessary to educate the populace on the importance of avoiding cleaning the ears with cotton buds as the cotton top can very easily dislodge within the ear canal. [15] The external auditory canal does not require any additional cleaning, as a natural cleaning mechanism already in place which involves epithelial migration aided by jaw movement is quite sufficient. [18] The most common foreign body lodged in the throat was fish bone making up 53.5% of cases and 16.9% presented with metal objects such as zippers and jewelry lodged in the throat [Table 2]. All patients who presented with fish bone insertion were adults, which is to be expected as children’s meals are often carefully prepared and devoid of bones. However, the occurrence of foreign body in the throat of a child was seen to include objects like a metal zipper which the child is likely to have seen lying around and probably put in the mouth.
Majority of patients who presented with Fbs in either the ear or nasal cavity were asymptomatic–56.0% for aural Fbs and 71.9% for nasal Fbs, compared to the presentation of persistent pain (74.6%) and difficulty in breathing (25.4%) seen with cases of throat Fbs [Table 3]. This, therefore, highlights the need for a high index of suspicion and thorough examination when managing presentations in the aural and nasal cavities. Some reports have it that Fbs in the nasal cavity could present for years without symptoms and only detected as incidental findings. [19]
A unilateral mucopurulent nasal discharge could sometimes occur and was seen in 20.0% of subjects with nasal Fbs [Table 3]. The nasal discharge may occasionally be blood-stained, and the unilateral vestibulitis especially in children is diagnostic. [5,20] Rarely, pains and headaches have been reported on the involved side often with intermittent epistaxis or sneezing reported by others. [20] Other writers have reported some cases with bromhidrosis (foul body odor) associated with nasal Fbs in children. [21] Neither pain, headaches, nor bromhidrosis was reported by any of our patients.
It is of utmost importance that when Fbs have been inserted into the ear they are removed safely by qualified personnel to avoid further injury. [15] In our center, the patients were pacified to gain their cooperation and sometimes restricted through parents/caregivers help leading to visualization and foreign body removal without resort to the use of general anesthesia. Our experience showed that this phase of management is very important and should be carefully handled to gain the confidence of the patients and/or caregivers. Furthermore, multiple attempts can be counter-productive and therefore good visualization, and excellent maneuver is a key.
The aural Fbs were removed with the child seated in an adult’s lap in the examination chair with the child’s arm and trunk securely held by the adults right arm, and the head immobilized by the left arm. [3,4,10] If however the patient were uncooperative, or the foreign body were to be lodged in the middle ear cavity there would then be a need to remove it under general anesthesia and otomicroscopy which would provide adequate magnification and assessment of the space between the foreign body and tympanic membrane. [15] In cases of foreign body in the middle ear, postaural tympanotomy would be necessary in order to remove it. [15]
In our centers, the child with a nasal foreign body was usually examined in an upright sitting position and with the head tilted back slightly so that the floor of the nose was visible to the examiner. Often, a parent or caregiver would aid in restraining and holding the child steady. Majority of inanimate Fbs when well-visualized can be easily removed via anterior rhinoscopy with cupped forceps, artery forceps, curved hooks, Eustachian tube catheters, and suction, Jobson Hornes probe with or without the use of a local anesthetic agent. [5] A similar position would also be adopted in order to visualize a foreign body in the throat of a child, tilting the head back slightly and holding the mouth wide open. However, endoscopic visualization is often necessary with throat foreign body presentation.
Complications that can arise from the process of removal of nasal Fbs include the inhalation of the foreign body which as a result of clumsy attempt at removal is pushed back into the nasopharynx; marked epistaxis and sudden terror and agitation requiring sedation with a general anesthetic. [5,20] These complications highlight the need for attempts at foreign body removal to be made by only adequately qualified and experienced personnel in order to prevent further problems on the part of the patient.
In rare cases, the only successful method of removing a nasal foreign body is to push the object posteriorly, so it enters the pharynx and is subsequently retrieved under general anesthesia with endotracheal intubation carried out to protect the airways. [5,22] Only 8.4% of patients with nasal Fbs in this study had them removed under general anesthesia.
For the removal of animate Fbs in the nose such as worms, larvae, maggots, and insects, a weak solution of 25% chloroform is instilled into the nasal spaces to kill the larvae. [5] It may need to be repeated up to two to three times a week for up to 6 weeks until the larvae are killed, when they can be subsequently removed by either blowing the nose, suction, irrigation, or curettage. [5] In some cases of roundworms in the nose, manual or forceps extraction would suffice. [5] However, none of the cases studied here presented with animated Fbs in the nose. On the other hand, insect in the ear is a fairly commoner occurrence. We had 16 cases [Table 2] in our series and this could be easily treated by instilling some bland oil into the ear canal or cotton wool pladget impregnated with alcohol in the external ear to suffocate the insect before manual evacuation.
Emergency intervention is crucial in the management of throat Fbs because of the risk of respiratory distress from complete airway obstruction. [23] This perhaps explains the high rate of surgical removal of throat Fbs observed in this series. Common Fbs which lead to obstruction in children include balloons, pieces of soft deformable plastic, and food boluses. [24] In the event that the foreign body in the throat is nonobstructing or partially obstructing, patients would often present with a history of choking, dysphagia, odynophagia, or dysphonia. [10] Pharyngeal Fbs should also be suspected in patients with undiagnosed coughing, stridor, or hoarseness. [25]
As with aural and nasal Fbs, a high index of suspicion is required, and parents and caregivers of children with symptoms of partial airway obstruction should be asked whether choking and aspiration have occurred. Delayed presentation [Figure 1] in addition to increasing the risk of complications, also complicates the diagnosis. Several study series describe Fbs in the throat that were misdiagnosed and treated as croup. [24,26]
The most common Fbs in the throat are pieces of plastic, metal pins, seeds, nuts, bones, coins, and dental appliances. [24,25,27,28] Radiography can be helpful in localizing coins, button batteries, and other radiopaque objects, but most laryngeal Fbs, including many fish bones, are radiolucent. [10,29] Therefore, the decision to pursue surgical intervention should be based on the patient’s history and a physical examination that suggests the presence of a foreign body rather than based on radiography alone. [30] The presentation of difficulty in breathing and history was key to rushing the cases who ingested and aspirated a metal zipper to theatre in addition to radiologic findings [Tables 3 and 4].
Due to the difficulty in visualizing pharyngeal Fbs without the use of flexible or rigid endoscopy, early consultation is advisable. [23] Furthermore; removal attempts are often difficult and are complicated by the gag reflex. In order to protect the airways, most Fbs in the throat, therefore, require otolaryngology intervention with sedation and endoscopic removal. [25,31] Complications may include airway obstruction, laryngeal edema, and pushing the foreign body into the subglottic space, esophagus, or trachea. [25,31]
In our environment, patients can present quite late postforeign body insertion [Figure 1], making removal more cumbersome and even complication prone. The overall incidence of complications in this study (51/594 8.6%) had a strong correlation with the duration of lodgement of Fbs prior to presentation (R = 0.9359; R2 = 8759) [Figure 2]. This is very likely due to migration (self or induced) of such lodged Fbs when left for a longer period. Peristalsis waves and attempts by patient at dislodging the Fb as an inherent defense mechanism for Fbs within the air and food passages readily occurs. Patients sometimes ingest abnormally large “food bolus” in an attempt at dislodging such throat Fbs like fish bones. This is most often counterproductive and can lead to laceration and perforation injuries of viscus. Foreign body reactions, inflammatory responses and infections; often results in prolonged Fb lodgements within ears and nose. Again, the complications seen in our series among early presentations were basically those cases that had previous failed removal attempts carried out by nonspecialists prior to referral. This highlights the need to rapidly engage skilled and experienced specialists in the ENT clinic for timely management.
The retrospective nature of this study limits the data analyzed to that recorded in the case notes. [4,10,32] Patients were unavailable for follow-up after removal of the Fbs, so assessments after the acute phase could, therefore, not be carried out in those who may have required it. Another limitation was the lack of access to data from peripheral hospitals on the failure and complication rates in their management of Fbs.
Conclusion
Foreign bodies in ENT are common especially among children below 5 years. Majority of Fbs presented beyond 24 h and there was a strong correlation between duration of foreign body insertion and associated complications. Repeated failed attempts and delayed referrals to otorhinolaryngologists from peripheral centers were also contributing factors to increased morbidity and hence the need for awareness.
Acknowledgments
The Research was self-funded. We appreciate Dr. Agbor Ebuta of the Department of Family Medicine, and the staff of the Medical Records Department, Garki Hospital Abuja and University of Abuja Teaching Hospital, Gwagwalada for their assistance in the course of this study. Our special thanks go to Dr. Perpetua Ibekwe (Ph.D Medical Research) for the statistical analysis.
References
- Thompson SK, Wein RO, Dutcher PO. External auditory canal foreign body removal: Management practices and outcomes. Laryngoscope 2003;113:1912-5.
- Yuca K, Yuca SA, Caksen H. Aural live foreign bodies in children. J Emerg Med 2003;25:102-4.
- Ansley JF, Cunningham MJ. Treatment of aural foreign bodies in children. Pediatrics 1998;101:638-41.
- Ologe FE, Dunmade AD, Afolabi OA. Aural foreign bodies in children. Indian J Pediatr 2007;74:755-8.
- Kalan A, Tariq M. Foreign bodies in the nasal cavities: A comprehensive review of the aetiology, diagnostic pointers, and therapeutic measures. Postgrad Med J 2000;76:484-7.
- Burton AH, Balmain AR. Foreign bodies and nasal carriers of diphtheria. Lancet 1929;2:ii: 977.
- DeWeese DD, Saunders AH, editors. Acute and chronic diseases of the nose. In: Textbook of Otolaryngology. St. Louis: CV Mosby; 1982.
- Guthrie D. Foreign bodies in the nose. J Laryngol Otol 1956;41:454-7.
- Malhotra C, Arora MM, Mehra YN. An unusual foreign body in the nose. J Laryngol Otol 1930;45:73.
- Ngo A, Ng KC, Sim TP. Otorhinolaryngeal foreign bodies in children presenting to the emergency department. Singapore Med J 2005;46:172-8.
- Ijaduola GT, Okeowo PA. Foreign body in the ear and its importance: The Nigerian experience. J Trop Pediatr 1986;32:4-6.
- Bhattia PL. Aural and nasal foreign bodies. Niger Med Pract 1986;14:17-20.
- Mishra A, Shukla GK, Bhatia N. Aural foreign bodies. Indian J Pediatr 2000;67:267-9.
- Ibekwe TS, Nwaorgu OG, Onakoya PA, Ibekwe PU. Paediatric otorhinolaryngology emergencies: A tropical country’s experience. Emerg Med Australas 2007;19:76-7.
- Fasunla J, Ibekwe T, Adeosun A. Preventable risks in the management of aural foreign bodies in Western Nigeria. Internet J Otorhinolaryngol 2006;7:1-4. Available from: https://ispub.com/IJORL/7/1/9424.
- Ologe FE. Traumatic perforation of the tympanic membrane in Ilorin, Nigeria. Niger J Surg 2002;8:9-12.
- Asif M, Shah SA, Khan F, Ghani R. Analysis of tracheobronchial foreign bodies with respect to sex, age, type and presentation. J Ayub Med Coll Abbottabad 2007;19:13-5.
- Alberti PW. Epithelial migration on the tympanic membrane. J Laryngol Otol 1964;78:808-30.
- Goldstein E, Gottlieb MA. Foreign bodies in nasal fossae of children. Oral Surg Oral Med Oral Pathol 1973;36:446-7.
- Walby AP. Foreign bodies in ear, nose and throat. In Kerr AG, Editor Scott Brown´s Otolaryngology 6th ed. Vol. 6 Oxford : Butterworth Heinemann; 1997. p. 1-3.
- Golding IM. An unusual cause of bromidrosis. Pediatrics 1965;36:791-2.
- Harner SG. Foreign bodies in the ear, nose, and throat. Postgrad Med 1975;57:82-3.
- Heim SW, Maughan KL. Foreign bodies in the ear, nose, and throat. Am Fam Physician 2007;76:1185-9.
- Bloom DC, Christenson TE, Manning SC, Eksteen EC, Perkins JA, Inglis AF, et al. Plastic laryngeal foreign bodies in children: A diagnostic challenge. Int J Pediatr Otorhinolaryngol 2005;69:657-62.
- Esclamado RM, Richardson MA. Laryngotracheal foreign bodies in children. A comparison with bronchial foreign bodies. Am J Dis Child 1987;141:259-62.
- Robinson PJ. Laryngeal foreign bodies in children: First stop before the right main bronchus. J Paediatr Child Health 2003;39:477-9.
- Berkowitz RG, Lim WK. Laryngeal foreign bodies in children revisited. Ann Otol Rhinol Laryngol 2003;112:866-8.
- Gautam V, Phillips J, Bowmer H, Reichl M. Foreign body in the throat. J Accid Emerg Med 1994;11:113-5.
- Kumar M, Joseph G, Kumar S, Clayton M. Fish bone as a foreign body. J Laryngol Otol 2003;117:568-9.
- Silva AB, Muntz HR, Clary R. Utility of conventional radiography in the diagnosis and management of pediatric airway foreign bodies. Ann Otol Rhinol Laryngol 1998;107:834-8.
- Puhakka H, Svedström E, Kero P, Valli P, Iisalo E. Tracheobronchial foreign bodies. A persistent problem in pediatric patients. Am J Dis Child 1989;143:543-5.
- Schulze SL, Kerschner J, Beste D. Pediatric external auditory canal foreign bodies: A review of 698 cases. Otolaryngol Head Neck Surg 2002;127:73-8.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.