Acute Osteomyelitis as Cause of Late Sepsis in a Nigerian Neonate
- *Corresponding Author:
- Dr. Josephat Chinawa
Department of Pediatrics, University of Nigeria Teaching Hospital, Ituku Ozalla, Enugu State University Teaching Hospital, Enugu, Nigeria
E-mail: josephat.chinawa@ unn.edu.ng
Citation: Odetunde OI, Aderibigbe AO, Chinawa JM, Odetunde OA, Okenwa WO, Onyemaechi Ndubisi OC. Acute osteomyelitis as cause of late sepsis in a Nigerian neonate. Ann Med Health Sci Res 2014;4:968-70.
Abstract
Neonatal osteomyelitis (NO) is said to be rare and uncommonly reported in the sub‑region. Although this may be true, either because the cases are under‑diagnosed, unreported or under‑reported. The diagnosis is clinical and supported with blood culture or the aspiration of pus with radiological findings. We report a case of a neonate with acute osteomyelitis of the right femur, diagnosed at 10th day of life, which was confirmed with blood culture and radiogram findings of the right upper thigh of the baby. To the best of our knowledge, this is the first documented reported case of NO from the south‑eastern Nigeria. It is imperative to recognize the clinical presentation necessary to raise the suspicion of NO and other focal infection in the newborn. With thorough examination and selected investigation the focus of infection in the neonate can be detected.
Keywords
Neonatal, Nigeria, Osteomyelitis, Septicemia
Introduction
Neonatal bone and joint infection are said to be infrequent and uncommonly reported in the sub-region.[1] The first few medical literatures from Nigeria dated back to about three decades ago[1-4] and since then there has been a paucity of reports on this disease from the sub-region. Although the rarity may be true, either because the cases are under-diagnosed, unreported or under reported.
Neonatal osteomyelitis (NO) and septic arthritis may result from hematogenous seeding in the course of bacteremia or direct extension from a skin infection after a latent period of about 1–3 weeks.[5] The usual site of osteomyelitis is a metaphyseal abscess in a long bone but the flat bone of the pelvis, scapula, rib, or craniofacial skeleton can be affected and spread occurs readily through the cortex, to form a sub-periosteal and soft tissue abscess and through the growth plate to the adjacent joint cavity.[5] The predisposing factors for NO include prematurity, skin or umbilical sepsis, Cesarean section delivery, significant jaundice, and systemic infections such as pneumonia or meningitis.
Some important factors in the pathogenesis of osteomyelitis include the virulence of the infecting organism, underlying disease, immune status of the host, and the type, location, and vascularity of the bone.[6] The pathogenesis of this disease includes vessel occlusion, leading to tissue ischemia, infarction and bone marrow hyperplasia.[7] Bone marrow hyperplasia results in widening of the medulla and subsequent cortical thinning. This results in coarsening of the normal trabecular pattern, with the loss of cortico-medullary differentiation in both long and flat bones.[7]
Early diagnosis of NO might be difficult because of the paucity of clinical signs and symptoms, but has to be included in the differential diagnosis when late-onset or prolonged neonatal sepsis is present, as outcome is dependent on rapid diagnosis and immediate start of treatment.[5,8] Several studies have documented poor outcome even with the advance in anti-microbial therapy. NO can lead to permanent joint disability, disturbances in bone growth resulting from damage to the cartilaginous growth plate, limb-length discrepancies and pathological fractures.[5]
This report highlights the fact that osteomyelitis is not an uncommon manifestation of septicemia in neonate and to break the silence of about three decades of no medical literature on the disease in the sub-region, we also review the available literature from the sub-region.
Case Report
Baby C.O was a 72 h old term out-born (delivered in the peripheral rural hospital) neonate on admission at Newborn special baby Care Unit Enugu State University Teaching Hospital, Parklane, Enugu. He was a product of singleton uneventful pregnancy, baby’s mother is a multi-parous woman with a positive history of premature rupture of membrane and prolonged labor with prolonged rupture of membrane but no history suggestive of maternal fever prior to the delivery. C.O was delivered by Breach spontaneous vertex and had poor cry at birth. He presented with fever, fast breathing, refusal of feeds, and two episodes of seizure, all of 48 h durations. Examination revealed a full term neonate, dusky, febrile (Temperature of 38.9°C), Grunting with intercostals recession, respiratory and heart rate of 88/cycles and 174/beats respectively. Birth weight of 2.7 kg length of 45 cm (percentile) and head circumference of 34 cm. Abdominal examination revealed an unkempt umbilical stump with no organomegaly. The anterior fontanel was patent and normotensive with poor cry and motor activities on stimulation. The muscle tone was remarkably decreased, and primitive reflexes depressed. The random blood glucose was 102 mmol/dl.
A provisional diagnosis of perinatal asphyxia with presumed neonatal septicemia was made.
The initial management was nil per oral, intravenous (IV) infusion, antibiotics (IV ampicillin/sulbactam and genticin) and anticonvulsant (IV phenobarbitone).
The CBC showed a packed cell volume of 34%, total white blood count of 19.8 × 109/L, predominately neutrophilia of 70% and immature to total neutrophil ratio of 0.4 and erythrocytes sediment rate of 10 mm/1st h (Westergren).
Review after 72 h into admission show a remarkable improvement with resolution of the seizure and respiratory distress, but the temperature spikes continued. And antibiotic was then changed to third-generation cephalosporin (IV ceftazidime).
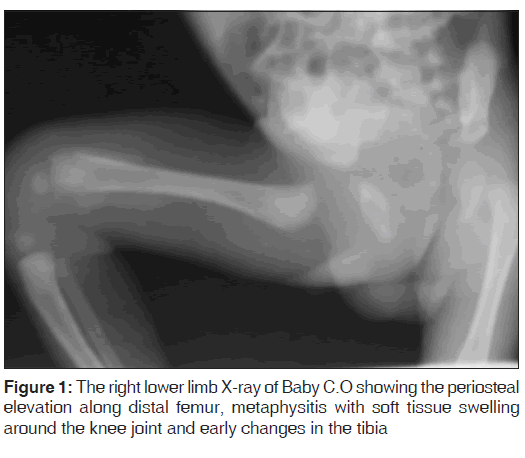
The fever persisted till 10th day of admission (13th day of life), and additional findings were limitation of movement of the right lower limb with warm, tender swelling of the distal thigh. Radiological examination of the right thigh showed significant periosteal reaction along the distal femur, metaphysitis with soft tissue swelling around the knee joint and early changes in the tibia [Figure 1]. A diagnosis of NO was made on the 10th day of hospitalization, supported with blood culture yield of Staphylococcus aureus, sensitive to vancomycin and chlydamycin and radiological findings. Baby C.O was treated with IV vancomycin and was discharge home without complication after 4 weeks of hospitalization on oral chlydamycin to be followed-up at the pediatric and orthopedic out-patient clinic.
Discussion
This report highlights the fact that NO is not a rare manifestation of septicemia in neonate, and it is important to recognize the clinical presentation of the disease necessary to raise the suspicion in the newborn. Our index patient presented with late onset neonatal septicemia with significant antecedent history of perinatal asphyxia and premature rupture of membrane. History of perinatal asphyxia, prolonged rupture of membranes and transplacental infection has been described as risk factors for neonatal NO.[4,8] Baby C.O presented on the 4th day of life and the diagnosis of NO was not made until the 13th day of life with the evolution of the disease that necessitate a prolonged hospital stay. The diagnosis of NO in this baby was based on clinical signs and symptoms, laboratory findings, radiological well as positive blood culture.
Diagnosis of osteomyelitis in the neonate can be challenging and is often delayed as it is rare in the neonatal period and frequently presents with non-specific signs of illness.[9] The blood culture result of the index patient yielded S. aureus, which is in consonance with the common etiopathological agent cultured in most literatures.[9-11] The X-ray of the affected limb confirmed the suspicion of NO in this baby, defined the infection site, differentiated between unifocal and multifocal disease patterns and ruled out secondary complications. Plain radiography can show soft tissue swelling and distorted fascial planes within days after onset of infection, but may be subtle and not obvious until day 5–7 in children.[12] Early changes on X-ray includes periosteal thickening or elevation, lytic lesions, osteopenia, loss of trabecular architecture, and new bone deposition, joint effusions and destructive bone changes appearing around 7–14 days of the disease.[13,14] In our index patient, X-ray of the limb was done on the 13th day of life (the 9th day of the illness). The findings were lytic lesions, osteopenia, loss of trabecular architecture, and new bone apposition, joint effusions and destructive bone changes. Antimicrobial treatment is frequently administered IV for 2–3 weeks and then switched to oral medication.[12,15] Baby C.O had 4 weeks of IV antibiotics, 2 weeks of oral and discharge home without any secondary complications. Longtime hospital admission is common morbidity associated with NO.[4-7,15]
Conclusion
To the best of our knowledge, this is the first reported case from the sub-region after a silent period of about three decades.
It is important to recognize the clinical presentations necessary to raise the suspicion of osteomyelitis and other focal infections in the newborn. Thorough clinical examination and selected investigations are paramount in localizing the focus of infection in neonates.
References
- Omene JA, Odita JC. Clinical and radiological features of neonatal septic arthritis. Trop Geogr Med 1979;31:207-12.
- Omene JA, Odita JC, Okolo AA. Neonatal osteomyelitis in Nigerian infants. Pediatr Radiol 1984;14:318-22.
- Akindele JA. Klebsiella Septicaemia with associated osteomyelitis and arthritis in neonates. Niger J Pediatr 1986;2:59-64.
- Adeyemo AA, Akindele JA, Omokhodion SI. Klebsiella septicaemia, osteomyelitis and septic arthritis in neonates in Ibadan, Nigeria. Ann Trop Paediatr 1993;13:285-9.
- Gutierrez K. Bone and joint infections in children. Pediatr Clin North Am 2005;52:779-94, vi.
- Ejindu VC, Hine AL, Mashayekhi M, Shorvon PJ, Misra RR. Musculoskeletal manifestations of sickle cell disease. Radiographics 2007;27:1005-21.
- Newman LG, Waller J, Palestro CJ, Schwartz M, Klein MJ, Hermann G, et al. Unsuspected osteomyelitis in diabetic foot ulcers. Diagnosis and monitoring by leukocyte scanning with indium in 111 oxyquinoline. JAMA 1991;266:1246-51.
- Liao SL, Lai SH, Lin TY, Chou YH, Hsu JF. Premature rupture of the membranes: A cause for neonatal osteomyelitis? Am J Perinatol 2005;22:63-6.
- Dessì A, Crisafulli M, Accossu S, Setzu V, Fanos V. Osteo-articular infections in newborns: Diagnosis and treatment. J Chemother 2008;20:542-50.
- Ish-Horowicz MR, McIntyre P, Nade S. Bone and joint infections caused by multiply resistant Staphylococcus aureus in a neonatal intensive care unit. Pediatr Infect Dis J 1992;11:82-7.
- McPherson DM. Osteomyelitis in the neonate. Neonatal Netw 2002;21:9-22.
- Pineda C, Espinosa R, Pena A. Radiographic imaging in osteomyelitis: The role of plain radiography, computed tomography, ultrasonography, magnetic resonance imaging, and scintigraphy. Semin Plast Surg 2009;23:80-9.
- KothariNA, PelchovitzDJ, MeyerJS. Imaging of musculoskeletal infections. Radiol Clin North Am 2001;39:653-71.
- BlickmanJG, van DieCE, de RooyJW. Current imaging concepts in pediatric osteomyelitis. Eur Radiol 2004;14 Suppl 4:L55-64.
- Faust SN, Clark J, Pallett A, Clarke NM. Managing bone and joint infection in children. Arch Dis Child 2012;97:545-53.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.