An Audit of Malignant Oro‑facial Tumors Presenting at a Tertiary Hospital in Lagos
- *Corresponding Author:
- Dr. Gbotolorun OM
Department of oral and maxillofacial Surgery, Faculty of Dental Sciences, College of Medicine, University of Lagos, Lagos, Nigeria.
E-mail: lekangbotol@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Oro‑facial malignancies are reported to have a high mortality and morbidity, this is further worsened when patient report late. To analyze the malignant oro‑facial lesions seen at a Hospital in the Lagos, Nigeria. Successive patients that presented in the hospital and met criteria of study during 15 months period were recruited into the study. Demographics, clinical variables, and treatment provided for each patient in the hospital was recorded. Data collected were presented as tables and percentages. There were 36 cases seen, their ages ranged from 10 to 72 years (median 49 years), and there were 21 males and 15 females. Time lapse before presentation to the clinic ranged from 2 to 30 months, mean (9.9 (±5.5 months and the largest dimension of lesions at presentation ranged from 2 cm to 12 cm (mean 6.4 ± 2.0 cm). Most common site of presentation was posterior tongue (16.7%; 6/36) and Squamous cell carcinoma (41.6%; 15/36) was the most common histopathologic diagnosis. Twenty‑three patients (63.9%; 23/36) had primary surgeries in the hospital. Patients seen in this case series generally reported late with large lesions.
Keywords
Malignant, Orofacial, Tumours
Introduction
Oro-facial malignancies are malignant neoplasms of the oral cavity and adjacent structures excluding the facial skin cancers.[1] Approximately, 90% of these cancers are reported to be squamous cell carcinoma (SCC).[2] Oro-facial malignancies exhibit geographic variations in prevalence and pattern due to cultural, social, occupational, or climatic factors.[3,4]
The prognosis of oro-facial malignancies is relatively poor; thus they are a public health concern in different parts of the world.[5-8] Treatment of patients presenting late presents further challenges, often resulting in disfigurement and/or impairment of basic functions such as talking, swallowing, eating, and breathing.[9] The treatment and outcome of these lesions are usually determined by the extent of spread/stage of the disease at presentation.[10,11]
The aim of this study was to analyze the types of oro-facial malignancies, patients’ exposure to risks factors, site and size of lesions on presentation, and treatment administered during their stay in the hospital.
Subjects and Methods
Consecutive patients that presented in the oral and maxillofacial outpatients clinic of the Lagos University Teaching Hospital with oro-facial malignancies during 15 months period extending from October 2012 to December 2013 and agreed to be part of the study were recruited into this survey. After informed consent was obtained, one of the reseachers (ECI) recorded demographics and clinical variables from each patient. Treatment provided for each patient in the hospital was also recorded. Data were presented as ranges, percentages, median, means, and standard deviation (to represent central tendencies) and tables as appropriate.
Results
There were 36 cases of oro-facial malignancies seen in the period. Ages ranged between 10 and 72 years (median of 49 years), with 21 males and 15 females (male:female; 1.4:1). Nineteen (52.8%; 19/36) subjects smoked tobacco, 12 of these took both alcohol and smoked tobacco. The length of time before presenting to the hospital ranged from between 2 and 30 months (mean 9.9 ± 5.5 months). The largest diameter of the lesions at presentation ranged from 2 cm to 12 cm (mean 6.4 ± 3.0 cm). The most common sites of presentation were posterior tongue with 6 patients presenting (16.7%; 6/36); others included the palate (13.9%; 5/36), the floor of the mouth and the mandibular alveolus which both had 4 (11.1%; 4/39) patients [Table 1].
| Histolopathological types | Tongue | Mandibular alveolus | Floor of mouth | Retomolar area | Cheek Palate | Maxillary antrum | Submandibular area | Parotid area | Upper lip | Mandible | Maxilla | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Squamous cell | 6 | 4 | 3 | 1 | 1 | 15 | |||||||
| carcinoma | |||||||||||||
| Adenocysticca | 1 | 3 | 1 | 1 | 6 | ||||||||
| Mucoepidermoid | 1 | 2 | 3 | 1 | 7 | ||||||||
| carcinoma | |||||||||||||
| Adenocarcinoma | 1 | 1 | 2 | ||||||||||
| Basal cell | 1 | 1 | |||||||||||
| carcinoma | |||||||||||||
| Osteosarcoma | 1 | 1 | |||||||||||
| Rhabdosarcoma | 1 | 1 | |||||||||||
| Fibrosarcoma | 1 | 1 | |||||||||||
| Ameloblasticca | 1 | 1 | |||||||||||
| Carcinoma | 1 | 1 | |||||||||||
| expleomorphic | |||||||||||||
| Total | 6 | 4 | 4 | 1 | 3 | 5 | 4 | 3 | 2 | 2 | 1 | 1 | 36 |
Table 1: Histopathological types and sites of presentation of oro-facial malignant tumors
The most common histopathological diagnosis was SCC (41.7%; 15/36), others included mucoepidermoid carcinoma (19.4%; 7/36), and adenocystic carcinoma which was the diagnosis in (6/36; 16.7%) patients. All lesions that presented on the tongue (16.7%; 6/36) and the mandibular alveolus (11.1%; 4/39;) were SCC, whereas none of the lesions that presented on the palate, parotid and submandibular gland were with SCC [Table 1]. Twenty-five patients had clinically palpable nodes at presentation, with 14 (14/36; 38.9%) of the patients presenting with unilateral lymph nodes and 11 (11/36; 30.6%) with bilateral nodes. Eight lesions involved multiple nodal levels whereas 17 were confined to a single nodal level.
The most common levels were level 1 (13 cases; 36.1%), level 2 (11 cases; 30.6%) and level 3 (7 cases; 19.45). The largest neck node in 11 patients was < 3 cm; they were between 3 cm and 6 cm in 8 patients and > 6 cm in 5 patients. Only 4 (11.1%; 4/36) patients presented with distant metastasis, 3 patients had metastasis in the lungs whereas the 4th patient had metastasis both in the lungs and the liver. All patients with distant metastasis had lesions ≥ 8 cm in their largest diameter. Overall based on the tumor, node, and metastases (TNM) staging of tumors, 2 (5.5%) were classified as stage 2, 5 (13.9%) stage 3, 14 (38.9%) stage 4a, 11 (30.6%) stage 4b and 4 (11.1%) stage 4c tumors, respectively.
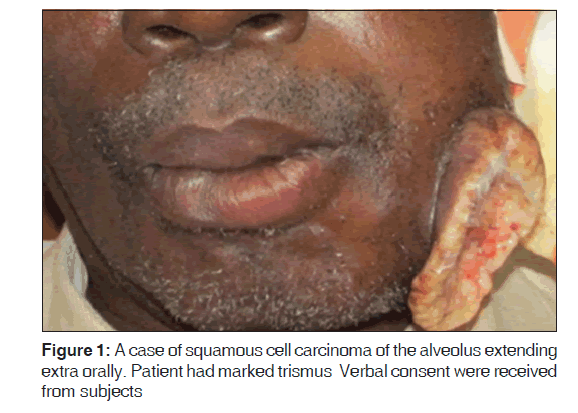
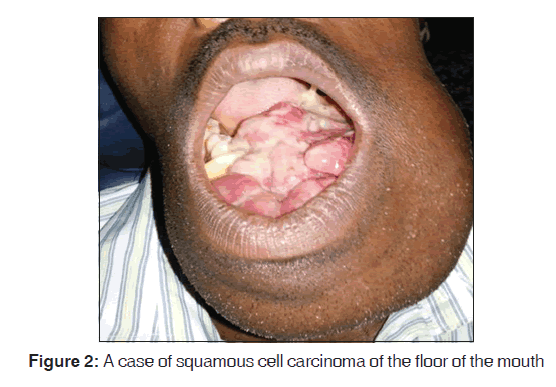
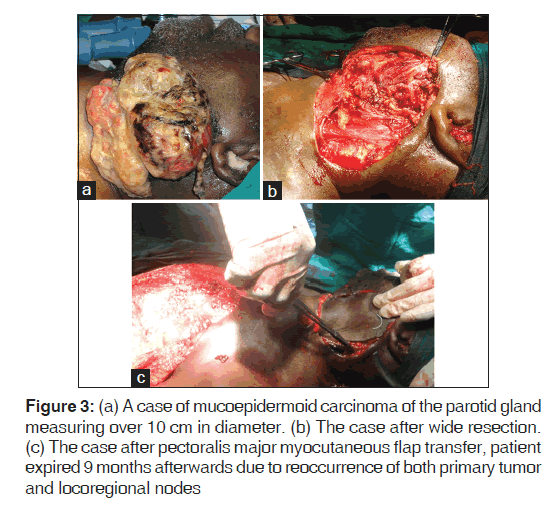
Twenty-three patients (63.9%) had primary surgeries done, others did not have surgery either due to the loss of patient to follow-up (5/36; 13.9%) or due to the lesions being classified as inoperable [Figures 1 and 2] and were sent for radiotherapy (8/36; 22.2%) alone. Only two patients who had primary surgery had intraoperative assessment for negative tumor margins with frozen section. Five (5/36; 13.9%) patients had neck dissections in conjunction with the removal of primary lesions in this series. Primary closure for soft tissue closure was used for most of the other lesions. Microvascular tissue transfer with the radial forearm microvascular flap was used for reconstruction for 1 case while three cases had reconstruction with the pectoralis major myocutaneous flap (PMMF) [Figure 3a-c]. The single radial forearm microvascular flap attempt failed while 2 of the attempts at PMMF were successful. All patients that had surgery were referred to the oncologist for adjunct radiotherapy and chemotherapy.
Figure 3: (a) A case of mucoepidermoid carcinoma of the parotid gland measuring over 10 cm in diameter. (b) The case after wide resection. (c) The case after pectoralis major myocutaneous flap transfer, patient expired 9 months afterwards due to reoccurrence of both primary tumor and locoregional nodes
Discussions
Oral SCC is reported to be the most common malignant tumor of the oro-facial region constituting between 70% and 90% of these lesions.[2] In this study, only 41.6% were SCCs. The lesions in this study showed site specificity in agreement with most researchers that report SCC to be most prevalent in the posterior tongue and mandibular retromolar region.[2,12] The median age of presentation in this study was 49 years this is comparable to a study in the same center which had a mean age of 42.2 years.[13] It is, however, lower than most studies in the in the western world, this difference in age of presentation has also been documented in other studies in Nigerians.[3,7,8] Tobacco, as documented in other studies, seems to also be to be an important risk factor in this series.[6,7,8,14] This is, however, is at variance with earlier reports by Oji and Chukwuneke,[3] in Enugu South Eastern Nigeria, who reported none of the 77 respondents with oral cancer in their study claiming to use neither tobacco nor alcohol.
Oro-facial cancers often present late in most studies in the western world.[7] The same scenario is reported in studies from Nigeria populations where most patients are reported to present at TNM stage 3 or 4.[3,15] Over 80% of patients in this study presented at the TNM stage 4 in consonance with earlier reports from the country.[3] The reason for this delay in presentation might be connected with a lack of awareness of the disease entities in the country and inadequate level of either clinic based or population based screening for the lesion.[7,16,17]
Eight patients (22.2%; 8/36) were not treated with claims of tumor being inoperable due to large size. Comparison in the sizes of tumors seen in these series with some in literature, however, showed that cases with larger sizes have been documented to have received primary surgeries.[18-20] The reason for the difference might however not be unconnected with the fact that microvascular free tissue transfer (free flap) for reconstruction after primary surgery was more readily available in such centers compared to ours. Furthermore, confirmation of negative tumor margins by frozen section was performed in only 2 (5.5%; 2/36) of the cases. The reason for this might not be unconnected to the cost of doing this.
Even though, microvascular free tissue transfer has had an exponential increase in the last two to three decades in the application for reconstruction of ablative defects of the head and neck,[21] this has not been the case in Nigeria.[22] The reason for this might not be unrelated to the cost of establishing centers with equipment for the free flap and also a lack of training fellowships for microvascular surgery as it is present in most developed countries. The only attempt at microvascular surgery in the series failed, and a salvage surgery had to be done.
Conclusion
Patients seen in this case series generally reported late with large lesions and treatment offered in the hospital was considered less than the optimal when compared to international standards. This might suggest that increased awareness of disease in the population and more infrastructures in the hospital are needed for optimal treatment for oro-facial malignancies in the hospital.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Arotiba GT, Ladeinde AL, Oyeneyin JO, Nwawolo CC, Banjo AA, Ajayi OF. Malignant orofacial neoplasms in Lagos, Nigeria. East Afr Med J 2006;83:62-8.
- Effiom OA, Adeyemo WL, Omitola OG, Ajayi OF, Emmanuel MM, Gbotolorun OM. Oral squamous cell carcinoma: A clinicopathologic review of 233 cases in Lagos, Nigeria. J Oral Maxillofac Surg 2008;66:1595-9.
- Oji C, Chukwuneke FN. Oral cancer in Enugu, Nigeria, 1998-2003. Br J Oral Maxillofac Surg 2007;45:298-301.
- Arotiba GT, Ladeinde AL, Arotiba JT, Ajike SO, Ugboko VI, Ajayi OF. Ameloblastoma in Nigerian children and adolescents: A review of 79 cases. J Oral Maxillofac Surg 2005;63:747-51.
- Weatherspoon DJ, Chattopadhyay A, Boroumand S, Garcia I. Oral cavity and oropharyngeal cancer incidence trends and disparities in the United States: 2000-2010. Cancer Epidemiol 2015;39:497-504.
- Demko CA, Sawyer D, Slivka M, Smith D, Wotman S. Prevalence of oral lesions in the dental office. Gen Dent 2009;57:504-9.
- Drugan C, Leary S, Mellor T, Bain C, Verne J, Ness A, et al. Head and neck cancer in the South West of England, Hampshire, and the Isle of Wight: Trends in survival 1996-2008. Br J Oral Maxillofac Surg 2013;51:19-24.
- Gupta B, Ariyawardana A, Johnson NW. Oral cancer in India continues in epidemic proportions: Evidence base and policy initiatives. Int Dent J 2013;63:12-25.
- Langevin SM, Michaud DS, Eliot M, Peters ES, McClean MD, Kelsey KT. Regular dental visits are associated with earlier stage at diagnosis for oral and pharyngeal cancer. Cancer Causes Control 2012;23:1821-9.
- Jansisyanont P, Blanchaert RH Jr., Ord RA. Intraoral minor salivary gland neoplasm: A single institution experience of 80 cases. Int J Oral Maxillofac Surg 2002;31:257-61.
- Akinbami BO, Omitola OG, Akadiri OA. Pattern of presentation and management of orofacial and neck soft tissue tumors in a Nigerian tertiary health center – A preliminary study. Intern Med Inside 2013;1:9.
- Chidzonga MM, Mahomva L. Squamous cell carcinoma of the oral cavity, maxillary antrum and lip in a Zimbabwean population: A descriptive epidemiological study. Oral Oncol 2006;42:184-9.
- Ajayi OF, Adeyemo WL, Ladeinde AL, Ogunlewe MO, Effiom OA, Omitola OG, et al. Primary malignant neoplasms of orofacial origin: A retrospective review of 256 cases in a Nigerian tertiary hospital. Int J Oral Maxillofac Surg 2007;36:403-8.
- Adewole RA. Alcohol, smoking and oral cancer. A 10-year retrospective study at Base Hospital, Yaba. West Afr J Med 2002;21:142-5.
- Gbotolorun OM, Bakare T, Olojede AC, Adeniyi A, Emeka CI, Adetayo AM, et al. A survey of of patients with oro-facial tumours in two tertiary hospitals in Lagos, Nigeria. Niger Med Pract 2014;66:3-5.
- Vijay Kumar KV, Suresan V. Knowledge, attitude and screening practices of general dentists concerning oral cancer in Bangalore city. Indian J Cancer 2012;49:33-8.
- Gbotolorun OM, Ayodele AS, Olojede AC, Adamson OO, Emeka CI, Amao AT. Knowledge and screening practices for oral cancers amongst general dental practitioners in Lagos, Nigeria. Afr J Biomed Res 2014;17:69-73.
- Okoturo E, Olubi O. An audit of cT4a head and neck cancer treatment: A preliminary study from a regional head and neck unit. Niger J Oral Maxillofac Surg 2014;1:21-6.
- Balasubramanian D, Thankappan K, Kuriakose MA, Duraisamy S, Sharan R, Mathew J, et al. Reconstructive indications of simultaneous double free flaps in the head and neck: A case series and literature review. Microsurgery 2012;32:423-30.
- Kawase-Koga Y, Mori Y, Saijo H, Hoshi K, Takato T. Reconstruction of a complex midface defect from excision of a squamous cell carcinoma, according to regional aesthetic units. Oral Surg Oral Med Oral Pathol Oral Radiol 2014;117:e97-101.
- Visse JH, Adendorff DJ, Malherbe WD. Free flap transfer with microvascular anastomosis. S Afr Med J 1976;50:2026-31.
- Okoturo E, Odebode OA, Erinoso OA, Naboya AN, Adesanya AA. Maxillary reconstruction with radial forearm fasciocutaneous free flap: A case presentation. Nig Q J Hosp Med 2014;24:150-4.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.