An Observational and Trend Analysis Study of Hand Hygiene Practices of Healthcare Workers at A Private Nigerian Tertiary Hospital
2 Department of Medical Microbiology, Jos University Teaching Hospital, Jos, Nigeria
3 Department of Medical Microbiology, Lagos University Teaching Hospital, Babcock University, Lagos, Nigeria
4 Department of Medical Microbiology, Babcock University, Ogun State, Nigeria
Citation: Shobowale EO, et al. An Observational and Trend Analysis Study of Hand Hygiene Practices of Healthcare Workers at A Private Nigerian Tertiary Hospital. Ann Med Health Sci Res. 2017; 7: 84-89
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
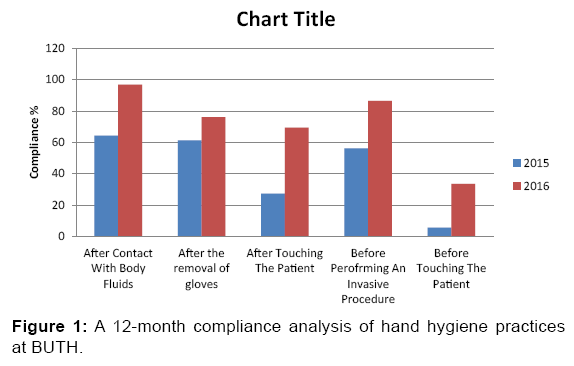
Background: Hand hygiene is a vital aspect of infection control and as such requires monitoring. Assessing compliance with hand hygiene and providing healthcare workers with feedback on their performance is important in any hospital hand hygiene improvement program. Aim: to investigate the degree of conformance with hand hygiene by healthcare personnel in a private tertiary hospital. Methods: a structured observational study to monitor conformance with hand hygiene during provision of patient care in a private health care facility in south west Nigeria, before and after institution of a hand-hygiene improvement campaign. Results: A total of 311 healthcare workers were observed from June 2015 to June 2016 with 1476 opportunities for hand hygiene. Improvements in hand hygiene occurred with a 33 % increase in compliance after contact with body fluids, 18% after the removal of gloves, 39% after touching the patient, 27% before performing an invasive procedure and 30% before touching the patient. Preoperative Nurses were 7.48 times more likely than the general population to wash their hands before patient contact [CI=3.1-18.73, X2=25.38], Critical care Units Staff were 0.34 times more likely to comply after contact with body fluids [CI=0.16-0.75, X2=6.15]. Conclusion: Measuring hand hygiene compliance is a veritable tool in hand hygiene compliance. Sustained educational programs and reminders serve to improve hand hygiene.
Introduction
Hand hygiene is an important aspect of Infection prevention and control (IPC) and its compliance requires measurement. Monitoring conformance with established hand hygiene parameters and providing healthcare personnel with results concerning their performance is a vital part of hand hygiene in the hospital setting. Observational surveys done covertly is one of the means of determining compliance. [1]
The transmission of microorganisms from the hands of hospital personnel is a huge source of infections and these can be readily prevented by staff conforming with laid down hand washing protocols such as the World Health Organization’s (WHO) five moments of hand hygiene. This is because unwashed personnel’s hands are the most common means for the transmission of pathogens from patient to patient and within the healthcare environment. [2]
Hand hygiene is therefore the easiest means for preventing the spread of pathogens with huge antimicrobial resistance potential and reducing rates of healthcare-associated infections. However, healthcare workers conformance with optimal practices has been observed to be low in most settings. [3]
These infections acquired in the hospital are a major cause of morbidity as well as mortality. Some studies have also shown that hand washing practices are persistently poor and sub optimal. It has also been challenging to show that hand washing practices can be easily improved and this has been attributed to difficulties associated with behavior modification among hospital staff. [4]
Adherence, with best practices for hand hygiene remains low but factors responsible for non-adherence have been identified and corrective actions proposed in some studies. The present guidelines propose the use of alcohol-based hand rub formulations where feasible in the absence of running water as the new standard of care, thus needing a system change in most hospitals. [5]
As a result, healthcare personnel education and encouragement have been proposed by some as key to change hand hygiene behavior in order to enhance conformance in hospitals. Improvement in compliance is associated with reduced infection rates and antimicrobial resistance.
Rational
Consistent hand hygiene is the sole most efficient tool available to prevent nosocomial infections. Daily hand hygiene opportunities and compliance for in-patients in our hospital are currently unknown. Hand hygiene literature is scarce in private tertiary hospitals in Nigeria. In order to establish a trend in compliance, a study thus needs to be performed and information on hand hygiene practice in such facilities will be collected and act as a baseline for developing interventions and assessing progress in compliance with best practices.
Aim
This study was intended to investigate the degree of conformance with hand hygiene and use of gloves by various categories of HCWs in a private tertiary hospital, and the factors that influence compliance to hand hygiene.
Objectives
Analyze the trends of hand hygiene practices over a 12 month period so as to determine behavioral patterns for hand hygiene and factors that contributed to compliance improvement or otherwise.
Methods
Study setting
The study was carried out at the Babcock University Teaching Hospital, a Private facility located in a rural setting. It is a 170 bed facility that caters for the health needs of undergraduate students of the institution and the immediate host community.
Study design
This was a structured observational study where we monitored conformance with hand hygiene during patient care at a teaching hospital in a sub-urban setting in south west Nigeria, before and during implementation of a hand-hygiene campaign. Two facility wide surveys were done six monthly with analyses of hand hygiene behavior in relation to profession, indication and shift.
From June 2015 till June 2016, HCWs in the hospital were covertly observed. The trained covert observer noted the number of opportunities for hand hygiene and the number of occasions for which the HCW complied with appropriate action. Adherence to standard precautions was evaluated.
Each event for hand hygiene or application of alcohol hand rubs or soap and water before or after patient contact was regarded as a hand hygiene opportunity. Any personnel who decontaminated his or her hands immediately after contact with a patient and then directly attended another patient without touching any object for example equipment, door handles or any other patient was considered to have complied with hand hygiene practice in relation to the second patient, same for the other moments of hand hygiene as determined by WHO. Hand hygiene compliance was expressed as a percentage, according to the formula.
Sample size determination
Assuming a compliance rate of 30% the sample size formula N=Z2pq//d2 gave a figure of 322 opportunities.
Data analysis
This was done using EPI INFO version 3.5.1 (CDC Atlanta) software. The Chi Square for Odds ratio was to test associations between variables and the Confidence Interval set at 95% with the level of significance being p< 0.05.
Data safety
All data collection was performed in a discrete manner and all information obtained were kept in the Principal Investigators computer and accessed only via a secure password.
Ethical approval was obtained from the Babcock University Teaching Hospital.
Results
In all 311 healthcare workers were observed over a two year period from June 2015 till June 2016. Most of these personnel were from the Surgery Department (30.2%) followed by the Critical Care Unit (17%) and the Emergency Department (16.7%). The year 2015 had 176 staff observed; there was a decline to 135 staff in 2016 due to a high staff turnover. The predominant staff observed were the Circulating Nurses (46.3%), next were the Anesthetists (10%), Surgeons and Residents (9%). Senior Nurses and Pre-operative Nurses were 8 and 7.4% respectively [Table 1].
| Variables | Frequency | Percent |
|---|---|---|
| A/E | 52 | 16.7 |
| CCU | 53 | 17.0 |
| Medicine | 59 | 19.0 |
| Paediatrics | 15 | 4.8 |
| Surgery | 94 | 30.2 |
| GOPD | 26 | 8.4 |
| Dental | 12 | 3.9 |
| Total | 311 | 100 |
| 2015 | 176 | 56.6 |
| 2016 | 135 | 43.4 |
| Compliance rate | 812/1476 | 55.01 |
| Total | 311 | 100 |
| Anesthesiologist | 31 | 10 |
| Senior Nurse | 25 | 8.0 |
| Circulating Nurse | 144 | 46.3 |
| Surgeon | 28 | 9.0 |
| Medical Student | 2 | 0.6 |
| Resident | 28 | 9.0 |
| Dental Technologist | 2 | 0.6 |
| Pre-operative Nurse | 23 | 7.4 |
| Medical Officer | 3 | 1.0 |
| Post-operative Nurse | 18 | 5.8 |
| Surgical technologist | 7 | 2.3 |
| Total | 311 | 100 |
Table 1: Distribution of participants by wards, years and specialty.
Regarding compliance with hand hygiene the Pre-operative Nurses were 7.48 times more likely than the general population to wash their hands before patient contact [CI=3.1-18.73, X2=25.38], Senior Nurses were also 3.8 times more likely to observe hand hygiene before contact with patients [CI=1.2- 16.11, X2=7.66]. The only group that observed hand hygiene after patient contact was again the pre-operative nurses [CI=1.79-14.8, X2=10.73]. The Pre-operative Nurse was also found to be 4.04 times more likely to perform hand hygiene before performing an invasive procedure [CI=1.27-29.3, X2=4.96] [Table 2].
| Personnel | Hand Hygiene Activity(%) | p value | AOR | 95% CI | ×2 | |
|---|---|---|---|---|---|---|
| Before contact with the patient | ||||||
| Compliant | Non-compliant | |||||
| Pre-op Nurse | 13 (56.5) | 10 (43.5) | 0.00 | 7.48 | 3.1-18.73 | 25.38 |
| 42 (14.7) | 244 (85.3) | |||||
| Resident Doctor | 13 (52) | 12 (48) | 0.08 | 0.48 | 0.21-1.12 | 3.13 |
| 194 (69.3) | 86 (30.7) | |||||
| Circulating Nurse | 16 (11.3) | 126 (88.7) | 0.006 | 0.42 | 0.22-0.78 | 7.66 |
| 39 (23.4) | 128 (76.6) | |||||
| Senior Nurse | 22 (88) | 3 (12) | 0.02 | 3.8 | 1.2-16.11 | 5.1 |
| 185 (66) | 95 (34) | |||||
| After Contact with the patient | ||||||
| Pre-op Nurse | 18 (78.3) | 5 (21.7) | 0.001 | 4.78 | 1.79-14.8 | 10.73 |
| 123 (44.3) | 164 (55.7) | |||||
| After Contact with body fluids | ||||||
| Anesthesiologist | 9 (42.9) | 12 (57.1) | 0.00 | 0.13 | 0.05-0.33 | 24.0 |
| 193 (85.8) | 32 (14.2) | |||||
| Pre-op Nurse | 20 (95.2) | 1 (4.8) | 0.08 | 4.71 | 0.83-101 | 2.68 |
| 182 (80.9) | 43 (19.1) | |||||
| After the use of gloves | ||||||
| Senior Nurse | 22 (88) | 3 (12) | 0.02 | 3.8 | 1.16-6.94 | 6.14 |
| 185 (66) | 95 (34) | |||||
| Pre-op Nurse | 19 (82.6) | 4 (17.4) | 0.11 | 2.37 | 0.83-8.33 | 2.47 |
| 188 (66.7) | 94 (33.3) | |||||
| Before Conducting an Invasive Procedure | ||||||
| Pre-op Nurse | 20 (90.9) | 2 (9.1) | 0.03 | 4.64 | 1.27-29.3 | 4.96 |
| 187 (68.2) | 87 (31.8) | |||||
| Resident | 15 (53.6) | 13 (46.4) | 0.05 | 3.92 | 0.21-1.00 | 0.46 |
| 183 (68.3) | 85 (31.7) | |||||
| Surgeon | 24 (85.7) | 4 (14.3) | 0.05 | 2.78 | 1.0-9.63 | 3.65 |
| 183 (68.3) | 85 (31.7) | |||||
| AOR = Adjusted Odds Ratio, CI = Confidence Interval, X2= Chi Square | ||||||
Table 2: Compliance of healthcare personnel with hand hygiene.
In terms of departmental compliance the Critical care Units Staff were 0.34 times more likely to comply after contact with body fluids [CI=0.16-0.75, X2=6.15]. The Internal Medicine Department, Surgery and Emergency rooms were also compliant with hand hygiene after patient contact [CI=1.03-3.25, 1.15- 3.02 and 0.20-0.76 respectively]. In addition the surgeons were 2.05 times more likely to perform hand hygiene before carrying out an invasive procedure [CI=1.15-3.72, X2=5.97] and also 0.59 times to wash hands after the removal of gloves before performing another task [CI=0.35-0.98, X2=4.27] [Table 3 and Figure 1].
| Department | Hand Hygiene Activity(%) | p value | AOR | 95% CI | X2 | |
|---|---|---|---|---|---|---|
| Compliant | Non-compliant | |||||
| After Contact with body fluids | ||||||
| CCU | 25 (73.7) | 13 (26.3) | 0.004 | 0.34 | 0.16-0.75 | 8.15 |
| 177 (85.1) | 31 (14.9) | |||||
| After Contact with the patient | ||||||
| CCU | 18 (34) | 35 (66) | 0.06 | 0.56 | 0.30-1.04 | 3.41 |
| 123 (47.9) | 134 (52.1) | |||||
| Medicine | 34 (58.6) | 25 (41.4) | 0.04 | 1.83 | 1.03-3.25 | 4.32 |
| 107 (42.7) | 144 (57.3) | |||||
| Surgery | 53 (56.4) | 41 (43.6) | 0.01 | 1.88 | 1.15-3.02 | 6.44 |
| 88 (41.3) | 125 (58.7) | |||||
| A/E | 14 (27.5) | 37 (72.5) | 0.00 | 0.40 | 0.20-0.76 | 7.98 |
| 123 (48.2) | 132 (51.8) | |||||
| Before conducting an invasive procedure | ||||||
| Paediatrics | 6 (40) | 9 (60) | 0.009 | 0.27 | 0.09-0.77 | 6.71 |
| 201 (71.5) | 80 (28.5) | |||||
| Surgery | 74 (79.6) | 19 (21.4) | 0.01 | 2.05 | 1.15-3.72 | 5.97 |
| 133 (65.5) | 70 (34.5) | |||||
| After the use of gloves | ||||||
| Paediatrics | 3 (20) | 12 (80) | 0.04 | 0.28 | 0.08-1.00 | 4.11 |
| 138 (46.8) | 157 (53.2) | |||||
| Surgery | 56 (59.6) | 38 (41.4) | 0.04 | 0.59 | 0.35-0.98 | 4.27 |
| 137 (63.1) | 80 (36.9) | |||||
| A/E | 21 (44.7) | 26 (55.3) | 0.00 | 0.31 | 0.16-0.59 | 13.65 |
| 186 (72.1) | 72 (27.9) | |||||
Table 3: Compliance of departments with hand hygiene.
Discussion
Conformance with hand hygiene is an effective preventive measure with respect to hospital infection control. Many of such infections are caused by pathogens transmitted from one patient to another by the hands of health care workers who have not washed their hands between patient care or who do not practice control measures such as use of hand disinfection with alcohol based preparation or glove use. [6-8]
The average compliance rates with hand hygiene recommendations varies between hospital wards, among professional categories of health-care workers, working conditions and definitions used in various studies. Compliance is estimated as being less than 50% which is less than the 55% obtained in our facility. [6]
Education, feedback intervention and patient awareness programs have had varying results with improvement in conformance. With the introduction of wall located dispensers containing an alcohol-based waterless hand washing antiseptic, significantly higher hand washing rates among health care workers have been observed. [9]
Our data and those of other researchers show that hands become progressively contaminated with commensal flora and potential pathogens during routine care, we therefore need to identify activities that are at higher risk for hand contamination and step up surveillance in those instances. [10]
Limited access to hand hygiene supplies, such as sinks, soap, or alcohol-based hand rub solutions are challenges towards conformance. This also includes the inconvenient location of hand wash sinks that make hand washing a mentally challenging task for health care workers and places a burden on them. [11]
Physicians adherence to hand hygiene is tied to workload constraints and possibly years of practice and exposure to educational programs. Strengthening a positive work culture attitude toward hand hygiene and reinforcing the conviction that each staff can influence group behavior may also improve adherence among physicians. [12]
Our data indicate that hand hygiene practice in the Critical Care Unit is sub-optimal as a consequence of a break in communication of infection control recommendations, insufficient promotion and enforcement of agreed research-based infection control practices, and a deficiency in infection control education. The current methods of communicating infection control recommendations have a limited effect on compliance rates in the CCU and are not evaluated adequately. [13]
We observed distinctly high rates of compliance of nurses towards hand hygiene which is also similar to the findings of researchers in Taif, Saudi Arabia where they identified team work and leadership as key factors that enhanced compliance in their cohort of nurses studied. Indeed it has been proven that nursing personnel are more compliant with hand hygiene than physicians as evidenced by a study from Nair et al in India who showed that nursing students were more compliant with hand hygiene when compared to medical students. [14,15]
Hand hygiene is recommended before performing invasive procedures and after overt or covert microbial contamination. Guidelines must be clear and easy for HCW’s in our environments to follow for them to become the norm in practice. Thus guidelines are needed that are easy to apply and reproducible across hospital such as in our cases that have a high volume and traffic of patients. [16]
In addition, the use of reminders or asking patients to remind staff of the need to conduct hand washing can have a sustained effect in enhancing compliance. The feedback of performance in our scenario leads to an improvement in compliance. This has been described in other settings and shown to increase the levels of compliance, however if the feedback is not repeated regularly, then this effect is not sustained. [17]
The provision of hand rubs close to patient beds has led to an increase in the frequency with which staffs cleanse their hands. Multipronged approaches which combine education with written material, reminders and continued feedback of performance can have an important effect on hand washing compliance and rates of hospital-acquired infection. [5,17,18]
Intensive hand washing promotion has been demonstrated in some studies to go as far as reducing diarrheal infections. To determine whether less intensive, more scalable interventions can improve health Bowen et al evaluated a school-based hand washing program. They randomized 87 Chinese schools to usual practices: with positive results seen. [19]
Good hand hygiene also reduces the spread of infections in the community. This is important because there is a dynamic flow between the hospital and the community. Alcohol-based hand sanitizers therefore come in handy in providing a convenient easy and cheap means of compliance. [20]
Direct contact between patients and healthcare workers who are transiently contaminated with nosocomial pathogens is believed to be the primary route of transmission for several organisms and can lead to patients becoming colonized or infected. A review of hand hygiene studies by the World Health Organization (WHO) found that baseline compliance with hand hygiene among healthcare workers was on average only 38.7%. [21,22]
Another study that adapted a multipronged approach on hand hygiene education showed that with system change, feedback evaluation and continuous reminders there can be up to 60% improvement in hand hygiene compliance rates as well as a reduction in MRSA infections in the hospital. [23,24]
The use of covert observers such as in our hospital has regularly pointed to nurses as the drivers of hand hygiene compliance. Dan and co-workers also showed nurses to have higher compliance rates and suggested them as ambassadors of hand hygiene programs. Getting it right with healthcare workers will markedly reduce the rates of HAI’s. [25-28]
Interventions: after the use of covert observers to collect data we presented our preliminary findings to the University Teaching Hospital at the Global Hand Washing Day. We also played video demonstrations of good hand hygiene techniques to the hospital staff, made posters on hand hygiene available all over the hospital and ensured that alcohol hand rubs were in sufficient quantity in all the wards. We put in place a system where once the alcohol hand rubs were exhausted the Infection control link nurses were notified and they made sure the in house pharmacy re stocked immediately.
Recommendations
From our findings we recommend the use of covert non identified observers on a periodic basis to assess the rates of hand hygiene compliance in our hospitals and the feedback of these results to departments and units as a means of inducing behavior change with regards to hand hygiene. With concerted efforts the compliance rates may improve over time.
Conclusion
Monitoring and measuring hand hygiene compliance is a veritable tool in hand hygiene improvement programs. Sustained educational programs and reminders serve to improve hand hygiene compliance among hospital personnel.
Acknowledgements
The authors wish to acknowledge the immense support of the Director of Clinical Services BUTH in actualizing this research.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Boyce JM. Measuring healthcare worker hand hygiene activity: Current practices and emerging technologies. Infection Control & Hospital Epidemiology. 2011;32:1016-1028
- Pittet D, Mourouga P, Perneger T. Compliance with hand washing in a teaching hospital. Ann Intern Med 1999; 130:126-130.
- Allegranzi B, Pittet D. Role of hand hygiene in healthcare-associated infection prevention.Journal of Hospital Infection. 2009; 73:305-315
- Simmons B, Bryant J, Neiman K, Spencer L, Arheart K. The role of hand washing in prevention of endemic intensive care unit infections. Infection Control & Hospital Epidemiology.1990;11:589-594
- Pittet D. Hand hygiene: Improved standards and practice for hospital care. Current Opinion in Infectious Diseases. 2003; 6:327-335
- Pittet D. Improving adherence to hand hygiene practice: A multidisciplinary approach. Emerg Infect Dis. 2001;7:234-240.
- Suchitra JB, Devi LN. Impact of education on knowledge, attitudes and practices among various categories of health care workers on nosocomial infections. Indian J Med Microbiol 2007; 25:181-187
- Voss A, Widmer AF.No time for handwashing!? Handwashing versus alcoholic rub: can we afford 100% compliance?Infect Control HospEpidemiol. 1997; 18:205-208.
- Bischoff WE, Reynolds TM, Sessler CN, Edmond MB, Wenzel RP. Hand washing compliance by health care workers: The impact of introducing an accessible, alcohol-based hand antiseptic. Arch Intern Med. 2000; 160:1017-1021.
- Pessoa-Silva CL, Dharan S, Hugonnet S, Touveneau S, Posfay-Barbe K, Pfister R, et al. Dynamics of Bacterial Hand Contamination During Routine Neonatal Care. Infection Control and Hospital Epidemiology. 2004;25:192-197
- Hugonnet S, Pittet D. Hand hygiene - Beliefs or science?. Clinical Microbiology and Infection. 2000; 6:348-354.
- Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV.Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 2004; 141:1-8.
- Sproat LJ, Inglis TJ. A multicentre survey of hand hygiene practice in intensive care units. J Hosp Infect. 1994; 26:137-148.
- Mazi W, Sanok AC, Al-Kandy S, Abdullah D. Implementation of the World Health Organization Hand Hygiene Improvement Strategy in Critical Care Units. Ant Res &Inf Control 2013;2:15
- Nair SS, Hanumanthappa R, Hiremath GS, Siraj MA, Raghinath P. Knowledge attitude and practices of hand hygiene among medical and nursing students at a tertiary healthcare center in Raichure India. ISRN Preventive Medicine. 2014.
- Wendt C. Hand hygiene--comparison of international recommendations. J Hosp Infect. 2001; 48 SA: S23-S28.
- Naikoba S, Hayward A.The effectiveness of interventions aimed at increasing handwashing in healthcare workers - A systematic review. J Hosp Infect. 2001; 47:173-180.
- Louise McLaws M, Pantle AC, Fitzpatrick KR, Hughes CF. Improvements in hand hygiene across New South Wales public hospitals: Clean hands save lives, Part III. Med J Aust 2009; 191: S18.
- Bowen A, Ma H, Ou J, Billhimer W, Long T, Mintz E. A cluster-randomized controlled trial evaluating the effect of a hand washing-Promotion program in Chinese Primary Schools. Am J Trop Med Hyg. 2007;76: 1166-1173
- Sandora TJ, Taveras EM, Shih M, Resnick EA, Lee GM, Ross-Degnan D, et al. A randomized, controlled trial of a multifaceted intervention including alcohol-based hand sanitizer and hand-hygiene education to reduce illness transmission in the home. Pediatrics. 2005; 116:587
- Pickering AJ, Boehm AB, Mwanjali M, Davis J. Efficacy of waterless hand hygiene compared with hand washing with soap: a field study in Dar es Salaam, Tanzania. Am J Trop Med Hyg. 2010; 82:270-278.
- Nantasit L, Maliwan H, Direk L, Yoel L, Lee AS, Stephan H et al. Comparative efficacy of interventions to promote hand hygiene in hospital: systematic review and network meta-analysis BMJ 2015; 351:h3728
- Ling ML, Hiw KB. Impact at a hospital wide hand hygiene promotion strategy in healthcare associated infections. Ant Res &Inf Control. 2012;1:13.
- Babeluk R, Jutz S, Mertlitz S, Matiasek J, Klaus C. Hand hygiene – Evaluation of three disinfectant hand sanitizers in a community setting. PLoS One. 2014; 9: e111969.
- Pan SC, Tien KL, Hung LC, Lin YJ, Sheng WH, Wang MJ et al. Compliance of healthcare workers with hand hygiene practices: independent advantages of overt and covert observers. PLoS One 2013;8:e53746.
- Carter D. The right balance between hand sanitizers and hand washing. Am J of Nursing. 2013; 113:13.
- Pittet D. Infection control and quality health care in the new millennium. American Journal of Infection Control. 2005;33:258-267.
- Goldmann D. System failure versus personal accountability — Thecase for clean hands. N Engl J Med 2006; 355:121-123.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.