An Overview of History, Pathogenesis and Treatment of Perforated Peptic Ulcer Disease with Evaluation of Prognostic Scoring in Adults
- *Corresponding Author:
- Dr. Vinod Prabhu
Department of Surgery, Bharati Medical College, Sangli, Maharashtra, India.
E-mail: cghert@yahoo.co.in
Citation: Prabhu V, Shivani A. An overview of history, pathogenesis and treatment of perforated peptic ulcer disease with evaluation of prognostic scoring in adults. Ann Med Health Sci Res 2014;4:22-9.
Abstract
Peptic ulcer disease including both gastric and duodenal ulcer form a substantial part of patients seeking surgical opinion world‑wide. The concept of acid in peptic ulcer disease, which was the basis of treatment of peptic ulcer was revolutionized by the discovery of H2‑receptor antagonists, that led to the principle of acid suppression therapy for duodenal ulcer which followed decades of preference for surgical interventions in the form of gastric resections, vagotomy etc., After the discovery of Helicobacter pylori organism as the causative factor a triple drug regime was identified to treat peptic disease which was further modified to sequential therapy to avoid antibiotic resistance. This recognition has not concluded the chapter on peptic ulcers. The management of ulcer disease and its complications remain a surgical challenge. All the materials for this review have been accessed from various internet search engines. The references have been narrowed down to 34 by excluding cross references, duplicated citations, pediatric studies, case reports, iatrogenic and malignant perforations and including microbiological, immunohistochemistry references and studies with more than a sample size of ten. Case control, cohort studies, prospective/retrospective, metaanalytical studies were preferred in that order. This article attempts to take an overview of all aspects of the management of peptic ulcer.
Keywords
Boey score, Helicobacter pylori, Pathogenesis, Peptic ulcer, Prognostic factors, Urea breath test
Introduction
Peptic ulcer disease includes both gastric and duodenal ulcers which posed a major threat to the world’s population over the past two centuries with a high morbidity and mortality. The evolution of knowledge regarding etiopathogenesis of peptic acid disease from acid‑driven disease to an infectious disease has opened up this topic for various studies to find the best possible options for management of this disease. The discovery of Helicobacter pylori has evinced great interest in the role played by this microbe. The eradication of this organism has been found to be of paramount importance to minimize the complications of peptic ulcers.
The management of peptic ulcer disease and its complications remain a challenge. In addition, non‑steroidal anti‑inflammatory drugs (NSAIDs), low‑dose aspirin, smoking, excessive alcohol use, emotional stress and psychosocial factors are increasingly important causes of ulcers and their complications even in H. pylori‑negative patients. Other rare causes of peptic ulcer disease in the absence of H. pylori, NSAIDs, and aspirin also exist.
Epidemiological studies reveal a very strong association between H. pylori infection and peptic ulcer disease. More than half the world’s population has a chronic H. pylori infection of the gastroduodenal mucosa, yet only 5‑10% develops ulcers. Factors that determine whether the infection will produce the disease depends on the pattern of histological changes, gastritis induced changes in homeostasis of gastric hormones and acid secretion, gastric metaplasia in the duodenum, interaction of H. pylori with the mucosal barrier, immunopathogenesis, ulcerogenic strains, and genetic factors.
Management of peptic acid disease varies from using H2 receptor antagonist, proton pump inhibitors (PPI) to triple chemotherapy and sequential regimen for H. pylori. Similarly treating perforation varies from a conservative non operative approach to a surgical approach.
Various prognosticating factors to predict mortality and morbidity have been used for scoring these patients of which Boey’s scoring system still forms a reliable system. Some scoring systems take only pre‑operative criteria into account whereas others include pre‑operative, intra operative and laboratory findings to score the patients.
Materials and Methods
Data source
The data used by the authors was sourced from Medline, Pubmed, Pubmed central (PMC), Google, Wiley online library, Springer link, Indian journal of surgery. The figures and tables have been compiled from internet search engines and modified in simple interpretational format.
Selection criteria
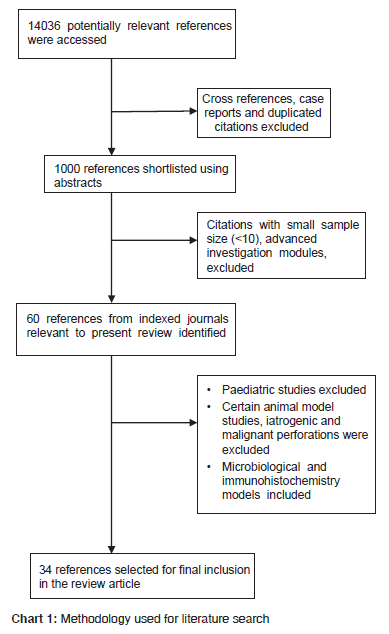
14036 references were initially accessed using “duodenal perforation”, “Helicobacter Pylori”, “drug therapy in peptic ulcer” as key search words, of which 1000 references were shortlisted after excluding case reports, cross references, complications of perforation and duplicated citations. The search was further narrowed to 60 references by identifying articles relevant to the present review. 34 references were finalized by ignoring paediatric studies, iatrogenic, malignant perforations and certain animal modules [Chart 1].
Preference was given to case control, cohort, prospective, retrospective studies and metaanalysis in that order.
References in the time frame of 1982-2012 were accessed.
Historical Aspects
The history probably starts with identification of duodenal perforation by To Cheng in 1984 when he found a duodenal perforation in a preserved body of 167 BC in China.[1]
In 1670 King Charles I’s daughter, Henriette‑Anne, died suddenly at the age of 26, a day after she complained of abdominal pain and tenderness. As poisoning was suspected an autopsy was performed that revealed peritonitis and a small hole in the anterior wall of the stomach.[2]
In 1843 Edward Crisp first reported 50 cases of peptic perforation and accurately described the clinical aspects of perforation, stating: “The symptoms are so typical, I hardly believe it possible that anyone can fail to make the correct diagnosis.” The basic idea for conservative treatment came from Crisp who noted that perforations of the stomach were filled by adhesions to the surrounding viscera which prevented leakage from the stomach into the peritoneal cavity.[2]
Johan Mikulicz‑Radecki (1850‑1905),[2] often referred to as the first surgeon who closed a perforated peptic ulcer by simple closure said, “Every doctor, faced with a perforated duodenal ulcer of the stomach or intestine, must consider opening the abdomen, sewing up the hole, and averting a possible inflammation by careful cleansing of the abdominal cavity.”
The Taylor method of conservative management presented in 1946, based on the theory that effective gastric decompression and continuous drainage will enhance self‑healing leading to treatment by nasogastric aspiration, antibiotics, intravenous fluids and nowadays H. pylori triple therapy.
Patients likely to respond to conservative management can be selected by performing a gastroduodenogram as described by Donovan.
Cellan‑Jones and Graham advocated use of omental patch for closing peptic perforations.[3]
Feliciano [4] in 1992 outlined five decisions facing the surgeon while treating peptic perforation viz,
1. Is the operation indicated?
2. Is an omental plication sufficient or is a definitive ulcer operation required?
3. Is the patient’s general condition stable enough to undergo a definitive ulcer operation?
4. Which definitive ulcer operation is indicated?
5. Should the availability of newer medical options influence the choice of operation? This was reinforced by Lagoo et al.[4] in 2002 by a sixth point of,
6. Should the procedure be performed laparoscopically or by laparotomy?
“Barry J. Marshall” and “Robin Warren” who identified H. pylori revolutionized the management of peptic disease [5,6] The Maastricht III Consensus Report [7] lay down guidelines for chemotherapy of H. pylori by using triple drug regime.
Several genes of H. pylori such as vacA and cagA have been identified as being related to virulence that may have clinical and epidemiological implications.[8,9]
Today, surgery for peptic ulcer disease is restricted to the treatment of complications such as perforation, bleeding etc., In peptic perforation, conservative treatment can be given in selected cases. If laparotomy is necessary, simple closure is sufficient in large majority of cases, and definitive ulcer surgery is no longer required in these patients.[10] Centre’s having facilities of laparoscopy and the expertise, undertake laparoscopic closure of perforation.[11]
Many scores are used to prognosticate mortality and morbidity in peptic perforation. All the scores, i.e. the Boey score, the mannheim peritonitis index (MPI) score, American society of Anesthesiologist score, Acute Physiology and Chronic Health Evaluation (APACHE II) score predict mortality and are used pre‑operatively in the scoring system.[12]
Pathogenesis of peptic disease
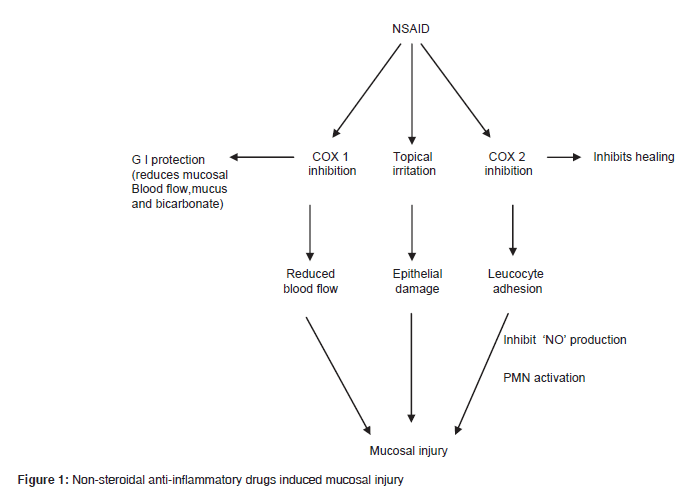
The pathogenesis of peptic ulcer disease may be considered as a combination scenario involving an imbalance between defensive factors (mucus‑bicarbonate layer, prostaglandins, cellular regeneration, mucosal blood flow) and aggravating factors (hydrochloric acid, pepsin, ethanol, bile salts, drugs). NSAIDs play an important role in the pathogenesis.[13,14]
The pathology can be divided in three broad categories, (1) H. pylori positive (2) H. pylori negative and non‑NSAID associated (3) NSAID associated.
There is a strong association between H. pylori infection and gastroduodenal ulcers. H. pylori causes an inflammatory response in gastric mucosa, with induction of epithelium derived cytokines, predominantly interleukin (IL) 8 and IL 1β.[15] Influx of neutrophils and macrophages into the gastric mucosa with release of lysosomal enzymes, leukotrienes (LT), and reactive oxygen species hampers mucosal defense and stimulates the immunopathogenetic process of ulcer formation. H. pylori has a very high urease activity, producing ammonia to protect the organism from the acidic gastric environment. Production of alkaline ammonia by bacteria on the surface epithelium and in the glands of the antrum inhibits D cells in the glands from sensing the true level of acidity leading to inappropriate release of somatostatin and hypergastrinemia. Urease catalyzes production of ammonia, when in large concentrations lead to formation of toxic complexes such as ammonium chloride which along with bacterial phospholipases A and C impair the phospholipid‑rich layer in the mucosa that maintains mucosal hydration and integrity of the gastric epithelial barrier.
Metaplasia is an essential prerequisite for H. pylori colonization of duodenal epithelium, because colonization is specific and exclusive to gastric epithelial cells. After colonization of islands of duodenal gastric metaplasia, the inflamed duodenal mucosa becomes more susceptible to peptic acid attack and ulceration.
Ulcers can exist in the absence of H. pylori infection and non‑NSAID group. Zollinger‑Ellison syndrome, truly idiopathic ulcers, Cushing’s ulcer, high‑dose upper abdominal radiotherapy, fall in this category.
NSAID induced ulcers [16] [Figure 1] form an important subset of ulcers that occur due to suppression of gastric prostaglandin synthesis. Prostaglandins are important for mucosal integrity. Cyclo‑oxygenase (COX 1 and COX 2) inhibition, more so of COX 2 is supposed to cause gastric ulcer. Neutrophil adherence is known to cause damage to mucosa by liberating oxygen free radicals, proteases release and reducing capillary blood flow. The role of nitric oxide (NO) and hydrogen sulphide (H2S), in maintaining integrity of gastric mucosa is well‑known. NO and H2S increase blood flow to mucosa, stimulate mucus secretion, and inhibit neutrophil adherence. NSAIDs, inhibit NO and H2S. We have in our rural setup identified NSAID as an important etiological factor due to indiscriminate use of these drugs for treating fever, joint pains, osteoarthritis of knee joints.
The carbon‑13‑urea [17] breath test is a costly, but reliable diagnostic indicator of H. pylori infection. It is advisable to look for the presence of H. pylori, as it can be eradicated easily. This test is carried out by giving oral 50 mg of 13C‑urea, in patients weighing less than 50 kg or 75 mg of 13C‑urea if they weighed more than 50 kg with 50 mg of a glucose polymer solution in 7.5 ml of water orally. Breath samples are collected at baseline and at 15, 30, 45, and 60 min. Detection of isotope‑labeled carbon di oxide in exhaled breath indicates the presence of H. pylori. The test is 100% sensitive and 97.6% specific at 30 min with a cutoff value of 3.5 delta 13CO2/ml. It takes 30 min for sampling. Neither fasting nor a test meal is required. However, the preferred method to diagnose H. pylori is by taking mucosal biopsies.
Immunopathologyof peptic ulcer
The response to H. pylori infection is mediated by release of bacterial lipopolysaccharide which perpetrates an acute followed by chronic immune response. Initially there is a polymorphonuclear infiltration which along with bacterial products stimulate the production of IL 8 whose production is stimulated by tumor necrosis factor alpha (TNF‑α) and IL‑1 released by macrophages in response to bacterial lipopolysaccharide. The acute and chronic response is facilitated by T‑helper cells. Th1 cells that promote inflammation and by activating Cluster of differentiation 8+ T cells lead to autoantibody formation and cell‑mediated epithelial damage. Continuous secretion of IL 8 due to chronicity of infection leads to mucosal damage and increased free radical formation. LT are mediators for mucosal damage particularly in alcohol induced ulcers where LT B4 is known to be a potent vasoconstrictor that induces mucosal ischemia. Cytokines [18] play an important role in regulation of mucosal immune system. Inflammation of gastroduodenal mucosa leads to release of IL 1β, IL 2, IL 6, IL 8 and TNF that damages mucosal tissue. The levels of IL 1β are elevated in H. pylori infection which causes inhibition of gastric acid and pepsinogen secretion.
Scoring systems for peptic perforation
As peptic perforation is life threatening, various scoring systems [19,20] have evolved to prognosticate mortality and morbidity. Some systems take pre‑operative status into account whereas others take the laboratory parameters and intra‑operative findings into account for scoring. We feel the Boey’s scoring system still stands the test of time and assess the condition of the patient fairly accurately. The MPI, APACHE II, Hacetteppe systems contain detailed parameters to be investigated to arrive at a score.
In our opinion the scoring system should be simple and should optimally predict the outcome on admission itself taking only clinical parameters into account so that a opinion can be given to the patient’s relatives about the prognosis which would allay any doubts.
Concurrent medical illness, pre‑operative shock, and longstanding perforations (more than 24 h) are taken into account in Boeys score [Table 1].
| Risk factors | No. of risk factors |
|---|---|
| None of below | 0 |
| Pre-operative BP<100 mmHg | 1 |
| Delayed presentation>24 h | 2 |
| Major medical illness present | 3 |
BP: Blood pressure
Table 1: Boey’s score.
Temperature, oxygen saturation, arterial pressure, heart rate, respiratory rate etc., are to be recorded in APACHE II score with interpretation [Table 2].
| High abnormal range | Low abnormal range | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Score→ | +4 | +3 | +2 | +1 | 0 | +1 | +2 | +3 | +4 |
| Temperature | >41 | 39-40.9 | 38.5-38.9 | 36-38.4 | 34-35.9 | 32-33.9 | 30-31.9 | <29.9 | |
| Meanarterial pressure mmHg | >160 | 130-159 | 110-129 | 70-109 | 50-69 | 40-54 | <39 | ||
| Heart rate | >180 | 140-179 | 110-139 | 70-109 | 50-69 | 40-54 | <39 | ||
| Resp rate | >50 | 35-49 | 25-34 | 12-24 | 10-11 | 6-9 | <5 | ||
| Oxygenation | >500 | 350-499 | 200-349 | <200 | |||||
| ArterialpH | >7.7 | 7.6-7.69 | 7.5-7.59 | 7.33-7.49 | 7.25-7.32 | 7.15-7.24 | <7.15 | ||
| S Sodium | >180 | 160-179 | 155-159 | 150-154 | 130-149 | 120-129 | 128-119 | <119 | |
| S Potassium | >7 | 6-6.9 | 5.5-5.9 | 3.5-5.4 | 2.9-3.4 | 2.5-2.9 | <2.5 | ||
| S Creatinine | >3.5 | 2-3.4 | 1.5-1.9 | 0.6-1.4 | <0.6 | ||||
| Hematocrit | >60 | 50-59.9 | 46-49.9 | 30-45.9 | 20-29.9 | <20 | |||
| WBC total/mm3 IN 1000 | >40 | 50-39.9 | 15-19.9 | 3-14.9 | 1-2.9 | <1 | |||
| Glasgow coma scale (score-15) | |||||||||
| Total score | |||||||||
| Interpretation | |||||||||
| Score | Death rate (%) | ||||||||
| 0-4 | 4 | ||||||||
| 5-9 | 8 | ||||||||
| 10-14 | 15 | ||||||||
| 15-19 | 25 | ||||||||
| 20-24 | 40 | ||||||||
| 25-29 | 55 | ||||||||
| 30-34 | 75 | ||||||||
| >34 | 85 | ||||||||
Table 2: Acute physiology and chronic health evaluation II score.
MPI system takes into account the type of peritoneal exudates [Table 3] and the Hacetteppe score takes medical illness, acute renal failure, white cell count of more than 20 × 109/l, and male sex into consideration [Table 4].
| Criteria | Score |
|---|---|
| Age>50 years | 5 |
| Female sex | 5 |
| Organ failure | 7 |
| Malignancy | 4 |
| Pre-operative duration of peritonitis>24 h | 4 |
| Origin of sepsis not colonic | 4 |
| Diffuse generalized peritonitis | 6 |
| Exudate | |
| Clear | 0 |
| Cloudy, purulent | 6 |
| Fecal | 12 |
Kidney failure=creatinine level>177 umol/L or urea level>167 mmol/L or oliguria<20 ml/h; pulmonary insufficiency=PO2<50 mmHg or PCO2>50 mmHg; Intestinal obstruction/paralysis>24 h
Table 3: Mannheim peritonitis index.
| Critera | Score |
|---|---|
| Coexisting medical illness | 1 |
| Acute renal failure | 1 |
| White cell count of more than 20�109 | 1 |
| Male sex | 1 |
Table 4: Hacetteppe score.
In a large series by Irvin, scores based on the presence of shock, delayed presentation or concurrent medical illness could have predicted majority of post‑operative deaths in elderly subjects, and it was suggested that risk stratification and greater caution in the use of definitive operations for perforated ulcer may result in a reduction in the high mortality rate in elderly subjects.
Similarly many authors have observed that likelihood of death could be predicted by the Boey score whereas the APACHE II score was better in predicting morbidity. Considering the large number of parameters that need to be evaluated in APACHE score that may not be possible in all set ups particularly so in our rural area Boey score still stands the test of time.
The summary of all scoring systems [21] lead us to believe that delay in treatment, concurrent medical illness and presence of shock form a vicious triad for mortality. As these criteria are met by Boeys, score it seems to be fairly indicative of morbidity and mortality.[22,23] Hence the scoring system should be regularly utilized for prognostication.
Medical management of peptic ulcer
The medical management of peptic disease was revolutionized by the advent of H2 receptor antagonists like ranitidine with subsequent discovery of PPI i.e omeprazole and its newer generations. It was then that H. pylori was identified and various eradication regimes evolved. H. pylori eradication regimen included the three drug regime [Table 5]. In order to avoid resistance to antibiotics a sequential regime is being used in many countries [Table 5a]. Selective COX 2 inhibitors were introduced to minimize NSAID induced ulcers. PPI forms the mainstay in NSAID induced ulcers. Misoprostol is better than H2 receptor antagonist in preventing gastric ulcer. There are research projects that are on to evaluate the preference for using safer analgesics based on the premise that addition of NO, H2S releasing moiety to analgesics in the form of [4‑(nitrooxy)‑Butyl‑(2S)‑2‑(6‑methoxy‑2‑naphthyl) ‑propanoate] 3582, 2‑(acetyloxy) benzoic acid3‑[(nitrooxy) methyl] phenyl ester]‑4016 molecule eliminates peptic ulcer risk substantially. These are partly in animal and human trials.[24‑26] In our institute we prescribe triple therapy to all patients with peptic ulcer and perforation as facilities for breath test and H. pylori histology and culture are not available.
| First-line options (7-14 days) | |
|---|---|
| In populations with less than 15-20% clarithromycin resistance and greater than 40% metronidazole resistance |
PPI standard dose, clarithromycin 2�500 mg, and amoxicillin 2�1000 mg, all given twice a day |
| Less than 15-20% clarithromycin resistance and less than 40% metronidazole resistance |
PPI standard dose, clarithromycin 500 mg, and metronidazole 400 mg or tinidazole 500 mg, all given twice a day |
| In areas with high | Bismuth-containing quadruple |
| clarithromycin and | therapy |
| metronidazole resistance | |
| Second-line | 1) Bismuth-containing |
| option (10-14 days) | quadruple therapy 2) PPI plus |
| metronidazole and amoxicillin, | |
| if clarithromycin was used | |
| in first-line treatment (in | |
| Latin America and China, | |
| furazolidone 2-4�100 mg | |
| is often preferred over | |
| metronidazole) | |
| Rescue therapies (10-14 days) | PPI twice a day plus amoxicillin |
| 2�1000 mg with either | |
| levofloxacin 2�250 (500) mg, or | |
| with rifabutin 2�150 mg | |
PPI: Proton pump inhibitor
Table 5: Helicobacter pylori eradication regimens.
| Day 1 to day 5 | Pantoprazole 40 mg twice daily+Amoxycillin 1gm twice daily |
| Day 6 to day 10 | Pantoprazole 40 mg twice daily+Clarithromycin 500 mg twice daily+Tinidazole 500 mg twice daily |
Omeprazole plus amoxicillin for 5 days, followed by omeprazole plus clarithromycin plus tinidazole for another 5 days.
Table 5a: Sequential therapy.
Management of perforated peptic ulcers
Perforation management of gastroduodenal ulcers has had many opinions.
Duodenal ulcers are the commonest ulcers to perforate as compared to gastric ulcers. Surgery forms the mainstay of treating perforation. It can be done by laparoscopy or open laparotomy.
Conservative treatment known as the Taylor method [27] consists of Ryles tube aspiration, antibiotics, intravenous fluids and nowadays H. pylori triple therapy. Patients likely to respond to conservative treatment can be identified by performing a gastroduodenogram as described by Donovan et al.[28] and demonstrate no leak. A randomized trial suggested that in patients with perforated peptic ulcer, an initial period of conservative treatment with careful observation may be safely allowed except in patients over 70 years old, because such an observation period can avoid the need for emergency surgery in more than 70 percent of patients.[29] However, this contention will not hold good in cases with long perforation‑operation interval. In conclusion non operative choice should be made in surgically unfit patients only.
The open repair entails the closure of perforation by Grahams patch or Cellan‑Jones technique. Here we would like to clarify that the former used a free omental graft and the latter pedicled omental graft. In our opinion a pedicled omentopexy is preferable as the patch remains viable for a longer period. In larger perforations which is defined as a perforation of more than 3 cm in size jejunal serosal flaps or antrectomy are done. A good peritoneal lavage is also important. A drain will not reduce the incidence of intra‑abdominal fluid collections or abscesses.[30] However, we would recommend use of drains as it reduces toxic peritoneal collections that adds to early convalescence. Rat models have proved that omental grafts helped ulcer healing and prevented ulcer recurrence due to the presence of fibroblast growth factor and transforming growth factor at the graft site indicating a significant role in healing due to greater anti‑inflammatory, increased angiogenic activity and increase in collagen synthesis activity.[31]
The indications for elective surgery during emergency laparotomy are still ill‑defined. However, highly selective vagotomy has been recommended in places where the cases present early with no comorbid factors. The addition of a definitive surgical procedure such as Billroth I/II; vagotomy during the emergency surgery is not necessary as it increases operating time particularly so in rural scenario where presentation to institute is delayed invariably due to poor socioeconomic conditions. In gastric perforations [32] the options available are primary closure with omental patch or adding a definitive procedure along with closure. Suffice it to state that simple closure is associated with low mortality and morbidity rate. Resections should be restricted to large ulcers and in early presentations.[33]
Laparoscopic repair has its own pros and cons. A laparoscopic procedure is a minimally invasive tool. Benefits of laparoscopic repair are reduced post‑operative pain, lesser use of analgesics, reduced hospital stay. Furthermore, a reduction in wound infections, burst abdomen and incisional hernia due to small scars is known. Drawbacks are a long operating time, higher incidence of re‑operations due to leakage at the repair site and a higher incidence of intra‑abdominal collection secondary to inadequate lavage and not the least requires an expert.[11]
A new method, called “stamp” method that uses a biodegradable patch made of lactide‑glycolide‑caprolacton to close the perforation using a glue Glubran 2 made of n‑butyl 2 cyanoacrylate 2‑octil cyanoacrilate, which has been approved for intracorporeal usage is in a trial stage in rats which has encouraging results.[34]
Conclusion
It has been the endeavor of this article to review the literature for evaluating the peptic acid disease spectrum particularly from a rural medical college perspective and to infer as to what is in the best interest from a rural medical college point of view.
We infer that in an area where general practitioners are the first contact for the patients a substantial reduction or judicious use of NSAID’s will help in reducing gastro duodenal ulcers. Newer NO, H2S releasing drugs if introduced would go a long way to reduce incidences of peptic disease and its complications.
In proved cases of gastro duodenal ulcers on endoscopy use of triple drug therapy for elimination of H. pylori is mandatory.
It would be advisable not to add a definitive procedure in emergency surgery scenario, if the perforation‑operation interval is more, elderly patients and patients having severe comorbid factors.
Boey score should be used to convey the prognosis of the patient.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Lau WY, Leow CK. History of perforated duodenal and gastric ulcers. World J Surg 1997;21:890-6.
- Bertleff MJ, Lange JF. Perforated peptic ulcer disease: A review of history and treatment. Dig Surg2010;27:161-9.
- Slade H, Howell HS. When repair is enough for perforated duodenal ulcer. Contemp Surg 2008;64:523. Available from: http://www.contemporarysurgery.com.
- Lagoo S, McMahon RL, Kakihara M, Pappas TN, Eubanks S. The sixth decision regarding perforated duodenal ulcer. JSLS 2002;6:359-68.
- Watts G. Nobel prize is awarded to doctors who discovered H. pylori. BMJ 2005;331:795.
- Ahmed N. 23 years of the discovery of Helicobacter pylori: Is the debate over? Ann Clin Microbiol Antimicrob 2005;4:17.
- Malfertheiner P, Megraud F, O?Morain CA, Atherton J, Axon AT, Bazzoli F, et al. Management of Helicobacter pylori infection?The Maastricht IV/Florence Consensus Report. Gut 2012;61:646-64.
- van Doorn LJ . Detection of Helicobacter pylori virulence-associated genes. Expert Rev Mol Diagn 2001;1:290-8.
- van Doorn LJ, Figueiredo C, Sanna R, Plaisier A, Schneeberger P, de Boer W, et al. Clinical relevance of the cagA, vacA, and iceA status of Helicobacter pylori. Gastroenterology 1998;115:58-66.
- Zittel TT, Jehle EC, Becker HD. Surgical management of peptic ulcer disease today?Indication, technique and outcome. Langenbecks Arch Surg 2000;385:84-96.
- Bhogal RH, Athwal R, Durkin D, Deakin M, Cheruvu CN. Comparison between open and laparoscopic repair of perforated peptic ulcer disease. World J Surg 2008;32:2371-4.
- Lee FY, Leung KL, Lai BS, Ng SS, Dexter S, Lau WY. Predicting mortality and morbidity of patients operated on for perforated peptic ulcers. Arch Surg 2001;136:90-4.
- Ballinger A, Smith G. COX-2 inhibitors vs. NSAIDs in gastrointestinal damage and prevention. Expert Opin Pharmacother 2001;2:31-40.
- Huang JQ, Sridhar S, Hunt RH. Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: A meta-analysis. Lancet 2002;359:14-22.
- Noach LA, Bosma NB, Jansen J, Hoek FJ, van Deventer SJ, Tytgat GN. Mucosal tumor necrosis factor-alpha, interleukin-1 beta, and interleukin-8 production in patients with Helicobacter pylori infection. Scand J Gastroenterol 1994;29:425-9.
- Wallace JL, Vong L. NSAID-induced gastrointestinal damage and the design of GI-sparing NSAIDs. Curr Opin Investig Drugs 2008;9:1151-6.
- Rowland M, Lambert I, Gormally S, Daly LE, Thomas JE, Hetherington C, et al. Carbon 13-labeled urea breath test for the diagnosis of Helicobacter pylori infection in children. J Pediatr 1997;131:815-20.
- Kaur A, Robin S, Sharma R. Peptic ulcer: A review on etiology and pathogenesis. Int Res J Pharm 2012;3:2230-8407.
- M�kel� JT, Kiviniemi H, Ohtonen P, Laitinen SO. Factors that predict morbidity and mortality in patients with perforated peptic ulcers. Eur J Surg 2002;168:446-51.
- Boey J, Choi SK, Poon A, Alagaratnam TT. Risk stratification in perforated duodenal ulcers. A prospective validation of predictive factors. Ann Surg 1987;205:22-6.
- Svanes C, Salvesen H, Espehaug B, S�reide O, Svanes K. A multifactorial analysis of factors related to lethality after treatment of perforated gastroduodenal ulcer. 1935-1985. Ann Surg 1989;209:418-23.
- Lohsiriwat V, Prapasrivorakul S, Lohsiriwat D. Perforated peptic ulcer: Clinical presentation, surgical outcomes, and the accuracy of the Boey scoring system in predicting postoperative morbidity and mortality. World J Surg 2009;33:80-5.
- Boey J, Wong J, Ong GB. A prospective study of operative risk factors in perforated duodenal ulcers. Ann Surg 1982;195:265-9.
- Wallace JL. Prostaglandins, NSAIDs, and gastric mucosal protection: Why doesn?t the stomach digest itself? PhysiolRev2008;88:1547-65.
- Fiorucci S, Santucci L, Gresele P, Faccino RM, Del Soldato P, Morelli A. Gastrointestinal safety of NO-aspirin (NCX-4016) in healthy human volunteers: A proof of concept endoscopic study. Gastroenterology 2003;124:600-7.
- Hawkey CJ, Jones JI, Atherton CT, Skelly MM, Bebb JR, Fagerholm U, et al. Gastrointestinal safety of AZD3582, a cyclooxygenase inhibiting nitric oxide donator: Proof of concept study in humans. Gut 2003;52:1537-42.
- Dascalescu C, Andriescu L, Bulat C, Danila R, Dodu L, Acornicesei M, et al. Taylor?s method: A therapeutic alternative for perforated gastroduodenal ulcer. Hepatogastroenterology 2006;53:543-6.
- Donovan AJ, Berne TV, Donovan JA. Perforated duodenal ulcer: An alternative therapeutic plan. Arch Surg 1998;133:1166-71.
- Crofts TJ, Park KG, Steele RJ, Chung SS, Li AK. A randomized trial of nonoperative treatment for perforated peptic ulcer. N Engl J Med 1989;320:970-3.
- Schein M. To drain or not to drain? The role of drainage in the contaminated and infected abdomen: An international and personal perspective. World J Surg 2008;32:312-21.
- Matoba Y, Katayama H, Ohami H. Evaluation of omental implantation for perforated gastric ulcer therapy: Findings in a rat model. J Gastroenterol 1996;31:777-84.
- Madiba TE, Nair R, Mulaudzi TV, Thomson SR. Perforated gastric ulcer ? Reappraisal of surgical options. S Afr J Surg 2005;43:58-60.
- Turner WW Jr, Thompson WM Jr, Thal ER. Perforated gastric ulcers. A plea for management by simple closures. Arch Surg 1988;123:960-4.
- Bertleff MJ, Stegmann T, Liem RS, Kors G, Robinson PH, Nicolai JP, et al. Comparison of closure of gastric perforation ulcers with biodegradable lactide-glycolide-caprolactone or omental patches. JSLS 2009;13:550-4.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.