Anthropometric Correlates and Prediction of Body Fat Measured by Bioelectric Impedance Analysis among Women
2 Department of Paediatrics, Ekiti State University, Ekiti State University Teaching Hospital, Ado-Ekiti Ekiti State, Nigeria
Citation: Raimi TH, et al. Anthropometric Correlates and Prediction of Body Fat Measured by Bioelectric Impedance Analysis among Women. Ann Med Health Sci Res. 2017; 7: 32-35
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
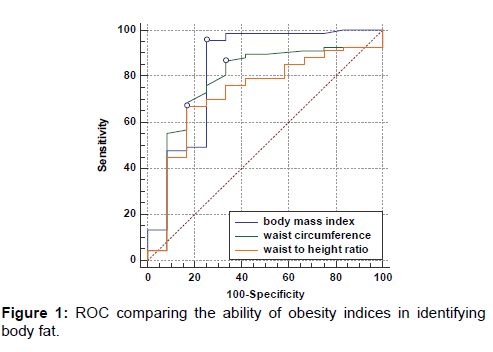
Context: Obesity may be defined based on percentage body fat. Because of the difficulty in measuring body fat in routine clinical practice, a number of surrogates such as body mass index (BMI), waist circumference (WC), waist-to-hip ratio (WHR), and waist-to-height ratio (WHtR) have been proposed. Aims: To determine the correlation between obesity indices and body fat, and the predictive ability of these indices to identify percentage body fat among women. Settings and Design: Cross-sectional. Methods and Material: Seventy nine women who participated in health screening were included in the study. BMI, WC, and WHtR of the participants were determined by standard protocols. Percentage body fat and visceral fat were measured by bioelectrical impedance analysis. Statistical analysis: Pearson correlation between percentage body fat and the obesity indices was determined. The area under curve (AUC) on the ROC was used to determine the best anthropometric index which identifies individuals with obesity. Results: The participant’s mean age was 42.4±9.1 years. There was a significant correlation between body fat and the anthropometric indices (p<0.001), but the correlation was best with BMI. The AUC on the ROC for BMI, WC, and WHtR, respectively were 0.831 (95% CI 0.669-0.993, p<0.001), 0.780 (95% CI 0.627-0.933, p=0.002), and 0.725 (95% CI 0.571-0.880, p=0.013). Conclusions: There is positive correlation between percentage body fat and anthropometric indices. Body mass index is as good as waist circumference, but better than waist to height ratio in predicting body fat. BMI should not be abandoned in the clinical evaluation of people with obesity.
Keywords
Adipose tissue; Anthropometry; Body mass index; Waist circumference; Waistheight ratio
Introduction
Obesity may be defined based on percentage body fat. [1]. The prevalence of obesity is rising globally with its attendant complications. [2]. Studies in Nigeria have shown that the burden of obesity is greater among women. [3,4]. We earlier reported that in south-west Nigeria, 11 women had obesity for every man who was obese. [5].
Because of the difficulty in measuring body fat in routine clinical practice, a number of surrogates have been proposed. These include body mass index (BMI), waist circumference (WC), waist-to-hip ratio (WHR), and waist-to-height ratio (WHtR). These surrogates have been shown to correlate with body fat among women by authors from other countries. [6,7]. A study among men revealed similar association. [8].
Some researchers [9,10]. have suggested that measures of central obesity are superior to BMI, and most criteria for the diagnosis of metabolic syndrome did not include BMI. [11,12]. Reports from Nigeria are scanty. Furthermore, the predictive ability of these indices with respect to body fat in our environment is unknown.
This study aimed at determining the correlation between obesity indices and body fat, and the predictive ability of these indices to identify obesity defined as percentage total body fat among women.
Subjects and Methods
The data of women who participated in health screening for noncommunicable diseases that was conducted at some secondary schools during the 2013/2014 World Diabetes Day celebration was used for the study. The school authority approved the screening exercise. Approval was also obtained from the Ethic and Research committee of our institution. The participants were screened for obesity, hypertension and diabetes mellitus.
Clinical measurements
The body mass index (BMI), waist circumference (WC), waist-to-height ratio (WHtR), and blood pressure (BP) of the participants were determined by standard protocols. Summarily, the height was determined to the nearest 0.1m with a stadiometer while the participants were barefooted. The weight was measured with a digital weighing scale to the nearest 0.1kg. The participants were barefooted and wore light clothing before the weight was taken. The height and weight were taken without headgear. The BMI was calculated with weight/height2. The waist circumference was measured along the umbilicus during expiration in centimetres. The WHtR was calculated as WC/Ht.
Percentage total body fat (%BF) and visceral fat (%VF) were measured by bioelectrical impedance analysis (BIA) using a body composition monitor (OMRON 511, OMRON healthcare Co., Ltd. Japan) in the fasting state. The monitor utilizes 8-sensor-measurement technology using both hands and feet for an accurate entire body measurement and classification of body fat percentage, visceral fat, skeletal muscle fat, and body mass index. The age, gender and height of the participants were entered into the device and confirmed. The participants then stood with the knees and back straight and looked straight ahead. The arms were horizontally raised and extended at a 90° angle to the body and the elbows were extended straight. The participants stood with weight evenly distributed on the measurement platform. The palms were pressed firmly on the grip electrodes, the middle fingers in the dent at the back of the grip electrodes, the inner grip electrodes held firmly with the thumb and index finger, and the outer grip electrodes held with the ring and small fingers. The measurement results on the display area of the device were then recorded. Obesity was defined as body fat>33%. [13].
Blood pressure was determined electronically with Omron or manually with mercury sphygmomanometer. Blood glucose was determined with a glucose meter (Accucheck active, Roche diagnostics)
Statistical analysis
Data were analysed with the statistical package for social sciences (SPSS) version 20.0 (Chicago, Illinois, USA). Continuous and categorical data were expressed as means and percentages respectively. Pearson correlation between percentage body fat and the obesity indices was determined. MedCalc Statistical Software version 14.8.1 (MedCalc Software, Ostend, Belgium, 2014) was used to generate Receiver Operative Characteristics (ROC) Curve, in order to determine and compare the ability of the anthropometric indices to identify obesity. The area under curve (AUC) on the ROC was used to determine the best anthropometric index which identifies individuals with obesity, defined as %body fat. The level of significance was set at p<0.05.
Results
A total of 99 women were screened, but 20 women who had insufficient information were not included in the data analysis. Data on seventy nine (79) women was finally analysed. Sixty seven (84.8%) participants were obese. Their clinical characteristics are shown in Table 1.
| Clinical characteristics | Mean (SD) |
|---|---|
| Age (years) | 42(9.1) |
| Weight (kg) | 73.8 (16.3) |
| BMI (kg/m2) | 30.49 (6.12) |
| WC (cm) | 88.2 (13.8) |
| WHtR | 0.57(0.08) |
| % body fat | 43.59(10.73) |
| % visceral fat (n=69) | 9.88 (5.55) |
| FBS (n=59) | 94.09(11.22) |
| SBP (n=77) | 129.16(29.51) |
| DBP (n=77) | 73.83(13.12) |
BMI: Body Mass Index; WC: Waist Circumference; WHtR: Waist To Height Ratio; FBS: Fasting Blood Glucose; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure
Table 1: Clinical characteristics of the study participants.
Table 2 shows that there was a significant correlation between body fat and the anthropometric indices (p<0.001). The correlation was best with body mass index.
| Obesity indices | Weight | BMI | WC | WHtR | %BF | %VF |
|---|---|---|---|---|---|---|
| Weight | 1 | 0.884** | 0.761** | 0.667** | 0.561** | 0.444** |
| BMI | 0.884** | 1 | 0.718** | 0.729** | 0.601** | 0.481** |
| WC | 0.761** | 0.718** | 1 | 0.964** | 0.411** | 0.410** |
| WHtR | 0.667** | 0.729** | 0.964** | 1 | 0.403** | 0.432** |
| % BF | 0.561** | 0.601** | 0.411** | 0.403** | 1 | 0.295* |
| % VF | 0.444** | 0.481** | 0.410** | 0.432** | 0.295* | 1 |
BMI: Body Mass Index; WC: Waist Circumference; WHtR, Waist To Height Ratio; SBP, Systolic Blood Pressure; DBP, Diastolic Blood Pressure **Correlation is significant at the 0.01 Level (2-Tailed); *Correlation is significant at the 0.05 level (2-tailed).
Table 2 : Correlation matrix between anthropometric indices and body fat.
Figure 1 shows the predictive ability of the anthropometric indices. BMI has the greatest Area under Curve (AUC). The AUC on the ROC for BMI, WC, and WHtR, respectively were 0.831 (95% CI 0.669-0.993, p<0.001), 0.780 (95% CI 0.627- 0.933, p=0.002), and 0.725 (95% CI 0.571-0.880, p=0.013).
Table 3 compares the AUC for detecting body fat. It showed that BMI was better than WHtR at detecting the presence of body fat (difference in areas = 0.106 p=0.0245). The AUC of BMI versus WC and WC versus WHtR on the ROC for identifying body fat were not significantly different.
| BMI ~ WC | |
| Difference between areas | 0.0516 |
| 95% CI | -0.0278 to 0.131 |
| z statistic | 1.274 |
| Significance level | p=0.2028 |
| BMI ~ WHtR | |
| Difference between areas | 0.106 |
| 95% CI | 0.0137 to 0.199 |
| z statistic | 2.249 |
| Significance level | p=0.0245 |
| WC ~ WHtR | |
| Difference between areas | 0.0547 |
| 95% CI | -0.00154 to 0.111 |
| z statistic | 1.906 |
| Significance level | p=0.0566 |
Table 3 : Pairwise comparison of AUC on the ROC of obesity indices in identifying body fat.ÂÂ
Discussion
Correlation between body fat and anthropometric indices
This study examines the correlation between percentage body fat and anthropometric indices as well as percentage visceral fat and anthropometric indices among women. Since obesity describes excess fat in the body, estimate of the body fat content should be used to define it. However, direct measurement of body fat is not routinely done in clinical and epidemiological surveys because this is expensive. Furthermore, the facilities such as CT scan, MRI and Dual energy X-ray absorptiometry are not readily available especially in our environment. Moreover, some of these diagnostic methods are associated with radiation exposure. Therefore, surrogates such as BMI, WC, WHtR, and WHR are used to determine adiposity. Bioelectrical impedance analysis (BIA) offers a cheaper, hazard-free and accessible way of estimating body fat, and it has been shown by several authors to compare well or correlate with the gold standards. [14-17].
The three indices of obesity studied were positively correlated with body and visceral fat. The correlation between % BF was best with BMI when compared with WC and WHtR. Similarly, although the correlation between the anthropometric indices and %VF was weak, it was best with BMI compared to WC and WHtR. Previous authors also found positive correlation between anthropometric indices and body fat as well as visceral fat. [7,18,19]. Percentage body fat describes the total body fat, and since body mass index is a measure of total adiposity, it is not surprising that the two entities correlated with each other. Waist circumference on the other hand is a measure of abdominal adiposity and may therefore be less correlated to percentage body fat than the BMI. Similar to our findings, the two studies [18,19]. above also found that BMI correlated with fat mass better than WC, whereas another study [20]. also revealed a better correlation between BMI and %BF compared to WC.
Abdominal fat is composed of subcutaneous fat and visceral fat, and in women subcutaneous fat is greater or more than visceral fat. [21]. WC is expected to correlate with both %body fat (which includes subcutaneous adipose tissue) and %VF.
In our study, whereas the correlation between BMI and %BF was stronger than the correlation between BMI and %VF, WC had similar correlation with both %BF and %VF. Further, we found that BMI had a stronger correlation with %VF than WC similar to the report by other workers, [7,22]. but in contrast to the findings of Kuk et al. [23]. and Jia et al. [24]. Similar to our findings, the report by Weerarathna et al. [7]. revealed that BMI had stronger correlation with both total and regional fat than all the other anthropometric indices. Interestingly, their study was also conducted only among women.
Since WC is a measure of abdominal obesity, the reason for the stronger correlation between BMI versus VF compared to WC versus VF in is not clear. Even though there are gender differences in the association between WC and body fat, Barreira et al. [19]. Kuk, and Janiszewski et al. [23]. Jia et al. [24]. and Kuk et al. [25]. found that WC correlated better with VF than BMI in both men and women. Previous studies on the relationship between anthropometric indices and body fat have yielded conflicting or inconsistent results. Both BMI and WC were previously found to correlate with fat mass better than VF. [18]. But, while some authors [23] found that the relationship between BMI and measures of body fat is dependent on WC, others [26]. reported that both BMI and WC were associated with VF, subcutaneous abdominal and total body fat independent of each other. Our study also revealed that when compared with WC, WHtR correlated better with %VF. Not many studies reported the correlation of WHtR and body fat. One study found that WSR (another name for WHtR) correlated with %body fat than WC among women. [22]. A study conducted among men also revealed that WHtR had stronger correlation with adipose tissue than other anthropometric indices [8]., whereas among women, another study [7]. found that both BMI and WC correlated with total and visceral fat than WHtR. As mentioned earlier, gender differences exist in the association of anthropometry and body fat. WHtR is WC corrected for height, and as such a measure of abdominal adiposity. It has been shown to be a good predictor of cardiovascular disease in both original research and systematic review. [26-29].
Prediction of obesity defined as body fat by anthropometric indices
The ability of anthropometric indices to predict body fat is very important in clinical settings, since they are surrogate measures of excess body fat. This will enable clinicians to confidently diagnose obesity.
A study revealed that WC predicted visceral fat better than other anthropometric indices when analysed by ROC. [24]. In contrast to the above, some workers concluded that in view of the comparable association of BMI and WC with total and visceral adipose tissue, the two indices of obesity give similar information about body fat [29,30]. Our study showed that BMI did not only correlate best with body fat, it also had the highest AUC on the ROC. The difference in the AUC between BMI and WHtR was significant, but when compared with WC, the difference was not significant.
Taken together, the above suggest that BMI is a good index of adiposity among the people studied. Therefore, BMI should not be abandoned in the clinical evaluation of people with obesity. This is important because most criteria for the diagnosis of metabolic syndrome did not include BMI. [11,12].
Limitation
This study is limited by the small sample size. A larger study is necessary to confirm the findings in this study. Determination of body fat with DEXA, computed tomography, and magnetic resonance imaging give more accurate result than the BIA used in this study. The body temperature and menstrual history of the participants were not taken. Ambient temperature and menstruation are known to influence BIA.
Conclusion
There is correlation between percentage body / visceral fat and anthropometric indices. Body mass index is as good as waist circumference, but better than waist to height ratio in predicting body fat. BMI should not be abandoned in the clinical evaluation of people with obesity.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- http://www.who.int/topics/obesity/en/. Accessed 2017
- World Health Organization. Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000; 894:i-xii, 1-253.
- Oladapo OO, Falase AO, Salako L, Sodiq O, Soyinka K, Adedapo K. Prevalence of cardiometabolic risk factore among a rural Yoruba south-western Nigerian population: A population-based survey. Cardiovasc J Afr. 2010; 21:26-31.
- Okafor CI, Gezawa ID, Sabir AA, Raimi TH, Enang O. Obesity, overweight, and underweight among urban Nigerians. Nig J Clin Pract. 2014; 17:743-749.
- Raimi TH, Odusan O, Fasanmade OA. High prevalence of central obesity in rural South-Western Nigeria: Need for targeted prevention. J Diabetes Endocrinol. 2015; 6:12-18.
- Gomes DM, Rech C, Gomes BM, Dos Santos DL. Correlation between anthropometric indices and body fat distribution in elderly women. Braz J Kin Hum Perf. 2006; 8:16-22.
- Weerarathna TP, Lekamwasam S, Rodrigo M. Prediction of total and visceral fat contents using anthropometric measures of adiposity in women. Ceylon Med J. 2008; 53:128-132.
- Chandrasekharan NK, Vipin B, Neeraj M. The normal range of body mass index with high body fat percentage among male residents of Lucknow city in north India. Indian J Med Res. 2012; 135: 72–77.
- Bener A, Yousafzai MT, Darwish S, Al-Hamaq AO, Nasralla EA, Abdul-Ghani M. Obesity index that better predict metabolic syndrome: body mass index, waist circumference, waist hip ratio, or waist height ratio. J Obes. 2013; 2013:269038.
- Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes Rev 2012; 13:275-286.
- Alberti KG, Zimmet P, Shaw J. The metabolic syndrome--A new worldwide definition. Lancet, 2005; 366:1059-1062.
- Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults: Executive summary of the third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III. JAMA. 2001; 285: 2486-2497.
- Ode JJ, Pivarnik JM, Reeves MJ, Knous JL. Body mass index as a predictor of percent fat in college athletes and nonathletes. Med Sci Sports Exerc. 2007; 39:403-409.
- Roubenoff R. Applications of bioelectrical impedance analysis for body composition to epidemiologic studies. Am J Clin Nutr. 1996; 64:459s-62s.
- Stewart SP, Bramley PN, Heighton R, Green JH, Horsman A, et al. Estimation of body composition from bioelectrical impedance of body segments: comparison with dual-energy X-ray absorptiometry. Br J Nutr. 1993; 69:645-655.
- Deurenberg P, Smit HE, Kusters CS. Is the bioelectrical impedance method suitable for epidemiological field studies? Eur J Clin Nutr. 1989; 43:647-654.
- Lukaski HC, Bolonchuk WW, Hall CB, Siders WA. Validation of tetrapolar bioelectrical impedance method to assess human body composition. J Appl Physiol 1986; 60:1327-1332.
- Camhi SM, Bray GA, Bouchard C, Greenway FL, Johnson WD, Newton RL, et al. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obesity 2011; 19:402-408.
- Barreira TV, Staiano AE, Harrington DM, Heymsfield SB, Smith SR, et al. Anthropometric correlates of total body fat, abdominal adiposity, and cardiovascular disease risk factors in a biracial sample of men and women. Mayo Clin Proc. 2012; 87:452-460.
- Kim SG, Ko K, Hwang IC, Suh HS, Kay S, Caterson I, et al. Relationship between indices of obesity obtained by anthropometry and dual-energy X-ray absorptiometry: The Fourth and Fifth Korea National Health and Nutrition Examination Survey (KNHANES IV and V, 2008-2011). Obes Res Clin Pract. 2015; 9:487-498
- Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gend Med. 2009; 6: 60-75.
- Flegal KM, Shepherd JA, Looker AC, Graubard BI, Borrud LG, Ogden CL, et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. Am J Clin Nutr. 2009; 89:500-508.
- Kuk JL, Janiszewski PM, Ross R. Body mass index and hip and thigh circumferences are negatively associated with visceral adipose tissue after control for waist circumference. Am J Clin Nutr. 2007; 85:1540-144.
- Jia WP, Lu JX, Xiang KS, Bao YQ, Lu HJ, Chen L. Prediction of abdominal visceral obesity from body mass index, waist circumference and waist-hip ratio in Chinese adults: Receiver operating characteristic curves analysis. Biomed Environ Sci. 2003; 16:206-211.
- Kuk JL, Lee S, Heymsfield SB, Ross R. Waist circumference and abdominal adipose tissue distribution: influence of age and sex. Am J Clin Nutr. 2005; 81:1330-1334.
- Janssen I, Heymsfield SB, Allison DB, Kotler DP, Ross R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am J Clin Nutr. 2002; 75:683-688.
- Wu HY, Chen LL, Zheng J, Liao YF, Zhou M. Simple anthropometric indices in relation to cardiovascular risk factors in Chinese Type 2 diabetic patients. Chin J Physiol. 2007; 50: 135-142.
- He Y, Zhai F, Ma G, Feskens EJ, Zhang J. Fu P, et al. Abdominal obesity and the prevalence of diabetes and intermediate hyperglycaemia in Chinese adults. Public Health Nutr. 2009; 12:1078-1084.
- Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev. 2010; 23:247-269.
- Oka R, Miura K, Sakurai M, Nakamura K, Yagi K, Miyamoto S, et al. Comparison of waist circumference with body mass index for predicting abdominal adipose tissue. Obes Res Clin Pract 2009; 83:100-105.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.