Appendiceal Endometriosis: A Rare Cause of Pain and Tenderness in Mc Burney’s Point
2 Department of Surgery All India Institute of Medical Sciences, Rishikesh Veerbhadra Road Uttarakhand, India, Email: sudhirkumar5788@gmail.com
Citation: Rao S, et al. Appendiceal Endometriosis: A Rare Cause of Pain and Tenderness in Mc Burney’s Point. Ann Med Health Sci Res. 2018; 8: 89-92
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Pain in the right in iliac fossa can be a related to organ localized within this quadrant. The most appropriate clinical diagnosis for tenderness in Mc Burney’s point is acute appendicitis. An uncommon cause for pain in the right iliac fossa is endometriosis of appendix. We document a case of 45-year-old lady who presented with pain in the right iliac fossa pain and tenderness in Mc Burney’s point diagnosed clinically as acute appendicitis, which was surgically removed and confirmed by histopathological examination as endometriosis of appendix. This case highlights difficulty in making preoperative diagnosis in this uncommon entity and importance of specimen sampling and histomorphology of appendix for rendering the right diagnosis. In addition, differential diagnosis of endometriosis of appendix should be considered as one of the rare possibility in women particularly when pain is related to menstrual cycle.
Keywords
Appendix; Endometriosis; Mc Burney’s point; Pain; Right iliac fossa
Introduction
Pain in the right iliac fossa may be attributed to various conditions with acute appendicitis being the most common etiology. Other causes include amoebic typhilitis, inflammatory bowel disease, ilieo-caecal tuberculosis, inflammed solitary diverticulum of the caecum and ectopic pregnancy and pelvic inflammatory disease in women. [1,2] In addition to all these, an uncommon etiology of right iliac fossa pain may be an appendicular or caecal endometriosis. [3,4]
A clinical diagnosis of appendicular endometriosis usually is usually not made pre-operatively which in most instances revealed only after histopathological examination of appendix removed for suspected appendicitis. In this case report, we document a case of appendicular endometriosis, which was diagnosed clinically as acute appendicitis due to pain around umbilical region shifting to right iliac fossa and tenderness in Mc Burney’s point.
Introduction
Pain in the right iliac fossa may be attributed to various conditions with acute appendicitis being the most common etiology. Other causes include amoebic typhilitis, inflammatory bowel disease, ilieo-caecal tuberculosis, inflammed solitary diverticulum of the caecum and ectopic pregnancy and pelvic inflammatory disease in women. [1,2] In addition to all these, an uncommon etiology of right iliac fossa pain may be an appendicular or caecal endometriosis. [3,4]
A clinical diagnosis of appendicular endometriosis usually is usually not made pre-operatively which in most instances revealed only after histopathological examination of appendix removed for suspected appendicitis. In this case report, we document a case of appendicular endometriosis, which was diagnosed clinically as acute appendicitis due to pain around umbilical region shifting to right iliac fossa and tenderness in Mc Burney’s point.
Case Summary
A 45-year-old lady was admitted to the surgical out-patient department with complaints of pain around umbilicus and shifting to the right lower abdomen of 4 days duration. This was accompanied by few episodes of non-projectile vomiting, fever and anorexia. There was no significant past medical history. Her menstrual cycles were normal with normal flow. Patient was menstruating at the time of presentation.
On general physical examination, patient was febrile (100°C) and had tachycardia. Per abdomen examination revealed tenderness in the right lower quadrant, especially at Mc Burney’s point. A 6 × 6 cm smooth, tender lump was also palpable in the right iliac fossa.
Ultrasonography of abdomen and pelvis showed features of appendicular lump and no calcified appendicoliths. Complete hemogram was done which revealed leukocytosis with neutrophilic shift to the left.
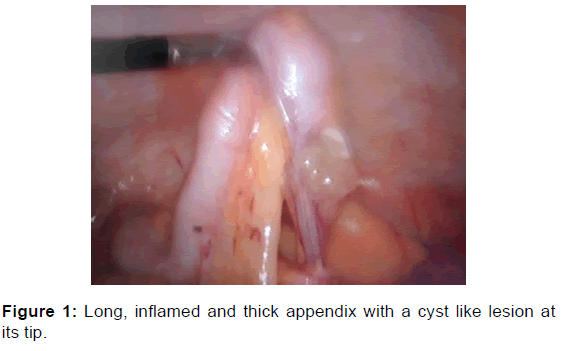
A clinical diagnosis of acute appendicitis was made. In view of presence of appendicular lump, patient was managed conservatively and discharged with a plan of interval appendicectomy. Patient was re-admitted after two months and laparoscopic interval appendicectomy was performed. Per-operative findings included edematous thick and appendix. There was also a cystic swelling present at the tip of appendix [Figure 1]. There was no other abnormality detected as visualized during laparotomy.
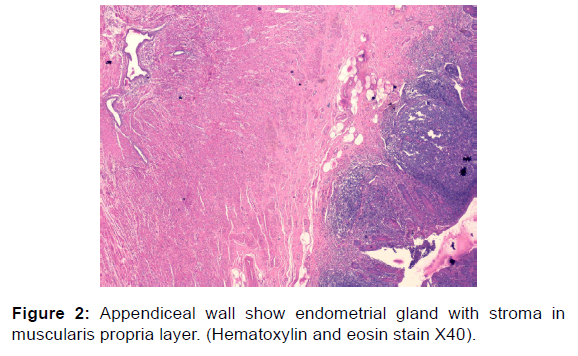
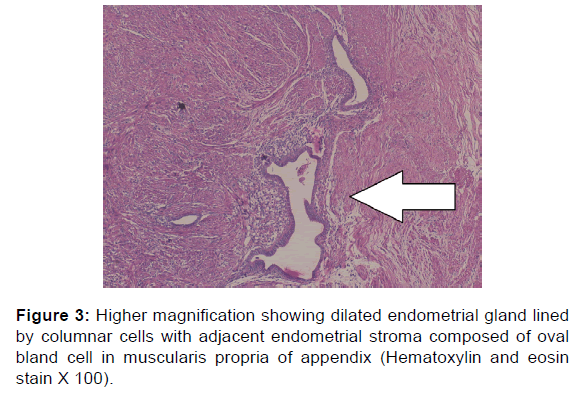
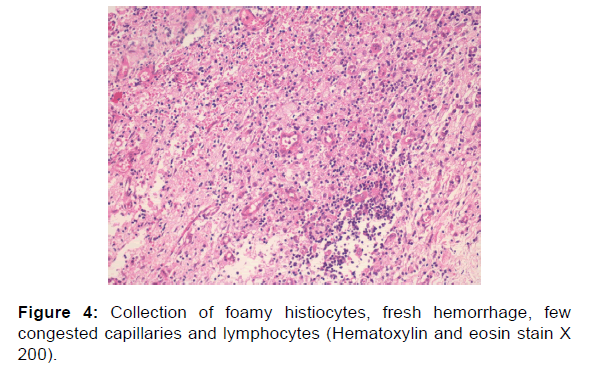
Excised appendix was sent for histopathological examination. Specimen of appendix received measured 5 × 1 × 0.8 cm and gross examination showed congestion on serosal surface and cystic area in tip. Cut section showed lumen with fecolith. Section from tip of appendix showed few endometrial glands and stroma involving serosa and outer layer of muscularis propria in focal areas [Figures 2 and 3] on microscopy. There was also an area showing collection foamy cells, congestion, fresh hemorrhage and edema in the serosa [Figure 4]. Focal aggregates of few lymphocytes were also seen [Figure 4]. Mucosa of the appendix showed reactive lymphoid hyperplasia [Figure 2]. There was no evidence of acute appendicitis on microscopic examination and final tissue diagnosis of appendiceal endometriosis was rendered. On discussion with the surgeons, they conveyed that laproscopy did not show signs of endometriosis anywhere else in the peritoneal cavity.
Discussion
Presence of endometrial glands and stroma in extra-uterine site is termed as endometriosis. Its incidence ranges from 4 to 17% among women of reproductive age group and usually affects females of 25 to 45 years of age. [5,6] Gastrointestinal involvement in endometriosis is not a common finding.
Endometriosis is an estrogen-dependent lesion, occurring commonly in young women, featuring endometrial glands and stromal tissue in extra-uterine location. Common sites of this entity with presence of ectopic endometrial tissue includes ovaries, peritoneum, uterosacral ligaments and rectovaginal cul-de-sac. While involvement of appendix is extremely rare and can mimic acute appendicitis. [7] The main symptom of endometriosis is chronic abdominal pain, and the diagnosis is often made later, mostly after the result of the histopathological examination. Endometriosis of the cecal appendix is rare and almost never diagnosed before the surgery, with the definitive diagnosis obtained only after microscopic examination of tissue. However, it should always be taken into account for the diagnosis of chronic pelvic pain, especially in young women complaining of recurrent pain, history of infertility and pelvic endometriosis.
One third of the infertility cases among females are associated with endometriosis. [5] The specific cause and pathogenesis of endometriosis is not defined. Among the most accepted theories, coelomic metaplasia is mentioned, [6] as well as retrograde menstruation, proposed by Sampson, [8] and the genetic theory, besides blood and lymphatic spread. Ectopic endometrial implants are usually present in the pelvic region, especially the pelvic peritoneum, ovaries, fallopian tubes, and recto-vaginal septum. [3] Review of literature reveals that the incidence of involvement of the gastrointestinal tract varies from 15 to 37% of the cases [1,3,9] and it most commonly affects the rectum and the recto-sigmoid junction accounting for 72 % of the cases. [1,3,9,10] The small intestine involvement is around 7% more likely restricted to the terminal ileum. [10] The less affected sites are the cecum and appendix. Several studies focused on appendicular endometriosis case series show incidence of < 1%. [11,12]
Appendiceal endometriosis is classified into primary and secondary types. Lesion with histopathological evidence of endometriosis within the appendix with no clinico-pathological evidence of extra-appendicular endometriosis is described as primary form while secondary form is associated with features of external endometriosis. Many patients diagnosed with appendiceal endometriosis also suffer from menstrual irregularities and uterine leiomyomas. However, primary appendiceal endometriosis cases have also been reported without involvement of any other gynecological organ. [13]
Based on clinical symptoms, appendiceal endometriosis may be sub classified into four groups: (1) Patient presenting clinically as acute appendicitis; (2) Patient with appendix invagination; (3) Patients presenting with non-specific symptoms like colicky abdominal pain, nausea/vomiting and malena; (4) Cases who are asymptomatic. [14] Finding of an inverted or bulbous appendiceal orifice on colonoscopy suggests a more likely diagnosis of appendiceal endometriosis. Complications that can occur due to endometriosis of the appendix include hemorrhage, intussusception and bowel perforation, a rare complication during 3rd trimester of pregnancy. [15,16] Appendiceal wall affected by endometriosis show secondary changes such as chronic inflammation, fibrosis, hypertrophy/hyperplasia of muscularis propria. The possible mechanism of intussusception could be hyperperistalsis of hypertrophic portion that may be the leading edge for hyperperistalsis making it prone for invagination and intussusception.
Presently there is no investigation that can give definite diagnose of endometriosis pre-operatively. Radio-imaging may also be of not much help for its diagnosis. Although, laproscopy, may be considered as a standard method for diagnosis as features visualized under magnification may give direct clue. However, variable lesions may be noted limiting its importance. Features identified on laproscopy may vary in appearance from black or dark bluish or deep red spots to raised reddish-blue irregularly shaped islands. The lighter lesions can easily be missed which include flame-like patches, whitish opacifications and yellow-brown discoloration. [16,17] If these lesions show mucosal involvement the possible differential diagnosis include Crohn’s disease, cancer and ischemia. The latter lighter lesions can be more frequent and are considered to be more active than the dark lesions. In a study by Stegmann et al revealed positive predictive value of 65% for laproscopic diagnosis of endometriosis. [18] During surgery findings of haemorrhagic peritoneal fluid and gross nodularity of the appendix may be pointer towards endometriotic lesion in appendix. [7]
Common locations of endometriosis in appendix are tip and body. In a study on appendiceal endometriosis by Mittal et al, about 56% showed involvement of body and 44% tip of the appendix while base of the appendix was not involved in any of their cases. [19] A definitive diagnosis of endometriosis can only be given on histopathology. The histologic hallmark of endometriosis includes presence of endometrial glands, stroma, fibrosis, and hemosiderin-laden macrophages. Layers involved by endometriosis of appendix wall include serosa and seromuscular. In the present case, the lesion was localized to tip of appendix and involved serosa and muscularis propria. Histology may not always show definite evidence of endometriosis. Endometriosis responds to hormonal therapy and may shrink and not be visible. [20,21] In women who are already a known case of endometriosis may be on hormonal therapy and in such cases histology may not show endometrial glands and stroma. It becomes a challenging task for a pathologist when endometrial glands are absent or sparse with evidence of may be stroma, which can be termed as stromal endometriosis. It becomes much more difficult when stromal component show changes such as presence of foamy histiocytes, smooth muscle metaplasia, myxoid and decidual change that can mask its true nature. Endometriosis can elicit a response resulting in infiltration of foamy histiocytes with abundant cytoplasm, which can be filled with erythrocytes as noted in our case.
Management of endometriosis of appendix depends on presentation. Symptomatic cases presenting with pain is the most common indication for surgical intervention. Surgical treatment may range from appendectomy, ileocecectomy, and right hemicolectomy depending on the appendicular lesion. Surgery is done with the aim to remove the diseased organ and restore the bowel continuity and function. Non-surgical treatment of superficial spots of endometriosis can be treated with CO2 laser. Acute symptoms tend to resolve with appendicectomy. Lower abdominal pain may quite likely recur due to associated pelvic endometriosis.
Pathologist should be aware of the fact that if appendectomy specimen received for a clinical diagnosis of acute appendicitis, does not show microscopic features of acute appendicitis, adequate sampling/ all embedding of appendix should be done to rule out acute appendicitis or any other etiology and even a rare possibility of endometriosis.
This case report emphasizes, that etiology may not always be related to disease intrinsic to the native tissue. A practical approach in making a clinical diagnosis should include differential diagnosis of extrinsic nature as a rare possibility. In a lady who is a known case of endometriosis, pain in abdomen and pelvic region a diagnosis of endometriosis affecting the specific tissue involved should be considered. This diagnosis should be more strongly suspected clinically, if the pain corresponds to the menstrual cycle. In the present case, pain in the right iliac fossa did correspond to menstrual cycle.
Conclusion
This case highlights that a suspicion of appendiceal endometriosis should also be kept in mind as a rare cause of pain in right iliac fossa, which can simulate an acute appendicitis.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Tanwar R, Jain SK, Bains l. Amoebic colitis presenting as ileocaecal intussusception - A rare case. Malays J Med Sci. 2014; 21: 68-70.
- Ruiz-Tovar J, Reguero-Callejas ME, González Palacios F. Inflammation and perforation of a solitary diverticulum of the caecum. A report of 5 cases and literature review. Rev Esp Enferm Dig 2006; 98: 875-880.
- Pandolfi MP, Borgonovi CA, Luís Cozetto de OA, Satomi CG, Gomes NJ. Appendicular endometriosis as a cause of chronic abdominal pain alone in the right iliac fossa: A case report and literature review. J. Coloproctol Rio J 2012; 32: 79-82.
- Baraket O, Zribi R, Berriche A, Chokki A. Cecal endometriosis as an unusual cause of right iliac fossa. J Postgrad Med 2011; 57: 135-136.
- Orbuch IK, Reich H, Orbuch M, Orbuch L. Laparoscopic treatment of recurrent small bowel obstruction secondary to ileal endometriosis. J Minim Invasive Gynecol 2007; 14: 113-115.
- Bailey HR. Colorectal endometriosis. Perspect Colon Rectal Surg 1992; 5: 251-259.
- Uwaezuoke S, Udoye E, Etebu E. Endometriosis of the appendix presenting as acute appendicitis: A case report and literature review. Ethiop J Health Sci 2013; 23: 69-72.
- Sourial S, Tempest N, Hapangama DK. Theories on the pathogenesis of endometriosis. Int J Reprod Med. 2014; 2014: 179515
- Yantiss RK, Clement PB, Young RH. Endometriosis of the intestinal tract. Am J Surg Pathol 2001; 25: 445-454.
- Macafee CH, Greer HL. Intestinal endometriosis. A report of 29 cases and a survey of the literature. J Obstet Gynaecol Br Emp. 1960; 67: 539-555.
- Collins DC: A study of 50,000 specimens of the human vermiform appendix. Surg Gynecol Obstet 1955, 101: 437-445.
- Berker B, Lashay N, Davarpanah R, Marziali M, Nezhat CH, Nezhat C. Laparoscopic appendectomy in patients with endometriosis. J Minim Invasive Gynecol 2005, 12: 206-209.
- Laskou S, Papavramidis TS, Cheva A, Michalopoulos N, Koulouris C, Kesisoglou I, et al. Acute appendicitis caused by endometriosis: a case report. Journal of Medical Case Reports 2011, 5: 144.
- Emre A, Akbulut S, Yilmaz M, Bozdag Z. An unusual cause of acute appendicitis: Appendiceal endometriosis. Int J. Surg Case Rep 2013; 4: 54-57.
- Sakaguchi N, Ito M, Sano K, Baba T, Koyama M, Hotchi M. Intussusception of the appendix: a report of three cases with different clinical and pathologic features. Pathol Int 1995; 45: 757-761.
- Nakatani Y, Hara M, Misugi K, Korehisa H. Appendiceal endometriosis in pregnancy. Report of a case with perforation and review of the literature. Acta Pathol Jpn 1987; 37: 1685-1690.
- Mettler L, Schollmeyer T, Lehmann-Willenbrock E, Schüppler U, Schmutzler A, Shukla D, et al. Accuracy of laproscopic diagnosis of endometriosis. JSLS 2003; 7: 15-18.
- Jansen RP, Russell P. Nonpigmented endometriosis: clinical, laparoscopic, and pathologic definition. Am J Obstet Gynecol 1986; 155: 1154-1159.
- Stegmann BJ, Sinaii N, Liu S, Segars J, Merino M, Nieman LK, et al. Using location, color, size, and depth to characterize and identify endometriosis lesions in a cohort of 133 women. Fertility and Sterility 2008; 89: 1632-1636.
- Mittal VK, Chouldhury SP, Cortez JA. Endometriosis of the appendix presenting as acute appendicitis. Am J Surg. 1981; 142: 519-521.
- Wood C, Kun R, Tsaltas J. Laparoscopic diagnosis of endometriosis. Australian and New Zealand Journal of Obstetrics and Gynaecology 2002; 42: 277-280.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.