Assessing the Awareness Regarding Sterilization and Disinfection Protocol in Routine Practice among Medical Students in India: A Survey-Based Research
Received: 14-Jan-2024, Manuscript No. amhsr-24-129766; Editor assigned: 16-Jan-2024, Pre QC No. amhsr-24-129766 (PQ); Reviewed: 31-Jan-2024 QC No. amhsr-24-129766; Revised: 07-Feb-2024, Manuscript No. amhsr-24-129766 (R); Published: 14-Feb-2024
Citation: Singh R, et al. Assessing the Awareness Regarding Sterilization and Disinfection Protocol in Routine Practice among Medical Students in India: A Survey-Based Research. Ann Med Health Sci Res. 2024;14:940-943.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Experts and scholars in the fields of dentistry, medicine, and public health persist in uncovering novel and improved methods to halt the transmission of infections. Operatory preparation and disinfection play a crucial role in ensuring the provision of safe care within medical settings. Maintaining proper hand hygiene, utilizing Personal Protective Equipment (PPE) correctly, and effectively disinfecting environmental surfaces, devices, and equipment are crucial elements in preventing the spread of infections. Medical teams are entrusted by patients to maintain the utmost level of infection prevention standards in order to provide a secure care setting. By communicating the implementation of supplementary measures and precautions in the office to ensure patient safety, medical professionals can enhance patient trust in their expertise.
Keywords
Sterilization; Medical practice; Health education
Introduction
Sterilization is one of the key factors responsible for the success of clinical procedure. Without sterilization, clinician is doing more harm rather than providing any benefit to the patient. Using instruments without sterilization is a serious crime and against the values and ethics of medical profession. It is rightly said that a neat and well sterilized operatory build a confidence among clinicians and instills a sense of trust amongst patients towards the operator. Sterilization plays an important role in preventing cross-contamination, containing the spread, breaks the chain of transmission from operator to patients or vice versa [1]. Proper knowledge regarding sterilization procedures, methods of sterilization is mandatory for the health professionals working in clinical area to ensure proper sterilization without any discrepancies. Proper segregation of biomedical waste and its safe disposal also plays a vital role in preventing nosocomial infection.
Sterilization is the process of complete destruction of micro- organisms both in vegetative and spore forms from the surface of object or any substance. Lack of sterilization in routine medical practice will have negative impact on the treatment, despite proper isolation and good skills of operator. Sterilization begins when patient enters the operatory. It ranges from proper hand wash technique to sterilization of instruments [2]. Various methods can be employed to perform sterilization. The crucial health safeguarding element that must be included in a MHCP’s (Medical Health Care Personnel) infection-control program is regular and thorough cleaning and disinfection of all equipment and surfaces. This is because many pathogens can survive on surfaces for extended periods of time and can easily be transmitted from one person to another through contact with contaminated surfaces. Without proper cleaning and disinfection protocols in place, MHCPs run the risk of spreading infections and illnesses to their patients as well as to other staff members [3]. This can lead to outbreaks of infectious diseases, which can be difficult and costly to contain. So, a survey-based research study was designed to assess the knowledge and status regarding sterilization and disinfection of medical operatory among the undergraduate and post graduate medical students in India.
Materials and Methods
The study included 3000 medical students including 2648 undergraduates and 352 postgraduates from different parts of country to assess their understanding regarding sterilization and disinfection of clinical area. All the participating students were informed about the survey study and a sterilization and disinfection questionnaire was given to all the students and their response was noted.
Inclusion criteria
Undergraduates from IIIrd year till internship
Postgraduates opting clinical branch
Exclusion criteria
Students who have assisted<20 patients in medical procedures
Unfilled questionnaire forms
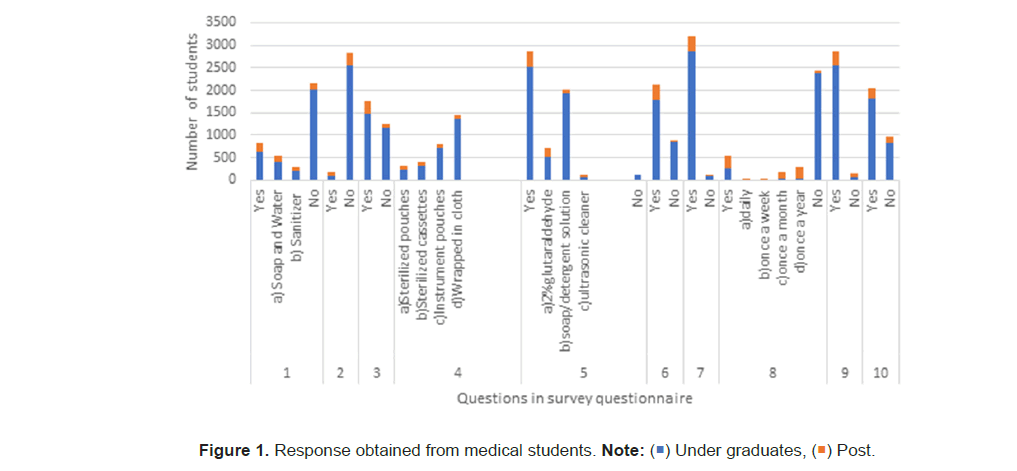
A sterilization/disinfection survey questionnaire was given to the students based on inclusion and exclusion criteria. The survey questionnaire on sterilization and disinfection was carefully designed and administered to a group of students (Figure 1). The researchers took into account specific criteria for inclusion and exclusion to ensure that the participants were suitable for the study. The inclusion criteria were established to ensure that the participants had relevant knowledge and experience in the field of sterilization and disinfection. This ensured that the participants had a basic understanding of the topic and could provide valuable insights. On the other hand, the exclusion criteria were put in place to exclude individuals who did not meet the necessary requirements for the study. The survey questionnaire itself was designed to gather information on various aspects of sterilization and disinfection. It included questions about the participants knowledge of different sterilization methods, their understanding of the importance of disinfection in healthcare settings and their opinions. The questionnaire was administered to the students in a controlled environment, ensuring that they had enough time to carefully read and respond to each question. The researchers also provided clear instructions on how to complete the questionnaire to minimize any potential confusion or misinterpretation. The data collected from survey questionnaire was tabulated and analysed to identify trends, patterns and insights related to sterilization and disinfection. This information will be helpful in improving current practices and developing more effective strategies in healthcare settings.
Results and Discussion
After results revealed that out of 2648 undergraduates, 1082 were interns, 892 from final year and 674 were from third year respectively who participated in this study. In case of 352 post graduate students; 146 were from first year, 112 from second year and 94 were from third year respectively which were part of this study. Information obtained by survey questionnaire was presented (Table 1). It was found that postgraduates and undergraduates lack expertise in the field of sterilization of dental operatory which needs to be reinforced (Graph 1). Although, postgraduates were more aware of infection-control protocol and sterilization methods.
| Serial number | Survey questions | Response | Under graduates | Post graduates | Total |
|---|---|---|---|---|---|
| 1 | Hand Hygiene Technique (WHO recommended) | Yes | 628 | 213 | 841 |
| a) Soap and water | 410 | 149 | 559 | ||
| b) Sanitizer | 218 | 64 | 282 | ||
| No | 2020 | 139 | 2159 | ||
| 2 | Sterilization of new file/instrument | Yes | 84 | 94 | 178 |
| No | 2564 | 258 | 2822 | ||
| 3 | Autoclaving cotton/gauze pieces | Yes | 1466 | 284 | 1750 |
| No | 1182 | 68 | 1250 | ||
| 4 | Autoclaved instruments storage | a) Sterilized pouches | 234 | 88 | 322 |
| b) Sterilized cassettes | |||||
| c) Instrument pouches | 321 | 97 | 418 | ||
| d) Wrapped in cloth | |||||
| 730 | 72 | 802 | |||
| 1363 | 95 | 1458 | |||
| 5 | Instruments clean before autoclaving | Yes | 2525 | 352 | 2877 |
| a) 2% Glutaraldehyde | 530 | 184 | 1870 | ||
| b) Soap/detergent solution | |||||
| c) Ultrasonic cleaner | 1927 | 98 | 520 | ||
| 68 | 70 | 487 | |||
| No | 123 | 0 | 123 | ||
| 6 | Use of sterilization tape for checking autoclave efficacy | Yes | 1798 | 328 | 2126 |
| No | 850 | 24 | 874 | ||
| 7 | Segregation of biomedical waste | Yes | 2864 | 340 | 2894 |
| No | 94 | 12 | 106 | ||
| 8 | Cleaning of sanitary pipes | Yes | 266 | 284 | 550 |
| a) Daily | 3 | 9 | 12 | ||
| b) Once a week | 5 | 39 | 44 | ||
| c) Once a month | 37 | 154 | 191 | ||
| d) Once a year | 27 | 276 | 303 | ||
| No | 2382 | 68 | 2450 | ||
| 9 | Universal precautions for HIV, HCV, HBV cases | Yes | 2566 | 288 | 2854 |
| No | 82 | 64 | 146 | ||
| 10 | Awareness regarding management of needle stick injury | Yes | 1809 | 226 | 2035 |
| No | 839 | 126 | 965 |
Table 1: Response regarding sterilization questionnaire obtained from undergraduates and postgraduate medical students
Improving sterilization/disinfection of medical operatory plays a vital role in ensuring less microbial count and proper implementation of infection-control policies [4]. Antimicrobial handrubs, which clinicians use prior to a medical procedure, aim to minimize the count of microbes that the clinician may transfer. These microorganisms can potentially contaminate Medical Healthcare Personnel (MHCP) and the surfaces of the medical equipment. In order to ensure proper sterilization, it is essential to thoroughly examine, organize, and prepare medical instruments and other supplies. This involves inspecting the cleanliness of the items, assembling them into trays, and securely packaging or placing them into instrument holder for sterilization. Heat-resistant medical instruments are commonly sterilized using three different methods: 1) Autoclaving, which involves steam under pressure, 2) Dry heat, or 3) Unsaturated chemical vapor. Heat-sensitive instruments have the capability to undergo sterilization by being submerged in germicides that have been registered by the FDA as sterilant [5]. In order to prevent the buildup of medical waste, it is imperative for medical health-care facilities to dispose of it on a regular basis [6]. It is recommended that medical professionals consult with the manufacturer of their equipment or water delivery system to determine the optimal method for maintaining water quality that meets the standard of less than 500 CFU/mL, as well as the appropriate frequency for monitoring [7]. It is imperative for any establishment that produces regulated medical waste to develop a comprehensive management plan that adheres to federal, state, and local regulations in order to guarantee the safety of both public health and the environment [8]. Postexposure management plays a crucial role in a comprehensive program aimed at preventing infection following an occupational exposure to blood [9]. There are certain guidelines which offer clinicians and Healthcare Professionals (HCP) direction on determining the appropriate circumstances to consider HIV PEP and provide recommendations for the PEP regimen [10]. The act of maintaining hand hygiene through handwashing or hand antisepsis is highly effective in minimizing the presence of harmful pathogens on the hands [11,12]. It is widely recognized as the most crucial step in mitigating the risk of transmitting infectious agents to both patients and healthcare personnel. Appropriate education and training programmes should be provided to the MHCP and undergraduates and post graduates in medical schools regarding prevention of cross-contamination, sterilization/disinfection protocol, post exposure prophylaxis etc [13]. MHCP are more inclined to adhere to an infection-control program and exposurecontrol plan if they grasp its underlying reasoning [14,15].
Conclusion
To minimize exposure risks, it is essential to establish strict protocols and guidelines for MHCP implementation and maintenance. This includes ensuring that only authorized personnel have access to MHCP systems and that regular security audits are conducted to identify and address any vulnerabilities. In order to effectively educate individuals on sterilization protocol, it is crucial that educational resources are customized to suit their specific educational level, literacy and language proficiency. This ensures that the information is presented in a manner that is easily understandable and accessible to the target audience.
References
- Rutala WA, Weber DJ. Disinfection, sterilization, and antisepsis: An overview. American Journal of Infection Control. 2016;44:e1–e6.
- Allen KW, Humphreys H, Sims-Williams RF. Sterilization of instruments in general practice: What does it entail? Public Health. 1997;111:115–117.
[Crossref] [Google Scholar] [PubMed]
- McNally O, Thompson IM, McIlvenny G, Smyth ETM, McBride N, et al. Sterilization and disinfection in general practice within university health services. J Hosp Infect. 2001; 9:210–214.
[Crossref] [Google Scholar] [PubMed]
- WHO. Guidelines on prevention and control of hospital associated infections. South East Asian Region. 2002.
- Rutala WA, Weber DJ, Healthcare Infection Control Practices Advisory Committee. Guideline for disinfection and sterilization in healthcare facilities. 2008.
- Bansod HS, Deshmukh P. Biomedical waste management and its importance: A systematic review. Cureus. 2023 Feb 3;15:e34589.
[Crossref] [Google Scholar] [PubMed]
- Keah K, Jegathesan M, Tan S, Chan S, Che O, et al. An evaluation of knowledge and awareness of disinfection and sterilization among health care workers. Southeast Asian J Trop Med Public Health. 1995; 26:51–56.
[Google Scholar] [PubMed]
- Datta P, Mohi GK, Chander J. Biomedical waste management in India: Critical appraisal. J Lab Physicians. 2018;10:6-14.
[Crossref] [Google Scholar] [PubMed]
- Garland K. Infection prevention post-exposure protocols. Dimensions of Dental Hygiene. 2019;17:18–20.
- Mathur P. Lippincott Williams & Wilkins; Philadelphia (PA). Hospital acquired infections prevention and control. 1st Edition. 2010.
- WHO. Guidelines on hand hygiene in health care: First global patient safety challenge clean care is safer care. Geneva: World Health Organization. 2009.
- Mohapatra S. Sterilization and disinfection. Essentials of Neuroanesthesia. 2017:929–44.
- Sheth N, Rathod Y, Shenoi P, Shori D, Khode R, et al. Evaluation of new technique of sterilization using biological indicator. Journal of Conservative Dentistry. 2017.
- Chidambaranathan AS, Balasubramanium M. Comprehensive review and comparison of the disinfection techniques currently available in the literature. Journal of Prosthodontics. 2017:1–8.
[Crossref] [Google Scholar] [PubMed]
- Bali RK. Operating room protocols and infection control. Oral and Maxillofacial Surgery for the Clinician. 2020:173–94.

 ) Under graduates, (
) Under graduates, ( ) Post.
) Post.


 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.