Assessment of Quality of Life and Clinical Performance of Immediately Loaded Basal Implants in Prosthetic Rehabilitation of Resorbed Ridges: A Clinico-Radiographic Study
Received: 31-May-2022, Manuscript No. AMHSR-22-65481; Editor assigned: 03-Jun-2022, Pre QC No. AMHSR-22-65481(PQ); Reviewed: 17-Jun-2022 QC No. AMHSR-22-65481; Revised: 01-Aug-2022, Manuscript No. AMHSR-22-65481(R); Published: 08-Aug-2022
Citation: Aggarwal S. Assessment of Quality of Life and Clinical Performance of Immediately Loaded Basal Implants in Prosthetic Rehabilitation of Resorbed Ridges: A Clinico-Radiographic Study. Ann Med Health Sci Res. 2022;12:1-7.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Basal implants are dental implants that employ the basal cortical portion of the jaws for implant retention. These implants are uniquely and specifically designed for the sole purpose of gaining anchorage from the basal cortical bone and have gone through several changes and modifications in the past several decades. The modern basal implant has a sophisticated yet simple design, surgical protocols and is a prosthetic friendly system. These properties have led several practitioners around the globe to include basal implantology in their practices and so far, this system has delivered fairly successful results. Although the use of basal implant supported prosthesis has been documented as an alternative treatment for patients with severe ridge resorption, there is a paucity of knowledge on how this treatment affects patients’ satisfaction and quality of life compared with their previous prosthetic treatment. Majority of the patients whose answer was ‘never’ force were related to inability to function (80.02%) followed by unsatisfactory (71.56%) and generally was satis ied in life (69.56%).
Aim: The aim of this present clinical research was to assess quality of life and clinical performance of immediately loaded basal implants in prosthetic rehabilitation of resorbed edentulous maxillomandibular sites and ridges.
Methods and materials: The study design included the patients desirous of replacement of missing teeth were selected from the OPD of subharti dental college, Swami Vivekanand subharti university. Meerut. BCS implants and BCS-EX implants from simpladent implant solutions, Pvt Ltd, India , surgical starter kit for basal implants, advanced handgrip surgical kit, addition silicone elastomeric impression material (3 M ESPE India), physiodispenser (NSK), metal cutting carbide burs, articulating papers (30 G, 18 G Bausch) were used in this study.
Statistical analysis used: All the values obtained during the study were expressed in the form of mean, Standard deviation and standard error of mean. The parameters were compared between groups using paired t-test for intragroup comparison at a similar time i.e., baseline, 1 month and 3 months. The data collected was comprehensively analysed using SPSS software.
Results: A total of 11 study participants (6 males and 5 females) with resorbed alveolar bone were included in the study. A total of 58 implants were placed of which 32 implants were placed in maxilla and 26 implants in mandible. In 2 patients, full arch implants were placed. In 1 patient, full mouth implant rehabilitation was done and in 3 patients, 4 implants were placed in posterior segment and in 5 patients, implants were placed in anterior maxilla and mandible. All patients were satis ied with respect to chewing ability, speech and aesthetics.
Conclusions: The influence of basal implants on patients’ oral health related to quality of life as depicted by (OHIP-14) and patients’ perceptions and expectations may guide the clinician in providing the best basal implant services. Basal implant supported prosthesis in edentulous and partially edentulous patients have a positive impact on patient satisfaction and hence enhance the quality of life. They can play a vital role in rehabilitation of patient, where compromised quality and quantity of bone is present.
Keywords
Basal implants; Bi-Cortical Screw (BCS); Bi-cortical engagement; Corticalization
Introduction
Restoring the edentulous maxilla or mandible with implants has become a normal predictable treatment today. This breakthrough in the oral rehabilitation was initiated by the discovery that dental implants, made up of commercially pure titanium can achieve anchorage in the jawbone with direct bone to implant contact. Two different approaches for immediate loading of dental implants or currently known. The first approach relies on the compression screw principle. Screw implants of this type can result in lateral condensation of spongy areas. Implant stability is greatly increased by a mechanism that could be regarded as ‘’corticalization’’ of spongy bone (KOS). The second approach is to establish cortical encourage of thin screw implants Biortical Screw (BCS) or basal implant. Excellent primary stability can be obtained along the vertical surfaces of these implants with no need for corticalization. Implants of this type are, therefore, well suited not only for immediate loading but also for immediate placement [1,2]. According to the concept of basal implantology, the jawbone comprises of two parts the tooth bearing alveolus or crestal part and the basal bone. The crestal bone is less dense in nature and is exposed to infections from tooth borne pathologies, injuries or iatrogenic factors and is therefore subject to higher rate of resorption whereas the basal bone is heavily corticated and is rarely subjected to the infections and resorption [3]. It is the basal bone that can offer excellent support to the implants because patients with severe ridge resorption. There is a paucity of knowledge on how this treatment affects patients’ satisfaction and quality of life compared with their previous prosthetic treatment of its densely corticated nature, at the same time the load-bearing capacity of the basal bone is many times higher than that offered by spongy crestal bone [4]. Basal implants are dental implants that employ the basal cortical portion of the jaws for implant retention. These implants are uniquely and specifically designed for the sole purpose of gaining anchorage from the basal cortical bone and have gone through several changes and modifications in the past several decades [5]. Although the use of basal implant supported prosthesis has been documented as an alternative treatment.
Material and Methods
Subjects
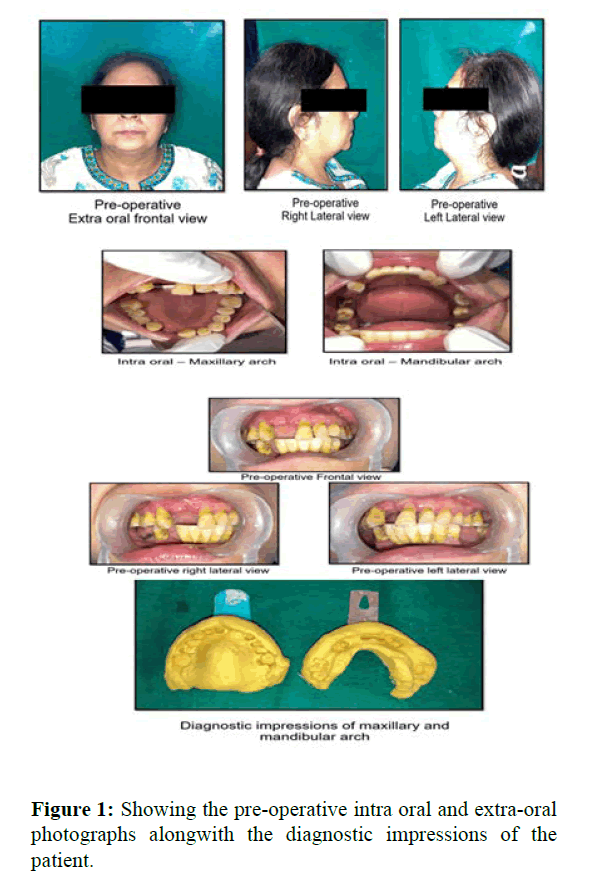
A total of 11 study participants (6 males and 5 females) with resorbed alveolar bone were included in the study. A total of 58 implants were placed of which 32 implants were placed in maxilla and 26 implants in mandible. In 2 patients, full arch implants were placed. In 1 patient, full mouth implant rehabilitation was done and in 3 patients, 4 implants were placed in posterior segment and in 5 patients, implants were placed in anterior maxilla and mandible. Prior to the surgery, a detailed history of the patient was taken which included chief complaint, medical history, dental history, intra and extra oral examination. Patients’ photographs were taken for the records and diagnostic impressions were made. Routine pre-operative preparations were performed which included Blood investigations (Hb, BT, CT. PT, INR), CBCT and IOPA (Figure 1).
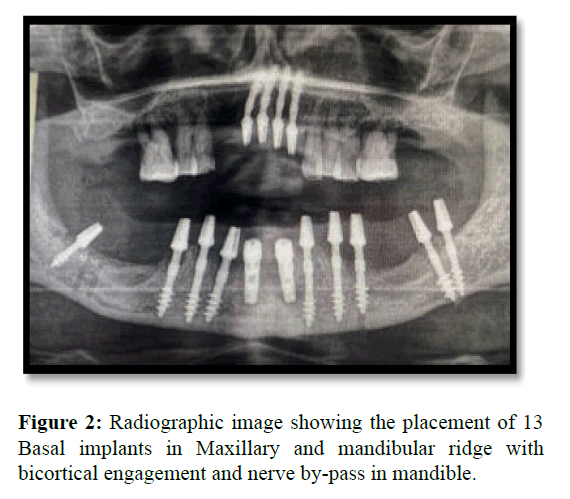
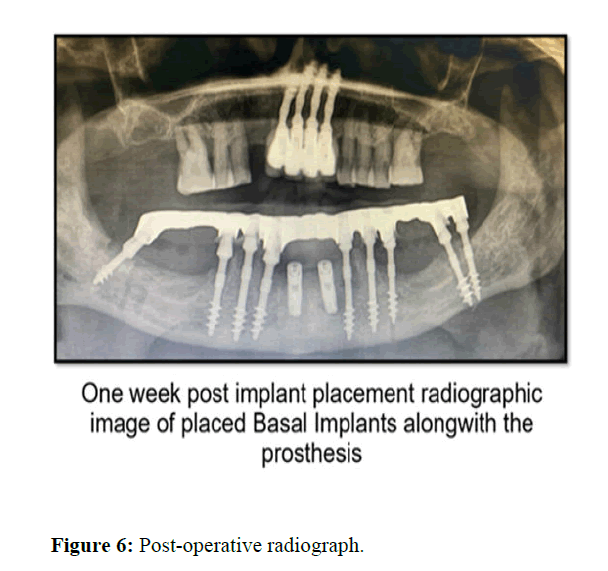
On the day of surgery, local infiltration of LA (lignocaine 2% was given around the edentulous site. The BCS starter kit and advanced hand griped kit was utilised to drill under copious irrigation of normal saline into the edentulous surgical sites with the help of physiodispensor. Implant length and diameter were determined by OPG and CBCT. An initial drilling of the implant site was made; a 2 mm diameter drill was used to prepare the implant site and to subjectively discriminate bone quality into hard or soft. For maxillary bone, the drill drilling speed was kept at to 20,000 rpm with 1:1 surgical hand piece. For mandible, the drilling speed was 2000 rpm with torque setting at 40 Ncm in physiodispenser. In maxilla, after drilling the first cortical i.e., a regular cortex the drilling was continued till 2nd or 3rd basal bone cortex (Nasal Floor or nasomaxillary buttress or sinus Floor or pterygoid apophysis. In mandible, after drilling the first cortical alveolar cortex, the drilling was continued deep to engage dense bone but no lingual cortical bone was drilled in the interforaminal region. In mandibular posterior region either lingual cortical or buccal cortical bone was drilled. In all cases the BCS implants were placed ensuring a bicortical engagement with dense basal bone so as to have a good primary stability. After placement of all the implants an OPG of the patient was taken to check the final position and angulation of placed basal implants. Postoperatively, patients were prescribed analgesics and antibiotics for 5 days (Figure 2).
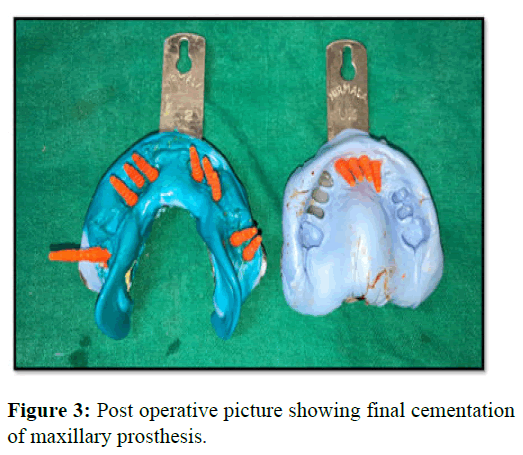
After having completed the implant placement, the implant neck was bent if required to give proper alignment for optimal prosthetic rehabilitation. Impression caps were placed and impression was made using addition silicone elastomeric impression material and tentative jaw relation was recorded using Alu wax. Cast were poured and sent to lab (Figure 3).
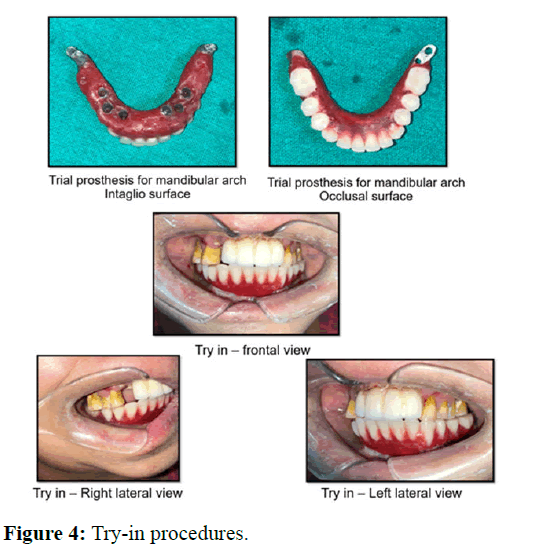
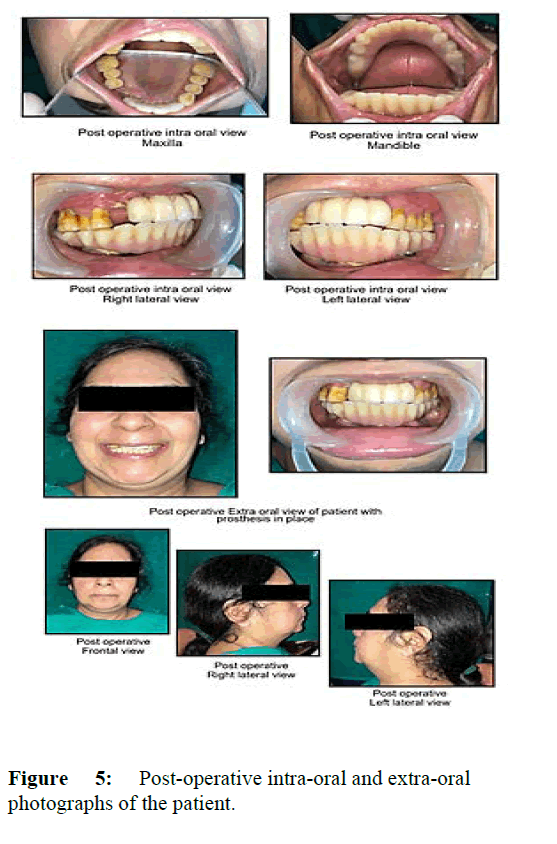
On second day after adjustment of the metal framework in patients’ mouth and completion of try-in, occlusal wax rims were made on the framework and definitive intermaxillary records were made (Figures 4-6).
Results
A total of 11 study participants (6 males and 5 females) with resorbed alveolar bone were included in the study. A total of 58 implants were placed of which 32 implants were placed in maxilla and 26 implants in mandible. In 2 patients, full arch implants were placed. In 1 patient, full mouth implant rehabilitation was done and in 3 patients, 4 implants were placed in posterior segment and in 5 patients, implants were placed in anterior maxilla and mandible. All patients were satisfied with respect to chewing ability, speech and aesthetics. Table 1 shows the result of which clinical parameters recorded at specified time intervals.
| Table 1: Clinical parameters recorded at specified time intervals. | ||||||
|---|---|---|---|---|---|---|
| Clinical parameters | BASELINE | 3 DAYS | 7 DAYS | 1 Months | 3 Months | 6 Months |
| 1.Mobility (P) | 1 day | 0.11 ± 0.47 | 0.11 ± 0.32 | 0 ± 0 | ||
| 0-1<0.05*(S) | ||||||
| 0-3<0.05*S | 1-3>0.5 (NS) | 3-6<0.05*(S) | ||||
| 0-6>0.05 (NS) | 1-6<0.05* (S) | |||||
| 2. Periimplant bone level with IOPAR (P for both M and D) | M 1.65 ± 0.66 | 1.50 ± 0.77 | 1.61 ± 0.71 | |||
| D 1.78 ± 0.91 | 1.46 ± 0.70 1.32 ± 0.77 |
|||||
| >0.05 NS | ||||||
| 3. Periimplant bone level with CBCT (P) | M 1.88 ± 0.45 | M 1.8 ± 0.13 | ||||
| D 1.79 ± 0.56 | D 1.54 ± 0.46 | |||||
| B 1.92 ± 0.37 | B 1.30 ± 0.52 | |||||
| L 2.12 ± 0.92 | L 2.05 ± 0.15 | |||||
| >0.05 NS | > 0.05 NS | |||||
| 4. Pain score (P) | 7.52 ± 1.26 | 5.12 ± 1.1 | 1.85 ± 1.2 | 0 ± 0 | 0 ± 0 | 0 ± 0 |
| <0.05*(s) | <0.5*(S) | <0.5*(S) | >0.05 NS | >0.05 NS | >0.05 NS | |
| 5. Sulcular bleeding (P) | 1.52 ± 0.31 | 1.62 ± 0.31 | `1.21 ± 0.33 | |||
| <0.05*(S) | <0.05*(S) | <0.05*(S) | ||||
| 6. Suppuration | 0 | 0 | 0 | 0 | 0 | |
P<0.05*Significant, >0.05 Non significant M-Mesial, D-Distal, B-Buccal, L-Lingual
Table 2 represents the distribution of responses to OHIP-14 items. The distribution of the patient's response was almost uniform to all the OHIP-14 items. Less percentage of patients reported having problems very frequently in past one year. Mean score ranged between points 0.45 for unable to function to 1.25 for having being self-conscious. Majority of the patients whose answer was ‘never’ force were related to inability to function (80.02%) followed by unsatisfactory (71.56%) and generally was satisfied in life (69.56%). More complaints were reported by the patients for becoming selfconscious (46.65%) followed by trouble in pronouncing words (50.91%). According to the observation from questionnaire response, majority of the participants were contended with their oral health and implant placement.
| Table 2: Oral Health Impact Profile (OHIP-14) questionnaire. | |||||||
|---|---|---|---|---|---|---|---|
| Dimension | Variables | 0 | 1 | 2 | 3 | 4 | mean |
| Functional limitation | Have you had trouble pronouncing any words because of problems with your teeth, mouth or dentures? | 50.91 | 16.25 | 20.3 | 10.1 | 2.38 | 1.04 |
| Have you felt that your sense of taste has worsened because of problems with your teeth, mouth or dentures? | 56.56 | 14.21 | 14.1 | 9.72 | 5.46 | 0.97 | |
| Physical pain | Have you had painful aching in your mouth? | 58.32 | 21.72 | 10.8 | 5.34 | 3.8 | 0.77 |
| Have you found it uncomfortable to eat any foods because of problems with your teeth, mouth or dentures? | 52.08 | 15.3 | 15.1 | 9.78 | 8.71 | 1.2 | |
| Psychological discomfort | Have you been self-conscious because of your teeth, mouth or dentures? | 46.65 | 17.47 | 16.2 | 7.69 | 12 | 1.25 |
| Have you felt tense because of problems with your teeth, mouth or dentures? | 52.9 | 15.4 | 15.1 | 6.2 | 10.4 | 1.12 | |
| Physical disability | Has your diet been unsatisfactory because of problems with your teeth, mouth or dentures? | 71.56 | 20.82 | 2.08 | 2.26 | 3.26 | 0.5 |
| Have you had to interrupt meals because of problems with your teeth, mouth or dentures? | 64.13 | 20.65 | 7.6 | 5.43 | 2.17 | 0.61 | |
| Psychological disability | Have you found it difficult to relax because of problems with your teeth, mouth or dentures? | 56.52 | 20.65 | 9.78 | 8.69 | 4.34 | 0.84 |
| Have you been a bit embarrassed with other people because of problems with your teeth, mouth or dentures? | 52.17 | 18.47 | 17.4 | 7.6 | 4.34 | 0.93 | |
| Social disability | Have you been a bit irritable with other people because of problems with your teeth, mouth or dentures? | 61.4 | 12.35 | 11 | 9.35 | 5.88 | 0.85 |
| Have you had difficulty doing your usual jobs because of problems with your teeth, mouth or dentures? | 54.43 | 20.65 | 12 | 5.43 | 7.6 | 0.91 | |
| Handicap | Have you felt that life in general was less satisfying because of problems with your teeth, mouth or dentures? | 69.56 | 21.72 | 2.46 | 3.17 | 3.09 | 0.49 |
| Have you been totally unable to function because of problems with your teeth, mouth or dentures? | 80.02 | 10.47 | 4.36 | 3.36 | 1.79 | 0.45 | |
Never (=0), Hardly ever (=1), Occasionally (=2), Fairly even (=3), Very often (=4)
Discussion
According to the concept of basal implantology, the jawbone comprises of two parts-the tooth bearing alveolus and the basal bone [6]. The crestal bone is less dense in nature is exposed to infection from to the bone pathologies, injuries or iatrogenic factors and is therefore subjected to a higher rate of resorption whereas; the basal bone is heavily decorticated and is rarely subjected to infections and resorption [7]. An orthopaedician uses a large fixation plate to rehabilitate the patients with trauma, example: Femur bone-most load bearing joint in the body. The fixation screws run from one side of the cortical to the opposite side the screws use the cortical on both side of the femur bone to stabilize the fracture segments and the patient is mobilized in 2-3 days following surgery. Applying the same concept in the jaw bone, we can engage basal implants in the basal bone (bicortical anchorage). Excellent support can be derived for the implants allowing them to be loaded immediately [8].
Conclusion
In this study, Basal Cortical Screw (BCS) implants were placed in all 11 cases. All the implants were of Simpladent immediate loading dental implant system. BCS implants are highly polished smooth surface all through the neck shaft and spiral. Unlike rough surface implants, BCS implants can be used in infected sockets. Its sharp threads help to establish good primary stability. These implants have bendable neck which allows for establishing parallelism. The smooth surface of BCS implants helps to prevent peri-implantitis and bacterial colonization. In the present study, it was observed that pain was maximum on day 1 (mean 7.52 ± 1.20) and decreased later on significantly on day 7 (mean 1.85 ± 1.20). The mean peri-implant bone loss measured at 6 months postoperative was 0.08 mm on mesial side, 0.15 mm distal side, 0.6 mm on buccal side and 0.11 mm on palatal side. At the end of study, none of the 58 BCS implants had any mobility.
References
- Gupta A, Madan B, Bakshi M, Garg M. Full Mouth Rehabilitation with Immediate Loading Basal Implant. Int J Pre and Clin Dent Res, 2017;4:1-3.
- Sharma R, Prakash J, Anand D, Hasti A. Basal Implants- An alternative treatment modality for atrophied ridges. Int J Res Dent. 2016;6:60-65.
- Gupta AD, Verma A, Dubey T, Thakur S. Basal Osseointegrated Implants: Classification and Review. Int J Cont Med Res; 2017;11:2329-2454.
- Narang S, Narang A, Jain K, Bhatia V. Multiple immediate implants placement with immediate loading. J Indian Soc Periodontol. 2014;18:648-650.
- Yadav RS, Sangur R, Mahajan T, Rajanikant AV, Singh N, Singh R. An Alternative to Conventional Dental Implants: Basal Implants. Rama Univ J Dent Sci 2015;2:22-28.
- Ihde Stefan (2005) Principles of BOI- Clinical, Scientific and Practical Guidelines to 4-D Dental implantology. Heidelberg Springer, New York.1-12.
- Niswade Grishmi, Mishra Mithl. Basal Implants – A Remedy for Resorbed Ridges. Wor J Pharma Life Sci. 2017;3:565-572.
- Babita Y, Neha C, Nazish B, Gaurav T, Pranit K. Basal Osseointegrated Implants. Int J Adv Heal Sci. 2016;3:1-8.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.