Awareness of Blood Donation in General Population-The Cross-Sectional Analytical Study
2 Department of Community, Medicine Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences Sawangi (Meghe), Wardha, India
Published: 30-Jul-2021
Citation: Jagadish M, et al. Awareness of Blood Donation in General Population: The Cross-Sectional Analytical Study. Ann Med Health Sci Res. 2021;11:28-32.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Blood donation is very vital to save human life as there is no substitute for human blood. Blood transfusion is an essential component of the health care system of every country and patientswho require blood transfusion service as part of the clinical management of their condition have the right to expect that sufficient and safe blood will be available to meet their needs. However, this is not always the case, especially in developing countries. To recruit and retain adequate regular voluntary non-remunerated blood donors the motivators and barriers of donors must be understood. Equally important to this goal is the knowledge of blood donors.
Method: This study was a cross-sectional study with purposive sampling, was done in the OPD patients of Shalinitai Meghe hospital and research center and Datta Meghe Medical college, Nagpur in collaboration with ABVRH, Sawangi (Meghe). After obtaining verbal consent, the data was collected by a pre-designed, pre-structured questionnaire. The data was analyzed using SPSS version 26.
Result: A total of 323 People took part in the study, with an average age of 35.6±6.53. Out of the 323, 121(37.5%) were donors and 202(62.5%) were non-donors. The majority of the donors were between the ages of 31 and 40 years old (48.5%), males (63.1%), singles (40.4%), and graduates (45%). The majority of donors (69.4%), 48.8%, had donated 2-5 times, 24.8% were frequent donors, and 37.1%donated annually. “No request for blood” (63.4%)was the most common reason given by non-donors for not donating blood. Around 218(67.5%) said they would be willing to be voluntary donors in the future, whereas 72(22.3%) said they would only donate for family and friends, and 33(10.2%) said they would not donate blood. Age, education, source of information, and kind of donationblood were all found to have a major impact on willingness to donate.
Conclusion: Males and those with a higher education were the most likely to donate blood. Donors saw blood donation as a humanitarian cause, and they felt it provided them with more moral gratification than non-donors. Non-donors were more likely than donors to believe that blood donation causes weakness/anaemia and is damaging to their health.
Keywords
Blood donation; Donors; Non-donors; Voluntary donation; Attitude
Introduction
Blood donation is still the most common source of blood and blood components in the world. Even though there has been a lot of promising research, there is no true substitute for blood and blood components. [1] Donated blood is crucial in the treatment of a variety of disorders. It is the most important lifesaving measure for someone who has lost a substantial amount of blood due to accidents, haemorrhages, or surgery. [2,3]
The majority of the blood used in transfusions comes from unpaid, volunteer donors. [4] Despite the fact that over a million blood units are collected each year, many more are required to meet worldwide demand and maintain the adequate and timely supply of blood. However, demand and supply are not equal; in fact, demand is increasing. [2]
A vital component of any healthcare system is blood transfusion. It is a life-saving treatment for a variety of serious illnesses, including bleeding disorders, haematological disorders, and cancer. [4] Blood donations, whether voluntary unpaid or recruited paid, can help to ensure an adequate blood supply. If the blood isn’t needed for therapy, it can be used for study. For the following reasons, blood banks are attractive for biomedical research projects. [3] For starters, blood banks are convenient locations for gathering a large sample of well-characterized and healthy individuals for genomes and epidemiological screening studies. Second, having donors contact information allows individuals to be contacted again for more samples. [5] Finally, blood donors are expected to have a favourable attitude toward volunteer blood sampling research. However, it is possible that the use of donated blood for research purposes will dissuade some current and potential blood donors from donating blood in the future. [4]
According to evidence, the world collects 112.5 million units of blood each year. In affluent countries, more than half of these blood units are collected. [1] When compared to low-income countries, the rate of blood donation per 1000 people in highincome countries is more than five times higher (33.1 donations vs. 4.6 donations). In rich countries, voluntary blood donors account for over 90% of donations, while in poorer ones, they account for less than half. [2]
Materials and Methods
This study used face-to-face interviews with translated questionnaires to conduct a cross-sectional analytical analysis on 323 adult residents of Nagpur. A set of questions was used to test knowledge and attitude levels, and individuals who answered above the mean for knowledge and attitude questions were classified as having an above-average knowledge level and a favourable attitude, respectively. At Datta Meghe Medical College (DMMC) Wanadongri, Nagpur and Shalinitai Meghe Hospital and Research Center (SMHRC), Nagpur in collaboration with ABVRH, Sawangi (Meghe).
Sample size
The sample size was calculated using Epi info 7 TM software for a population survey based on the prevalence of positive attitudes about blood donation (52.5%). which resulted in the greatest sample size. The sample size was determined to be 323 using a 95% confidence interval and a 5% margin of error, as well as a 5% non-response rate.
Inclusion criteria
The study comprised those who were willing to participate and was between the ages of 18 and 65 (the age range for blood donation according to Indian blood bank rules). [3]
Exclusion criteria
Adults who were critically ill were not included in the study.
Sample collection
For data collection, a simple random sampling procedure was used, including face-to-face interviews utilising a structured and semi-structured pre-tested questionnaire prepared. The survey was written in both Hindi and Marathi.
Statistical analysis
A data documentation sheet was created and utilized to create a data entry form in Epi info 7, as well as check instructions to prevent out-of-range and unlawful values. After data was coded and input into EPI info version 7, it was cleaned and analysed using SPSS version 25. The results were presented using tables and narratives, with frequencies and percentages for categorical variables and averages and standard deviations for numerical variables. Wherever possible, the Chi-square test was used, and a p value of <0.05 was considered statistically significant.
Result
A total of 323 workers took part in the research. They ranged in age from 18 to 51 years old, with a mean age of 35.6 ± 6.53. The gender breakdown was nearly equal, with 160 (49.5%) males and 163 (50.5%) females. However, statistically significant associations for blood donation were discovered for age group, gender, type of family, and education. The donors were predominantly in the age group 31 years-40 years. (48.5%), men (63.1%), single (40.4%), and graduates (45%) [Table 1 and Table 2].
| Particulars | Frequency N (%) | Donors N (%) | Non-donors N (%) | χ2 value | df | P value | |
|---|---|---|---|---|---|---|---|
| Age groups | ≤ 30 Yrs | 188 (58.2) | 61 (32.4) | 127 (67.6) | 7.6639 | 2 | 0.0216 |
| 31-40 Yrs | 101 (31.3) | 49 (48.5) | 52 (51.5) | ||||
| >40 Yrs | 34 (10.5) | 11 (32.4) | 23 (67.6) | ||||
| Gender | Male | 160 (49.5) | 101 (63.1) | 59 (36.9) | 89.1337 | 1 | <0.00001 |
| Female | 163 (50.5) | 20 (12.3) | 143 (87.7) | ||||
| Religion | Hindu | 313 (96.9) | 116 (37.1) | 197 (62.9) | 0.6925 | 1 | 0.4053 |
| Muslim | 10 (3.1) | 5 (50.0) | 5 (50.0) | ||||
| Residence | Urban | 200 (31.9) | 79 (39.5) | 121 (60.5) | 0.9318 | 1 | 0.3344 |
| Rural | 123 (38.1) | 42 (34.1) | 81 (65.9) | ||||
| Marital Status | Single | 109 (33.8) | 43 (39.5) | 66 (60.5) | 0.2902 | 2 | 0.8649 |
| Married | 211 (65.3) | 77 (36.5) | 134 (63.5) | ||||
| Widow | 3 (0.9) | 1(33.3) | 2 (66.7) | ||||
| Type of family | Nuclear | 204 (63.1) | 81 (39.7) | 123 (60.3) | 6.071 | 2 | 0.048 |
| Joint | 59 (18.3) | 14 23.7 | 45 (76.3) | ||||
| Three generation | 60 (18.6) | 26 (43.3) | 34 (56.7) | ||||
| Education | Illiterate | 13 (4.0) | 2 (15.4) | 11 (84.6) | 9.7042 | 4 | 0.0471 |
| Primary school | 19 (5.9) | 6 (31.6) | 13 (68.4) | ||||
| High school | 51 (15.8) | 20 (39.2) | 31 (60.8) | ||||
| Diploma course | 91 (28.2) | 26 (28.6) | 65 (71.4) | ||||
| Graduate | 149 (46.1) | 67 (45.0) | 82 (55.0) | ||||
| Total | 323 (100) | 121 (37.5) | 202 (62.5) |
Table 1: Socio-demographic factors affecting blood donation.
| Particulars | Frequency | Percentage(%) | |
|---|---|---|---|
| Type of donation | Family | 84 | 69.4 |
| Replacement | 37 | 30.6 | |
| Friends | 19 | 15.7 | |
| First time donated for | Family | 8 | 6.6 |
| Relatives | 18 | 14.9 | |
| Unknown | 76 | 62.8 | |
| Once | 36 | 29.8 | |
| Frequency | (2-5) | 59 | 48.8 |
| (6-10) | 15 | 12.3 | |
| >10 | 11 | 9.1 | |
| Regular donation | Yes | 30 | 24.8 |
| No | 91 | 75.2 | |
| Frequency of regular donation | 3 Months | 40 | 33.1 |
| 6 Months | 36 | 29.8 | |
| Yearly | 45 | 37.1 | |
Table 2: Blood donation among the donors.
In this study, 121 (37.5%) of the participants were donors, while 202 (62.5%) were non-donors. Table 2 lists the donors’ blood donation information.
Blood donation was viewed as a humanitarian cause by 99.2% of donors, and it provided moral gratification to 97.5% of nondonors (p=0.001). Non-donors were more likely than donors (p=0.000) to believe that blood donation causes weakness/anaemia (39.1%) and is damaging to health (29.7%). Donors, on the other hand, were more likely than non-donors to assume that blood donation can spread HIV infection (p=0.000). Donors also believed that blood donating causes them to age faster, have infertility, and lose vitality than non-donors, however this was not statistically significant (p>0.05) [Table 3].
| Sr. No. | Blood donation | Donors (%) (Total 121) | Non-donors (%) (Total 202) |
P value |
|---|---|---|---|---|
| 1 | Saves lives | 119 (98.3) | 200 (99.0) |
0.43 |
| 2 | Is a humanitarian cause | 120 (99.2) | 177 (87.6) |
0.01 |
| 3 | Gives moral satisfaction | 118 (97.5) | 168 (83.2) |
0.001 |
| 4 | Can transmit HIV infection | 80 (66.1) | 92 (45.5) | <0.00001 |
| 5 | Leads to weakness/anaemia | 31 (25.6) | 79 (39.1) | 0.083 |
| 6 | Donation is harmful to health | 14 (11.6) | 60 (29.7) | <0.00001 |
| 7 | Leads to accelerated aging | 19 (15.7) | 17 (8.4) | 0.095 |
| 8 | Leads to infertility and loss of vitality | 8 (6.6) | 14 (6.9) | 0.669 |
Table 3: Factors affecting blood donation.
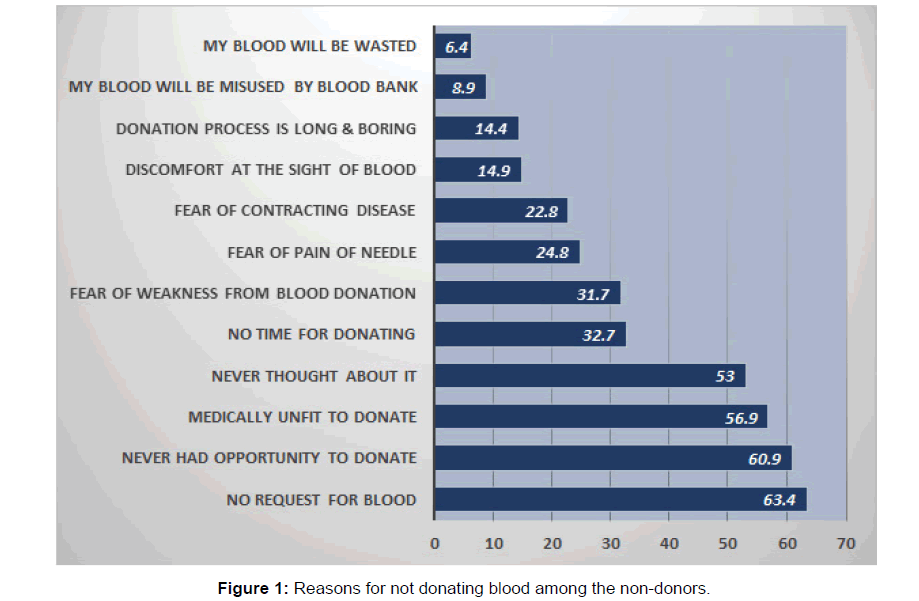
No request for blood (63.4%) was the most common reason given by non-donors, followed by Never had opportunity to donate (60.9%), Medically unfit to donate (56.9%), Never thought about it (53%), and No time for donating (32.7%), Fear of blood donation causing weakness (31.7%), fear of needle pain (24.8%), fear of catching disease (22.8%), discomfort at the sight of blood (14.9%), donation process is long and dull (14.4%), my blood would be exploited by the blood bank (8.9%), and my blood will be wasted (6.4%) [Figure 1].
In this study, 218 (67.5%) people said they would be willing to be voluntary donors in the future, whereas 72 (22.3%) said they would only donate for family and friends, and 33 (10.2%) said they would not donate blood. The majority of donors (86%) were more inclined to be voluntary donors than non-donors (56.4%), a statistically significant difference (p=0.000) [Table 4]. [6]
| Blood donation in the future | |||||||
|---|---|---|---|---|---|---|---|
| Particulars | No N (%) | Only if family/friends | Yes, as a voluntary | χ2 value | df | P value | |
| Blood donation | |||||||
| Donors | 3 (2.5) | 14 (11.6) | 104 (86.0) | 31.08 | 2 | <0.00001 | |
| Non-Donors | 30 (14.9) | 58 (28.7) | 114 (56.4) | ||||
| Gender | Male | 10 (6.3) | 34 (21.3) | 116 (72.5) | 5.466 | 2 | 0.065 |
| Female | 22 (13.5) | 38 (23.3) | 103 (63.2) | ||||
| Age groups | ≤ 30 yrs | 14 (7.4) | 53 (28.2) | 121 (64.4) | 15.726 | 4 | 0.034 |
| 31-40 yrs | 11 (10.9) | 14 (13.9) | 76 (75.2) | ||||
| >40 yrs | 8 (23.5) | 5 (14.7) | 21 (61.8) | ||||
| Education | Illiterate | 6 (46.2) | 3 (23.1) | 4 (30.8) | 30.318 | 8 | 0.0001 |
| Primary school | 4 (21.1) | 1 (5.3) | 14 (73.7) | ||||
| High school | 4 (7.8) | 15 (29.4) | 32 (62.7) | ||||
| Diploma course | 11 (12.1) | 21 (23.1) | 59 (64.8) | ||||
| Graduate | 8 (5.4) | 31 (20.8) | 110 (73.8) | ||||
| Source of information | Books | 2 (3.1) | 22 (34.4) | 40 (62.5) | 23.241 | 6 | 0.0007 |
| Media/Internet | 5 (11.6) | 9 (20.9) | 29 (67.4) | ||||
| Heard from other people | 20 (16.5) | 29 (24.0) | 72 (59.5) | ||||
| Type of donation | Blood bank | 5 (5.3) | 12 (12.6) | 78 (82.1) | 10.33 | 2 | 0.0057 |
| Voluntary | 2 (2.4) | 4 (4.8) | 78 (92.9) | ||||
| Replacement | 0 | 10 (27.0) | 27 (73.0) | ||||
Table 4: Factors affecting the willingness to donate blood in the future.
Discussion
Blood is something that everyone needs at some point in their lives. Because human blood donation is the only means to obtain blood, it is critical to determine what variables inspire donors to donate voluntarily and regularly, as well as what hinders nondonors from doing so.
In this study, 37.5% of the participants were donors, which is comparable to a study of health workers but higher than studies of students. [4,5,7,8] The majority of the donors were between the ages of 31 and 40, with the younger and older age groups donating less. However, only gender, type of family, and education status were found to have a significant relationship with blood donation, with males donating more than females (p=0.00001) and those from higher education donating more than those from lower education (p=0.0471). Other investigations have found a similar male majority among the donors. [4,5,9] Related studies were reported by Chandi et al., [10] Gupta et al., [11,12] and Balwani et al. [13,14]
The reasons for giving blood and non-giving were comparable to those found in prior research. Those who donated blood more frequently did so because it gave them a sense of moral fulfilment. [8,9] The primary reason for not donating was that they were not asked for it or that they did not have the opportunity to do so. [7] Related studies from Global burden of disease studies were reviewed. [15-17]
Voluntary donors also donated more frequently than replacement donors, and they were also more willing to donate in the future (p=0.0057). Even while 89.8% said they would donate in the future, only 67.5% said they would donate voluntarily, with the remaining 22.3% saying they would donate mainly for friends and relatives. Only 10.2% people did not want to donate blood. Because age, education, source of information, past contribution, and type of contribution were all found to be strongly correlated with willingness to donate, these aspects can be investigated further to increase the number of contributors.
Conclusion
Males and those with a higher education were the most likely to donate blood. Donors saw blood donation as a humanitarian cause and felt it provided them with higher moral gratification than non-donors. Non-donors were more likely than donors to believe that blood donation causes weakness/anaemia and is damaging to their health. In comparison to non-donors, the majority of donors were willing to be voluntary donors in the future. Non-donors had not given blood since they had not been solicited. As a result, it can be stated that suitable incentive and enough awareness through campaigns can be used to attract more contributors for voluntary giving. The concept of voluntary blood donation must be heavily pushed in order to attract regular, unpaid donors.
References
- www.who.int/bloodsafety/factsheet.
- https://www.who.int/health-topics/blood-transfusion- safety#tab=tab_1
- http://www.naco.gov.in/sites/default/files/National%20 Blood%20Policy_0.pdf
- Sameeya FS, Reddy MR. Factors influencing blood donation among the workers of a tertiary care hospital, Chitradurga: A comparative study. Int J Community Med Public Health 2018;5:1004-1009.
- Manikandan S, Srikumar R, Ruvanthik PN. A study on knowledge, attitude and practice on blood donation among health professional students in Chennai, Tamil Nadu, South India. Int J Scientific Res Publ. 2013;3:1-4.
- Dubey A, Sonker A, Chaurasia R, Chaudhary R. Knowledge, attitude and beliefs of people in North India regarding blood donation. Blood Transfus. 2014;12:21-27.
- Anand N, Inban P. A study on knowledge, attitude and practice regarding blood donation in an urban community, Chennai. Public Health Rev Int J Public Health Res. 2018;5:35-44.
- Durugu S, Ganta SR. A study of knowledge, attitudes and practices of voluntary blood donation among relatives of patients admitted to a tertiary care hospital in north coastal Andhra Pradesh, India. Int J Community Med Public Health 2016;3:2237-2243.
- Verma S, Sharma RK, Sharma M, Pugazhendi S. Voluntary blood donation: Attitude and practice among indian adults. J Community Med Health Educ. 2016;6:1-6.
- Chandi DH, Patil P, Damke S, Basak S, Ashok R. Bacteriologic antibiography outline of isolates from blood culture at tertiary center. J Pure Appl Microbiol. 2020;14:2801-2806.
- Gupta V, Vagha SJ. Pre-Donation blood donor deferral: A perspective in rural population of India. Vox Sanguinis. 2010;99:145-146.
- Gupta V, Vagha SJ, Meshram N. Social marketing of voluntary blood donation in rural setup of India. Vox Sanguinis. 2010;99.
- Manish B, Amit P, Feroz A, Mohan P, Vivek K, Pankaj S, et al. Knowledge regarding brain death and organ donation laws among medical students. Transplantation. 2018;102:S812.
- Manish B, Mohan P, Goswami J, Vivek K, Trivedi HL, Pankaj S. Awareness and beliefs towards organ donation in chronic kidney disease patients: A single center experience. Transplantation. 2017;101: S102.
- Cristiana A, Abbas KM, Abbasi M, Abbasifard M, Abbasi- Kangevari M, Abbastabar H, et al. Five insights from the global burden of disease study 2019. Lancet. 2020;396:1135-1159.
- Cristiana A, Abbas KM, Abbasi M, Abbasifard M, Abbasi- Kangevari M, Abbastabar H, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396:1204-1222.
- Lozano R, Fullman N, Mumford JE, Knight M, Barthelemy CM, Abbafati C, et al. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: A systematic analysis for the global burden of disease study 2019. Lancet. 2020;396:1250-1284.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.