Awareness of Post-Surgical Adhesions among Gynecological Surgeons: Focus on the Surgical Management of Endometriosis
2 Hospital Universitario Infanta Sofía, San Sebastián de Los Reyes, Madrid, Spain
3 Department of Obstetrics and Gynecology, VU University Medical Centre, Amsterdam, Netherlands
4 Human Development and Health, Faculty of Medicine, University of Southampton, and Complete Fertility Centre, Southampton, United Kingdom
5 Centre Hospitalier Régional Universitaire de Lille, France
6 Department of Public Health, University “Federico II” of Naples, Italy
7 University Hospital Gasthuisberg, Katholieke Universiteit, Leuven, Belgium
8 Clinic of Gynecology, Private Hospital Mølholm, Vejle, Denmark
9 Division of Infertility and Reproductive Endocrinology, Poznan University of Medical Sciences, Poznan, Poland
10 Department of Obstetrics and Gynecology, University Clinic Heidelberg, Germany
Citation: De Wilde RL, et al. Awareness of Post-Surgical Adhesions among Gynaecological Surgeons: Focus on the Surgical Management of Endometriosis. Ann Med Health Sci Res. 2017; 7: 13-17
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objective: Postoperative adhesions occur in 80% of cases of gynecological surgery. Therefore evidence-based recommendations have been made to improve surgeons´ knowledge of postoperative adhesion formation and preventive strategies. The objective of this survey was to assess the perceptions and practice of international gynecological surgeons on adhesions following endometriosis surgery. Materials and Methods: Data capture was conducted via online survey. The questionnaire was accessible worldwide during 2 weeks through the Society of Endometriosis and Uterine Disorders (SEUD) website. The qualitative variables were described as number and percent of the different response modalities, comparing European participants (n= 35) within the whole sample of surgeons (n= 65) vs non-European participants (n= 30). Results: 97% of Europeans and 63% of non-European surgeons recognize adhesion prevention as useful to reduce chronic postoperative pain and to avoid complications related to adhesions. To minimize adhesions, good surgical technique was considered relevant to almost all responders, also the use of anti-adhesive barriers or solutions (77% Europeans vs 57% non-European). 20% of all responders do not provide their patients with information about the risks of adhesion formation, related long-term complications or preventive treatment options. Conclusion: Despite a substantial awareness, disparities in daily practice of gynecological surgeons around the world facing the problem of adhesion formation in surgical endometriosis management exist. In order to improve adherence to anti-adhesion strategies in endometriosis surgery, more scientific evidence is needed. National and international scientific societies can play an important role to initiate research; also it might be helpful to call for more communication in this field.
Keywords
Surgery-induced adhesions; Gynecological surgery; Awareness; Prevention; Endometriosis
Introduction
Postoperative adhesions, bands of connective tissue that join two normally separate anatomical structures, have become one of the commonest sequelae of 75% to 93% of gynecological surgeries, leading to chronic pain, infertility or bowel obstruction, [1-3]. Secondary adhesions due to endometriosis could affect fertility and pregnancy rates through anatomical distorsion or internal reproductive organs [4]. or could produce small bowel obstruction. [3]. Since 40% to 60% of surgeons were not aware of the consequences of adhesion for their clinical practice and women’s life, [5] a first consensus position was published in 2007 by the European Society of Gynecological Endoscopy (ESGE) with the aim to provide evidence-based recommendations to reduce postsurgical adhesions in gynecological surgery.[3]. which allowed an improvement in the European surgeons’ knowledge and antiadhesion strategies, as demonstrated in a subsequent survey performed in 2014. [6]. In that survey 70% of respondents thought that endometriosis surgery, myomectomy, adhesiolysis, and adnexal surgery are the most likely to be associated with adhesions, but only 60% reported to know the surgical techniques recommended for adhesion prevention; and few (38.4%) used antiadhesion agents regularly, because they did not consider these agents as an important measure in adhesion prevention. [6]. Based on this findings, the Society of Endometriosis and Uterine Disorders (SEUD), an international scientific network of experts in women’s and reproductive health, performed the present survey with the aim to assess the perceptions and practice of international gynecological surgeons on adhesions following endometriosis surgery.
Materials and Methods
This was an international online survey conducted among gynecological surgeons, who were recruited through the SEUD website (http://seud.org/about-the-society-of-endometriosisand-uterine-disorders/). This web-site is a platform of information to promote medical education about disease awareness, pathogenesis, risk factors, diagnosis and treatments of diseases that negatively affect women’s health and fertility. The survey was accessible during 2 weeks, from 5th to 22nd April 2014, to surgeons who voluntarily filled up a 12-items questionnaire (Appendix 1). Questions were related to the impact of adhesions on endometriosis and its management, factors associated with adhesion prevention in endometriosis surgery, information of patients and patients consent, prevention of adhesions during surgical management of endometriosis, and the role of the anti-adhesion agents during laparoscopic surgery of endometriosis.
It was an anonymous survey; surgeons all around the world, both members and non-members of the SEUD were allowed to access it, and there was no financial incentive for participants.
Questionnaires were provided with a qualitative 4-point-scale to answer each question: strongly applicable, undetermined, and slightly or not applicable. Every participant was allowed to answer the questionnaire only once. Data were analyzed using SAS software version 9.4. The qualitative variables were described as number and percent of the different response modalities, comparing European surgeons (ES) within the whole sample of surgeons (WSS) vs. Non-European Surgeons (NES). The numbers of missing data were also included.
Results
Sixty-five gynecological surgeons participated [Table 1], most of them Europeans (35/65); mainly working in university hospitals (63%), with a median of 42 beds in their departments. The main countries represented were France (16.9%), Spain (13.8%), Brazil (7.7%), Russia (6.2%) and South Korea (4.6%). During the 6 months prior to the survey, comparable numbers of laparoscopies and laparotomies were performed by each surgeon. The mean numbers of interventions for endometriosis reported during the previous 5 years were 307 for WSS (mean 61/year), mostly by ES, indicting participants had an appropriate level of expertise in the endometriosis field.
| Country | Total | Country | Total | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Europe | Asia | ||||
| Belgium | 2 | 3.1 | Japan | 1 | 1.5 |
| South Korea | 3 | 4.6 | |||
| France | 11 | 16.9 | Other Countries | ||
| Algeria | 1 | 1.5 | |||
| Germany | 2 | 3.1 | Israel | 1 | 1.5 |
| Kenya | 1 | 1.5 | |||
| Greece | 1 | 1.5 | Lebanon | 1 | 1.5 |
| Russia | 4 | 6.2 | |||
| Italy | 3 | 4.6 | South Africa | 2 | 3.1 |
| Turkey | 1 | 1.5 | |||
| Portugal | 3 | 4.6 | Ukraine | 1 | 1.5 |
| United Arab Emirates | 1 | 1.5 | |||
| Spain | 9 | 13.8 | Uzbekistan | 1 | 1.5 |
| USA | 4 | 6.2 | |||
| Sweden | 1 | 1.5 | Central and South America | ||
| Argentina | 1 | 1.5 | |||
| Netherlands | 1 | 1.5 | Brazil | 5 | 7.7 |
| Chile | 1 | 1.5 | |||
| United Kingdom | 2 | 3.1 | Mexico | 1 | 1.5 |
| Total | 35 | 0.538 | Total | 30 | 0.461 |
Table 1: Survey respondents by country of residency.
Regarding the impact of adhesions on endometriosis and its management [Table 2], few NES (20%) think that adhesions can trigger ovarian endometrioma, but 57% of them recognize adhesions as a risk factor for endometrioma recurrence, while 43% of ES agree with both statements. About the negative consequences of endometriosis on fertility, most of participants recognize this effect, but only 63% of NES recognize adhesion prevention as useful to reduce chronic pain and to avoid complications related to adhesions. This medium-low level of knowledge in the pathogenesis of long-term complications related to endometriosis and peritoneal adhesion could affect the surgeon´s pre and intra-operative decision-making process regarding adhesion prevention when facing patients with endometrioma.
| Variables | Strongly applicable | Undetermined | Slightly or  not applicable |
||||||
|---|---|---|---|---|---|---|---|---|---|
| WSS N=65 | NES N=30 |
ES N=35 |
WSS N=65 | NES N=30 |
ES N=35 |
WSS N=65 | NES N=30 |
ES N=35 |
|
| Adhesions can trigger ovarian endometrioma | 21 (32%) |
6 (20%) |
15 (43%) |
8 (12%) |
0 | 8 (23%) |
29 (45%) | 17 (45%) |
12 (34%) |
| Presence of adhesions is a risk factor for endometrioma recurrence | 32 (49%) | 17 (57%) | 15 (43%) |
9 (14%) |
3 (10%) |
6 (17%) |
24 (36%) | 10 (33%) |
14 (40%) |
| Endometriosis may affect fertility by various mechanisms, including disturbance of pelvic anatomy by adhesions | 64 (98%) | 29 (97%) | 35 (100%) |
0 | 0 | 0 | 1 (2%) |
1 (3%) |
0 |
| Adhesion prevention is very important in reducing pain, avoiding complications such as bowel obstruction, and preserving fertility | 53 (81%) | 19 (63%) | 34 (97%) |
2 (3%) |
1 (3%) |
1 (3%) |
0 | 0 | 0 |
WSS: Whole Sample of Surgeons; NES: Non-European surgeons; ES: European Surgeons
Table 2 : Impact of adhesions on the endometriosis and its management.
When asked about their experience with endometriosis patients, and patient counselling [Table 3], it was found that patients with endometriosis and adhesions are an important part of their daily work, both medically (87% NES vs 74% ES), and surgically (90% NES vs. 74% ES). During the patient counselling process, most surgeons provide information regarding adhesion formation, but the majority did not discuss long-term complications of adhesions (73% NES vs. 74% ES), or provide information about prevention options to patients with endometriosis undergoing pelvic surgery (67% NES vs 74% ES). As mentioned before, the lack of up-dated information about the consequences of adhesions between surgeons could also impact the quality of information and care that patients receive by their physicians.
| Variables | Strongly applicable | Undetermined | Slightly or not applicable |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| WSS N=65 | NES N=30 |
ES N=35 |
WSS N=65 | NES N=30 |
ES N=35 |
WSS N=65 | NES N=30 |
ES N=35 |
||
| Patients with endometriosis and adhesions are an important part of my daily medical work besides surgery | 52 (80%) | 26 (87%) |
26 (74%) |
7 (11%) | 3 (10%) | 4 (11%) |
6 (9%) |
1 (3%) | 5 (14%) | |
| Patients with endometriosis and adhesions are important part of my daily surgical work | 53 (82%) | 27 (90%) |
26 (74%) |
6 (9%) | 3 (10%) | 3 (9%) |
6 (9%) |
0 | 6 (17%) |
|
| I provide information on treatment options for adhesions for all patients with endometriosis undergoing pelvic surgery | 46 (71%) | 20 (67%) |
26 (74%) |
8 (12%) | 8 (12%) | 3 (9%) |
11 (17%) | 5 (17%) |
6 (17%) |
|
| I provide information on long-term complications of adhesions | 48 (74%) | 22 (73%) |
26 (74%) |
8 (12%) | 4 (13%) | 4 (11%) |
9 (14%) |
4 (11%) | 5 (14%) |
|
| I provide information about adhesion formation during the consent process | 52 (80%) | 22 (73%) |
30 (86%) |
4 (6%) | 4 (13%) | 0 | 9 (14%) |
4 (11%) |
5 (14%) |
|
WSS: Whole Sample of Surgeons; NES: Non-European Surgeons; ES: European Surgeons
Table 3 : Information of patients and patients’ consent.
When asked about the factors associated with adhesion prevention during surgical management of endometriosis [Table 4], the large majority of respondents have well defined surgical strategies to prevent adhesions, and also consider adhesiolysis as an important preliminary step in the surgical procedures for endometriosis. To minimize adhesions, good surgical technique was considered as relevant for both groups, more than the use of anti-adhesive barriers or solutions (57% NES vs. 77% ES). Here, 60% of NE and 57% of ES reported to use these agents regularly as an adhesion prevention strategy. These results suggest that surgeons relay adhesion prevention on surgical technique more than in anti-adhesion substances, reflecting what ESGE and other international guidelines emphasize, but also could be related with a low availability of the substances in some settings.
| Variables | Strongly -applicable | Undetermined | Slightly or not applicable |
||||||
|---|---|---|---|---|---|---|---|---|---|
| WSS N=65 |
NES N=30 |
ES N=35 |
WSS N=65 | NES N=30 |
ES N=35 |
WSS N=65 | NES N=30 |
ES N=35 |
|
| Adhesion prevention is one of the goals of laparoscopic surgery for endometriosis | 58 (89%) | 29 (97%) | 29 (83%) | 5 (8%) |
1 (3%) |
4 (11%) | 2 (3%) |
0 | 2 (6%) |
| Adhesiolysis is considered an important preliminary step in the surgical procedures for endometriosis | 64 (99%) | 30 (100%) |
34 (97%) | 1 (1%) |
0 | 1 (3%) |
0 | 0 | 0 |
| Good surgical technique is important to minimizing adhesions | 64 (99%) | 30 (100%) |
34 (97%) | 1 (1%) |
0 | 1 (3%) |
0 | 0 | 0 |
| Anti-adhesive barriers or solutions are important in adhesion reduction and prevention | 44 (68%) | 17 (57%) | 27 (77%) | 13 (20%) | 10 (33%) | 3 (9%) |
8 (12%) |
3 (10%) |
5 (14%) |
| I regularly (at least two times in the last month) use agents for adhesion reduction and prevention intra-operatively | 38 (59%) | 18 (60%) |
20 (57%) | 10 (15%) | 0 | 10 (33%) | 17 (26%) | 12 (40%) | 5 (14%) |
WSS: Whole Sample of Surgeons; NES: Non-European Surgeons; ES: European Surgeons
Table 4: Prevention of adhesions during surgical management of endometriosis.
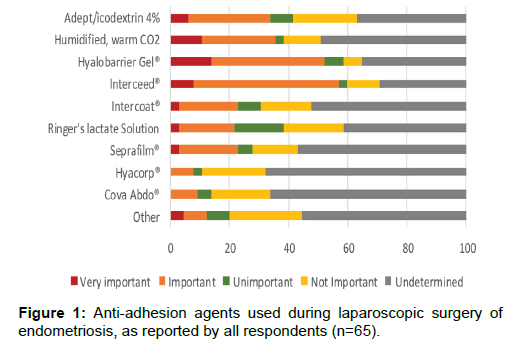
Specifically, anti-adhesion agents during laparoscopic surgery [Figure 1] are used on a regular basis by most of all responders in case of diagnosis of adhesions during endometriosis surgery. Different agents were mentioned to be used, or to be considered to use, such as oxidized regenerated cellulose (Interceed®) hyaluronic acid (Hyalobarrier gel®) and 4% icodextrin (Adept®); and 20% of surgeons use Ringer´s lactate as an adhesion prophylactic agent. In addition, environmental peritoneal conditioning technique, which includes the use of humidified CO2 and physiologic temperature during laparoscopy, was considered useful in adhesion reduction and prevention by one third of AS. Here, participants reflect the wide option of antiadhesion agents available and used; but in accordance to the medium-frequency of use yet discussed, participants prefer to use them as a secondary prevention measure after adhesiolysis of preexisting adhesions.
Discussion
Endometriosis and its associated adhesions adversely impact on women’s reproductive health and quality of life, and is a significant health care burden for patients, clinicians and health care providers. The adverse impact of endometriosis on fertility and the optimal surgical options in their treatment are recently highlighted as two of the top ten concerns in endometriosis by health care practitioners and the public. [7]. In addition, there is inconclusive evidence about the long-term effectiveness of prevention agents. [8].
Many scientific communities involved with women’s health are also concerned and they performed surveys to assess the awareness of gynecological surgeons regarding postsurgical adhesions after surgical management of endometriosis. A previous survey, conducted by ESGE among 253 gynecological surgeons from European countries [5], reported that the knowledge of recommended surgical techniques and preventive measures to reduce adhesions were not widely spread; although the responders showed a good knowledge of the risk factors. In the present survey, conducted with the assistance of SEUD, it was demonstrated that even in gynecological surgeons with expertise in the field of endometriosis surgery, discrepancies in the respondent’s opinion regarding the impact of adhesions on endometriosis and its management exist.
Regarding the impact of adhesions and endometriosis, the associated impairment of fertility is well recognized by all participants. In contrast, the role of adhesions in ovarian endometrioma occurrence and recurrence is not recognized by more than half of WSS, especially by NES. Different studies have reported that ovarian endometrioma reoccurs in 9.6 to 80% of cases after complete laparoscopic resection. [9,10]. Presence of adhesions, previous pelvic surgery, fulguration, and higher Ca 125 levels, seem to be risk factors for endometrioma recurrence. [10,11]. Interestingly, small endometrioma (< 3 cm) could be associated with a higher degree of pelvic adhesions. [10].
In contrast to the 40% of ESGE respondents, we found that most of WSS recognize the importance of adhesion prevention to reduce long term complications related to abdominal and gynecological surgery. As well, WSS reported to follow the international recommendations for surgical management of endometriosis [12,13] that is using laparoscopic approach, adhesiolysis and good surgical technique. Thus, patients with endometriosis are a high risk for pre and postsurgical adhesions, being laparotomy more adhesiogenic than laparoscopy (1.23 ± 0.22, p<0.000; 95% IC 1.02-1.99), [14]. and that laparoscopic surgery is associated with higher pregnancy rates (RR 1.44, 95% CI: 1.24-1.68, p<0.01), and live birth rates (RR 1.52, 95% CI: 1.26-1.84, p<0.01). [15]. This awareness improvement could be the result of new evidence and educational activities that promotes the application of good surgical technique and complementary measurements for patients at high risk of adhesions. Therefore more patients will benefit from practices that reduce their own risk of peritoneal adhesions after endometriosis surgery.
Based on the safety and reported efficacy compared to notreatment to reduce surgical adhesions, [16]. anti-adhesive barriers and the use of peritoneal conditioning have been proposed in the recommendations as complementary measures. Antiadhesion agents were reported to be important, or to be used in daily practice by our responders in similar way to what was reported by ESGE participants (59% SEUD vs. 60.5% ESGE). [5]. However, we found a decrease in the frequency of use of peritoneal conditioning compared to ESGE survey (34% SEUD vs. 55.3% ESGE). [6]. This limited use of complementary and effective measures to prevent postsurgical adhesions could be explained by the non-availability of these technologies in low income settings or by their high cost, when available. Meanwhile, in some settings the woman reproductive health or the burden of postsurgical adhesions will not be improved, what is contrary to the objectives of the clinical guidelines?
Despite the interest of gynecological surgeons in post-surgical adhesions and their preventive measures facing one of the major medical problems in gynecology, The majority of surgeons yet does not provide their patients with information about the risks of adhesion formation, long-term complications related with or preventive treatment options (73% NES vs. 80% ES). This frequency is higher than was former reported by surgeons in the Netherlands (10% to 41%), and the United Kingdom (23% to 48%). [1]. Incorporating adhesion prevention as a routine in the pre-operative counselling procedure could thus help to prevent medical malpractice lawsuits when complications occur. [1].
We recognize that the scope of the present survey was limited by the low number of respondents, especially NES. In consequence, the composition of our groups did not constitute completely representative sample of gynecologists that take care of women with endometriosis. But, all together these results reflect again that the knowledge, perceptions and practices of surgeons regarding adhesions should be improved in order to increase the benefits of adhesion prevention after endometriosis surgical management, especially on women´s reproductive health.
Conclusion
The results of this survey highlight the disparity in the opinion of gynecological surgeons around the world, on the management of adhesions in the context of endometriosis. It is prudent that surgeons remain up to date with evidence in order to provide women with adequate information on the impact of endometriosis and adhesions on their reproductive health. National and international, scientific and funding bodies should prioritize research in the area of endometriosis, particularly around its detrimental impact on women’s reproductive health and ways to optimize surgical management with a focus on adhesion formation, reformation and prevention.
Acknowledgements
The authors thank all responders of the survey for their important opinions, and Laurence Saya, MD, Altius Pharma CS, Paris, France, for the help in medical writing.
Author Disclosure Statement
All members of the ANGEL group received travel reimbursement fees to attend the author´s meeting to analyze and discuss the survey´s results.
Funding
Nordic Pharma sponsored the survey´s platform and the transcription of the author’s meeting for the preparation of this manuscript.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the final version to be published.
REFERENCES
- Hirschelmann A, Wallwiener CW, Wallwiener M, Weyhe D, Tchartchian G, Hackethal A, et al. Is patient education about adhesions a requirement in abdominopelvic surgery? Geburtshilfe Frauenheilkd. 2012; 72:299-304.
- De Wilde RL, Bakkum EA, Brölmann H, Crowes A, Konninckx P, Korell M, et al. Consensus recommendations on adhesions (version 2014) for the ESGE Adhesions Research Working Group (European Society for Gynecological Endoscopy): an expert opinion. Arch Gynecol Obstet. 2014; 290:581-582.
- Wolthuis AM, Meuleman C, Tomassetti C, D’Hooghe T, De Buck van Overstraeten A, D’Hoore A. Bowel endometriosis: Colorectal surgeon’s perspective in a multidisciplinary surgical team. WJG. 2014; 20:15616-15623.
- Ghezzi F, Raio L, Cromi A, Duwe DG, Beretta P, Buttarelli M, et al. "Kissing ovaries": A sonographic sign of moderate to severe endometriosis. Fertil Steril. 2005; 83:143-147.
- De Wilde RL, Trew G. Postoperative abdominal adhesions and their prevention in gynaecological surgery. Part 2. Gynecol Surg. 2007; 4:243-253.
- Wallwiener M, Koninckx P, Hackethal I, Brolmann H, Lundorff P, Mara M, et al. A European survey on awareness of post-surgical adhesions among gynecological surgeons. Gynecol Surg. 2014; 11:105-112.
- Horne AW, Saunders PTK, Abokhrais IM, Hogg L. Endometriosis priority setting partnership steering Group (appendix). Top ten endometriosis research priorities in the UK and Ireland. Lancet. 2017; 389:2191-2192.
- Lower AM, Hawthorn RJ, Ellis H. The impact of adhesions on hospital readmissions over ten years after 8849 open gynaecological operations: an assessment from the Surgical and Clinical Adhesions Research Study. BJOG 2000; 107:855-862.
- Porpora MG, Pallante D, Ferro A. Pain and ovarian endometrioma recurrence after laparoscopic treatment of endometriosis: A long-term prospective study. Fertil Steril. 2010; 93:716-721.
- Exacoustos C, Zupi E, Amadio A. Recurrence of endometriomas after laparoscopic removal: Sonographic and clinical follow-up and indication for second surgery. Minim Invasive Gynecol. 2006; 13:281-288.
- Guzel AI, Topcu HO, Ekilinc S. Recurrence factors in women underwent laparoscopic surgery for endometrioma. Minerva Chir. 2014; 69:277-2782.
- De Wilde RL, Brölmann H, Koninckx PR. Prevention of adhesions in gynaecological surgery: The 2012 European field guideline. The Anti-Adhesions in Gynecology Expert Panel (ANGEL). Gynecol Surg. 2012; 9:365–368.
- Diamond MP, Wexner, SD, Di Zereg GS. Adhesion prevention and reduction: Current status and future recommendations of a multinational interdisciplinary Consensus Conference. Surgical Innovation: 2012, 17:183-188.
- Shehata F, Zare A. Shalom-Paz E, Tulandi T. Predictors of intra-abdominal adhesions. Gynecol Surg. 2011; 8:405–408.
- Jin X, Ruiz Beguerie J. Laparoscopic surgery for subfertility related to endometriosis: a meta-analysis. Taiwan J Obstet Gynecol. 2014; 53:303-308.
- Ahmad G, Duffy JM, Farquhar C, Vail A, Vandekerckhove P, Watson A, et al. Barrier agents for adhesion prevention after gynaecological surgery. Cochrane Database Syst Rev. 2008; 2:CD000475.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.