Awareness, Practices and Treatment Seeking Behavior of Type 2 Diabetes Mellitus Patients in Delhi
2 Department of Community Medicine, Maulana Azad Medical College,Reproductive Health and Nutrition Division, Indian Council of Medical Research, New Delhi, India, Email: drnaveenta@gmail.com
Citation: Kishore J, Kohli C, Gupta N, Kumar N, Sharma P. Awareness, practices and treatment seeking behavior of type 2 diabetes mellitus patients in Delhi. Ann Med Health Sci Res 2015;5:266-73.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Type 2 diabetes mellitus is a multisystem disorder that is associated with number of complications. Patient’s awareness and practices are crucial components in reducing the burden of diseases and its complications. Aim: To assess patient’s knowledge about their disease and its complications, practices, treatment seeking behavior and average expenditure incurred by its management. Subjects and Methods: A community based cross‑sectional study was conducted in rural and urban slum areas of Delhi selecting a total of 98 diabetic patients diagnosed during the two community surveys and interviewed using pretested and predesigned questionnaire. Data were analyzed using SPSS software, version 17 (Chicago II, USA). Chi‑square, fisher or Mann–Whitney tests were used for test of significance and considered statistically significant at P < 0.05. Results: Of 98 participants, 31.6% (31/98) were from urban slum area, and 68.4% (67/98) were from the rural area. In both urban and rural areas, majority were Hindu, married, literate and unemployed. Significantly less subjects (61.3%, 19/31) of urban slum area than of rural area (85.1%, 57/67) could name at least one complication of DM (P < 0.01, odds ratio [OR] =3.6, 95% confidence interval [CI] =1.3–9.6). Majority of participants in both urban slum and rural area have knowledge about at least one component of management but significantly lesser in urban (83.9%, 26/31) than rural area (97.0%, 65/67) were reported (P = 0.02, OR = 6.2, 95% CI = 1.1–34.2). Significantly more subjects (29.0%, 9/31) in urban slum area than rural areas (7.5%, 5/67) reported that they were not taking any treatment for DM (P < 0.01, OR = 0.2, 95% CI = 0.1–0.6). In urban area, 32.2% (10/31) patients told that it is a burden on their family while in rural area 44.7% (30/67) of the patients told that they have to squeeze money from the family expenditure to afford drugs. Conclusion: Patients need to be made aware of the asymptomatic phase of DM and its long‑term complications. At the same time, efforts should be made to sensitize them about the importance of taking regular treatment and management.
Keywords
Diabetic mellitus type 2, Economic impact, Knowledge, Practices
Introduction
Diabetes mellitus (DM) is a chronic disorder characterized by elevated blood sugar levels that occur when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces. The first one is called as type 1 diabetes mellitus (T1DM) and later one is called as type 2 diabetes mellitus (T2DM).[1] The prevalence of diabetes is more heavily due to T2DM, and its adverse health effects have risen more rapidly in South Asian region than in any other region of the world.[2] According to the International Diabetes Federation, currently 39.5 million people in India have prediabetes, and of them seven million will develop diabetes every year. The number of people with diabetes in India is expected to increase from 51 million in 2010 to 87 million in 2030.[3] Studies have documented 2.6% and 1.5% prevalence of diabetes among men and women in the urban areas while in rural areas had a lower prevalence: 1.8% and 1.3% respectively.[4] By 2010, the average age-adjusted prevalence of diabetes in India was 8%, higher than that in most European countries.[5] DM is associated with a large variety of complications and a greater risk of all manifestations of atherosclerosis.[6]
Diabetes is a silent disease-many sufferers became aware that they have diabetes only when they develop one of its life-threatening complications. Once diabetes develops, it is a costly disease to manage because of its chronic nature and severity of complications.[7] Over 70% of diabetes-related cost is attributed to its complications, particularly for macro-vascular diseases that most commonly occur in type 2 diabetics.[8]
It is known that adequate control of diabetes is essential if complications are to be reduced.[9] There is evidence available that knowledge about DM and its complications has a positive association with attitude and practices for self-care and glycemic control among diabetics.[10,11]
If patients are to contribute to the effective control of their diabetes, their awareness and practices can assist in reducing the incidence of its complications. The interaction between demography and awareness about DM has already been emphasized by some authors in other countries. Similarly, the rural-urban difference could be present.[12]
This article discusses the results of a study conducted among people with T2DM in rural and urban areas of Delhi with an objective to assess their knowledge about DM and its complications, practices, treatment seeking behavior and average expenditure incurred on its management among those who are suffering.
Subjects and Methods
Study design, setting and participants
In this cross-sectional study, 98 adult patients with T2DM were included. These patients were detected from the screening survey conducted 4 months back on 200 adults in urban area and 1005 adults in rural area selected by systematic random sampling[13] from approximately 22,000 population of following areas; urban areas: An urban slum[14] Balmiki Basti and a resettlement colony Vikram Nagar and rural area: Barwala and adjoining Pooth Khurd village. This sample was calculated on the basis of previous recorded prevalence of diabetes in a rural population in multicentric study as 3.1% and for urban 7.3%.[15] The two areas were selected by convenience sampling. The study was conducted over a period of 3 months from July 2012 to September 2012 and four months after the screening survey.
Methodology
All subjects were diagnosed during a screening survey by fasting and postprandial blood glucose tests in both rural and urban areas described elsewhere.[13] The patients were traced after 4 months in those two areas. Seven patients in the urban area could not be traced even after three visits. Finally, 31 DM patients in the urban area and 67 in the rural area were interviewed after taking informed consent and analyzed.
Study tool
A pretested, predesigned, semi-structured questionnaire schedule in local language consisting of items on the demographic profile including age, sex, religion, marital status, education, occupation, etc., was used. Questionnaire consisted of items to assess their knowledge (cause, types, symptoms and complications), practices for management and prevention of complications (exercise and dietary modifications) and health seeking behavior about DM and its complications (drugs, compliance to treatment, reasons for not taking treatment, complications of management etc.) Questionnaire was pilot tested in a different setting among adult DM patients for assessing its feasibility and reliability. Suitable modifications were done afterward. Cronbach’s alpha that is a coefficient of internal consistency was calculated which came out to be 0.82. Opinion of experts on each questionnaire item was obtained, and all graded excellent in its construct and meaning. Data were also collected about the average out of pocket expenditure incurred on DM treatment. Average time duration of each interview was approximately 10-15 minutes.
Inclusion and exclusion criteria
All adult patients that is, aged equal to or more than 18 years with DM diagnosed through screening survey were included. No patient refused to participate, and none was seriously ill who could not complete the interview.
Statistical analysis
Data were analyzed using SPSS software, version 17 (Chicago II, USA). Results are presented in averages and proportions. Difference in proportions between groups was assessed using Chi-square or fisher test and means by Mann–Whitney test for nonnormal distribution. It was accepted for statistical significance when error was <5%.
Ethical issues
All patients were explained the purpose of the study and confidentiality was assured. A written informed consent was taken from each patient before collecting data. The study was approved by the University’s Institutional Ethical Committee.
Results
Demographic profile of participants
Of 98 participants, 31.6% (31/98) were from the urban area, and 68.4% (67/98) were from the rural area. In urban area, there were 38.7% (12/31) males and 61.3% (19/31) females while in rural area there were 41.8% (28/67) males and 58.2% (39/67) females who participated in the study. In both urban and rural areas, majority were Hindu (74.2%; 23/31 and 97%; 65/67), married (83.9%; 26/31 and 92.5%; 62/67), literate (77.4%; 24/31 and 80.6%; 54/67) and unemployed (71%; 22/31 and 61.2%; 41/67). Mean age (standard division) in the urban area was 49.58 (12.07) years and in a rural area was 51.18 (11.47) years.Average monthly family income and per capita income were significantly higher in urban areas than in rural areas. Details of socio demographic profile are given in Table 1.
| Characteristic | Urban n=31 (%) | Rural n=67 (%) | Total n=98 (%) | OR, 95% CI | P | |||
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Male | 12 | (38.7) | 28 | (41.8) | 40 | (40.8) | 1.1, 0.5-2.2 | 0.77 |
| Female | 19 | (61.3) | 39 | (58.2) | 58 | (59.2) | ||
| Religion | ||||||||
| Hindu | 23 | (74.2) | 65 (97) | 88 | (89.8) | 11.3, 2.2-57.2 | 0.01 | |
| Muslim | 1 | (3.2) | 1 | (1.5) | 2 | (2.0) | ||
| Sikh | 7 (22.6) | 1 | (1.5) | 8 | (8.2) | |||
| Education | ||||||||
| Illiterate | 7 (22.6) | 13 | (19.4) | 20 | (20.4) | 0.8, 0.3-2.3 | 0.71 | |
| Literate | 24 | (77.4) | 54 | (80.6) | 78 | (79.6) | ||
| Occupation | 0.6, 0.3-1.6 | 0.34 | ||||||
| Unemployed | 22 | (71.0) | 41 | (61.2) | 63 | (64.3) | ||
| Employed | 9 (29.0) | 26 | (38.8) | 35 | (35.7) | |||
| Marital status | ||||||||
| Married | 26 | (83.9) | 62 | (92.5) | 88 | (89.8) | 2.38, 1.6-8.9 | 0.03 |
| Unmarried | 3 | (9.7) | 0 | (0.0) | 3 | (3.1) | ||
| Widow/separated | 2 | (6.4) | 5 | (7.5) | 7 | (7.1) | ||
| Income (monthly in rupee)* | ||||||||
| Total family, mean (SD) | 22,419.35 (19,621.03) | 16,295.52 (12,431.25) | 18,232.65 (15,244.98) | 0.07-0.08 | 0.08 | |||
| Per capita, mean (SD) | 4412.22 (3474.23) | 2642.29 (2081.55) | 3202.16 (2713.97) | 0.03-0.04 | 0.01 | |||
Table 1: Demographic characteristics of study subjects
Knowledge of type 2 diabetes mellitus and its complications
When participants were asked about what happens to blood glucose levels in DM, 74.2% (23/31) participants in urban area and 49.3% (33/67) in rural area responded correctly that glucose levels increases in DM that was statistically significant (P = 0.02, odds ratio [OR] =0.3, 95% confidence interval [CI] =0.1–0.9). When they were asked if they know about types of DM, 22.6% (7/31) in urban slum area and 32.8% (22/67) in rural area answered positively but it was not statistically significant (P = 0.3, OR = 1.7, 95% CI = 0.6–4.5). Participants were also asked about the cause of DM in which only 19.4% (6/31) in urban slum area and 11.9% (8/67) in rural area knew that it is because of decreased availability of insulin in the body but this difference was not significant (P = 0.32, OR = 0.6, 95% CI = 0.2–1.8). 61.3% (19/31) patients in urban area and only 1.5% (1/67) in rural area reported that they knew about the genetic inheritance of DM, but 38.7% (12/31) in urban slum area and 98.5% (66/67) in rural area had no knowledge about the same. This difference in knowledge was statistically significant (P < 0.01, OR = 0.01, 95% CI = 0.01–0.08 ).
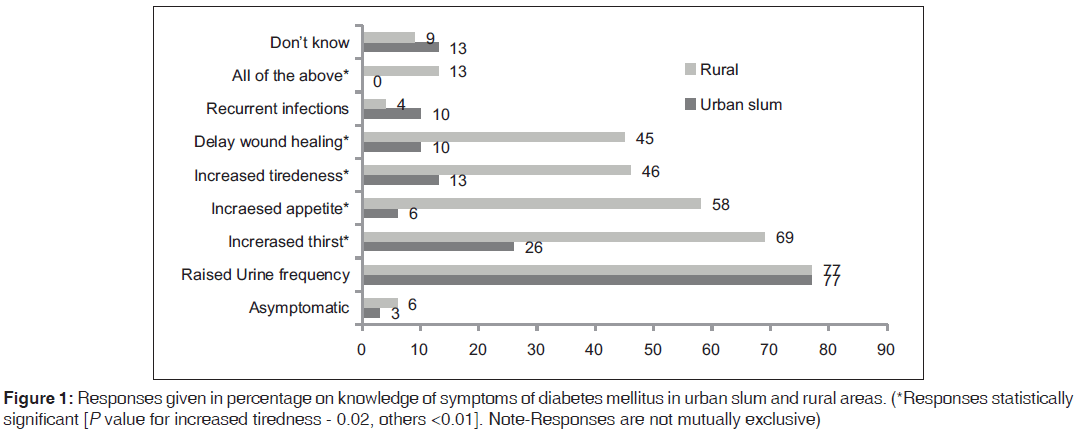
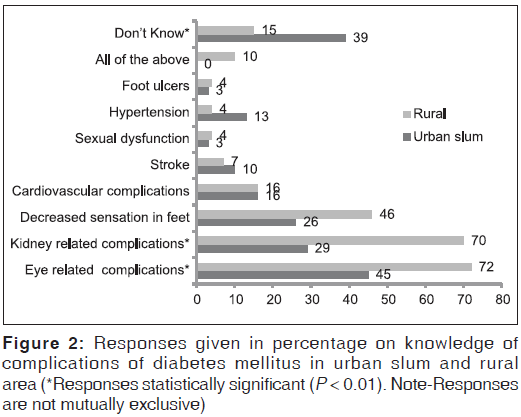
When asked about their awareness on symptoms of DM, 87.1% (27/31) patients in urban slum area and 91.0% (61/67) in rural area were able to name at least one symptom of DM but this difference was not significant (P = 0.54, OR = 1.5, 95% CI = 0.4–5.8). The responses that were given by participants are shown in Figure 1 But when asked about their awareness on complications of DM, then 61.3% (19/31) in urban area and 85.1% (57/67) in rural area could name at least one complications of DM and this difference was statistically significant (P < 0.01, OR = 3.6, 95% CI = 1.3–9.6). Figure 2 shows responses given by respondents on complications of DM.
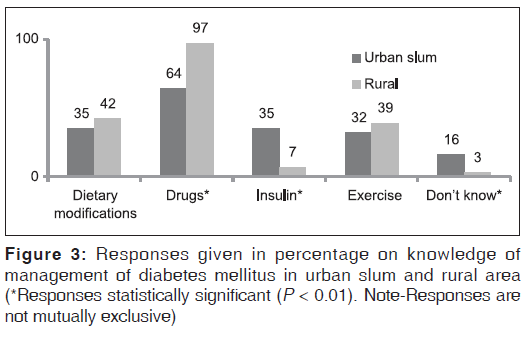
The majority of participants in both urban slum 83.9% (26/31) and rural area 97.0% (65/67) were reported to have knowledge about at least one component of DM management which was statistically significant (P = 0.01, OR = 6.2, 95% CI = 1.1–34.2) as shown in Figure 3. 67.7% (21/31) in urban slum area and 70.1% (47/67) in rural area knew that lifestyle modifications are important for a patient with DM but the difference was not significant (P = 0.81, OR = 0.3, 95% CI = 0.1–0.8). Surprisingly, the rural population showed more health literacy about T2DM.
About 51.6% (16/31) in urban slum area and 71.6% (48/67) in rural area knew that a DM patient should get his/her eye checked by doctor which was not significant (P = 0.05, OR = 2.7, 95% CI = 1.0–5.7). When asked about awareness on symptoms of hypoglycemia when a patient is on treatment of DM, then patients in urban slum area have significantly higher knowledge where 58.1% (18/31) patients as compared to 35.8% (24/67) in the rural area could tell at least one symptom of hypoglycemia (P = 0.03, OR = 0.4, 95% CI = 0.2–0.9). Only 35.5% (11/31) in urban and 20.9% (14/67) in the rural area knew that symptoms of hypoglycemia can be corrected by taking items like sugar candies. 64.5% (20/31) patients in urban area and 50.7% (34/67) in rural area had no knowledge about the practices a DM patient should adopt like care for their feet, carrying candies when they go out, regular eye check-up and blood sugar monitoring etc., (P = 0.20, OR = 0.6, 95% CI = 0.2–1.4). Similarly, 54.8% (17/31) and 80.6% (54/67) patients in urban and rural areas respectively had no knowledge about forbidden practices that a diabetic patient should not do like wearing tight shoes, skipping meals, taking alcohol etc., which was statistically significant (P < 0.01, OR = 3.4, 95% CI = 1.3–8.7 ). 61.3% (19/31) and 79.1% (53/67) in urban slum and rural area, respectively, had no knowledge about recommended diabetes foot care practices like selecting proper footwear, washing and inspecting feet daily for cuts and abrasions, not walking barefoot etc., but difference was not significant (P = 0.06, OR = 2.4, 95% CI = 1.0–6.1)
Practices
About 64.5% (20/31) in urban slum and 61.2% (41/67) in rural area said that they do exercise (P = 0.75, OR = 0.9, 95% CI = 0.3–2.1). Out of those who answered positively, 75.0% (15/20) in urban slum and 68.3% (28/41) in rural area use to do exercise daily. 5.0% (1/20) in urban slum and 2.4% (1/41) in rural area reported once weekly exercise, while 20.0% (4/20) and 29.3% (12/41) used to exercise occasionally in urban slum and rural area, respectively. When asked about their dietary practices, 67.7% (21/31) in urban slum and 83.6% (56/67) in rural area replied positively (P < 0.01, OR = 2.4, 95% CI = 0.9–6.5) about following diabetic diet. Out of those replied positively, more than one-third (8/21; 38.1% urban) and about half (29/56; 51.7% rural) used to follow DM diet always, 61.9% (13/21) in urban and 35.7% (20/56) in rural used to follow it sometimes while 0.0% (0/21) in urban and 12.5% (7/56) in rural followed it occasionally, which was statistically significant (P = 0.02).
Treatment seeking behavior
About 29.0% (9/31) in urban area and 7.5% (5/67) patients in rural area reported that they are not taking any treatment for DM which was statistically significant (P < 0.01, OR = 0.2, 95% CI = 0.1–0.6 ). The majority of patients reported to be taking metformin. One patient each in rural and urban area reported using herbal remedies for DM while one patient in the urban area reported use of homeopathic medicines. None of DM patient reported self-monitoring of glucose at home. When asked about the reasons for not taking any treatment, lack of money, distance of the health facility from residence, dissatisfied with long queues and waiting time and no need of taking treatment were some of the reasons given by the patients as given in Table 2. Out of those who were taking treatment, slightly more than one-third, 36.4% (8/22) in urban slum area and 11.3% (7/62) in rural area said that they used to miss medicines, this difference was significant (P < 0.01, OR = 0.2, 95% CI = 0.1–0.7). Out of those eight patients in urban slum area, 62.5% (5/8) reported that they used to forget taking medicines once a week, and 37.5% (3/8) reported that they forgot occasionally. Similarly out of seven patients in a rural area, 14.3% (1/7) reported that they used to forget taking medicines once a week, and 85.7% (6/7) reported that they do only occasionally.
| Reason for not taking treatment** | Urban (%) | Rural (%) | Total (%) |
|---|---|---|---|
| Lack of money | 4 (44.44) | 2 (40.0) | 6 (42.85) |
| Distance of health facilityfrom residence* | 0 (0.0) | 2 (40.0) | 2 (14.28) |
| Dissatisfied with longqueues and waiting hours | 3 (33.33) | 1 (20.0) | 4 (28.5) |
| No need of treatment | 3 (33.33) | 2 (40.0) | 5 (35.7) |
Table 2: Reasons given by patients for not taking treatment
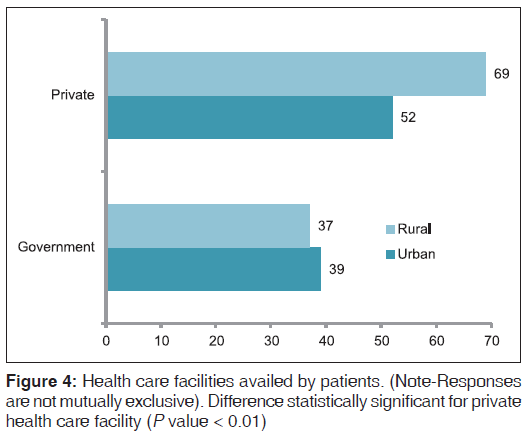
About 9.7% (3/31) and 13.4% (9/67) in urban and rural area respectively reported to have suffered from complications related to DM (P = 0.59, OR = 1.4, 95% CI = 0.4–5.8). 7.5% (5/67) patients in the rural area reported that they had suffered from complications of management of DM. All five patients reported histories of hospital admissions after symptoms of hypoglycemia. When asked about the health facility where they go for treatment, it was found that those who were taking treatment used to follow multiple systems of medicines like allopathic, ayurvedic, homeopathic and home remedies and used to avail both government and private health care facilities [Figure 4].
Expenditure on diabetes management
Patients were asked about out of pocket expenditure on management of DM. The details are shown in Table 3.
| Expenses | Urban area | Rural area | Total | P, 95% CI | ||||
|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | Mean (SD) | ||||
| Drugs (monthly) | 16 | 972.58 | (1354.98) | 53 | 887.99 (1603.20) | 914.74 (1522.57) | 0.27, 0.5-0.6 | |
| Insulin (monthly) | 5 | 209 (535.63) | 2 | 11.19 | (67.88) | 73.98 (316.97) | <0.01, 0.004-0.007 | |
| Travel* | 8 | 73.87 | (150.63) | 42 | 111.04 | (160.09) | 99.29 (157.35) | <0.01, 0.01-0.02 |
| Consultation* | 9 | 254.84 (537.17) | 40 | 233.58 | (224.84) | 240.31 (351.77) | 0.04. 0.07-0.08 | |
| Investigations* | 11 | 829.03 | (2743.01) | 48 | 141.64 | (138.64) | 359.08 (1563.12) | 0.07, 0.1-0.2 |
| Hospitalization related to DM* | 4 | 1338.71 (4459.79) | 1 | 2.99 (24.43) | 425.51 (2557.67) | <0.01, 0.007-0.001 | ||
Table 3: Out of pocket expenditure (in Indian rupee) by the patients on management of DM
From the table data, rough estimate for out of pocket expenditure for 1000 diabetic patients/year for drugs, insulin, travel, consultation, investigations, hospitalization would be Indian National Rupee (INR) 112,008.97 (1789.85$), 9058.77 (144.76$), 4052.65 (64.76$), 9808.57 (156.74$), 14,656.32 (234.2$), 17,367.75 (277.09$) respectively. However, not all patients were taking insulin or hospitalized. Weighted mean came out to be Rs. 433.84 (6.92$)/person in last 3 months or Rs. 1735.36 (27.23$) annually.
Questions were also asked to assess the effect of DM management on the patients and their families. In urban area, 32.2% (10/31) patients told that it is a burden on their family while in rural area 44.8% (30/67) of the patients told that they have to squeeze money from the family expenditure to afford drugs as given by Table 4.
| Effect of DM management on family | Urban (%) | Rural (%) | Total (%) | |
|---|---|---|---|---|
| Squeeze familyexpenditure to buy drugs* | 8 (25.8) | 30 | (44.7) | 38 (38.8) |
| Burden on family budget* | 10 (32.2) | 5 | (7.4) | 15 (15.3) |
| Sacrifice family needs | 6 (19.3) | 6 | (8.9) | 12 (12.2) |
| Not a burden | 7 (22.5) | 26 | (38.8) | 33 (33.6) |
Table 4: Impact of expenditure on DM management on family
Discussion
Knowledge about diabetes mellitus and its complications
The study shows that there is a difference in knowledge among patients in urban slum and rural areas. Study conducted by Pardhan et al. in Badford, UK to compare Caucasian and Asian diabetic patient’s awareness about DM showed that Asians reported a significantly lower perceived knowledge of diabetes, its complications and of the dietary practices required for optimal diabetes management.[16] When the questions were asked to assess their knowledge on pathophysiology of DM like types of DM, causes of DM, it was found that not even half of patients in both urban slum and rural areas knew about these. A similar finding was reported by Shah et al. (2009) among DM patients attending three health centers in Saurashtra, Gujarat where about 46% of patients knew the pathophysiology of diabetes.[17] When asked about the awareness on symptoms of DM, it was found that good percentage that is, 87.1% in urban slum area and 91.0% in rural area were able to name at least one symptom of DM. Most common symptom known to patients in both urban slum and rural areas was increased frequency of urination, and least known symptoms were DM being asymptomatic in the urban area and recurrent infections in the rural area. This corresponds to the findings of a study conducted by Mukhopadhyay et al. (2010) in Kolkata in which frequent urination was most common symptom known to the patients (42.2%) and being asymptomatic was least commonly known (to only 3.1%).[18] The possible reason for higher knowledge about DM among rural patients than urban patients in some aspects may be actual suffering from the symptom or complications by rural patients that leads to their diagnosis. Patients in the urban area might be screened by opportunistic screening for DM while contacting some health facility for some other morbidity. Similarly, when asked about the complications of DM, eye and kidney related complications were most common complications known to patients, again corresponding to the finding of previous study.[18] The majority of patients knew one of the components of management needed for a DM patient. Most commonly known were dietary modifications and drugs as found in the previous study.[18] Another study has found lacunae in knowledge prevailed in drug therapy of diabetes.[17] More than 50% of patients in both areas knew that they should get their eye examination done. In another study conducted by Khandekar et al. (2010) in Oman, knowledge of eye complications of diabetes was excellent in 72.9% of patients.[19] Similar findings were given by Rani et al. in rural districts of Tamil Nadu in which 65.9% patients had the right knowledge of getting an eye examination done despite no knowledge about diabetic retinopathy.[10] For some questions like knowledge about complications and management of DM, knowledge was higher in a rural area as compared to urban slum area. This could be because of higher percentage of literates in the rural area of Delhi as compared to urban slum and resettlement colony. Although 58% of patients in urban slum area could tell at least one symptom of hypoglycemia, but patients in both areas reported low knowledge about how to manage hypoglycemic symptoms. In a study carried out by Upadhyay et al. (2012) in Nepal, only 10.49% of patients knew symptoms, and only 17.28% patients knew how to manage hypoglycemic symptoms in their study.[20] The majority of patients in both areas had no knowledge about overall do’s and don’ts for a diabetic patient. Similarly awareness about foot care was also found to be low. The same findings were reported by Matwa et al. (2003) [21] in Eastern Cape Province concerning poor foot care knowledge and practices and Hasnain and Sheikh (2009)[22] in Lahore where one-third of diabetic patients had poor knowledge about foot care.
Practices
It is a well-established fact that healthy planned eating and regular exercise can delay diabetes and its complications.[23] Although more than 50% patients in both areas said that they used to exercise (30 minutes of brisk walk for at-least 5 days in a week), not all of them used to exercise daily. This is in line with previous studies; one by Raj and Angadi (2010) in Karnataka in which only 40.68% of the respondents reported to exercising regularly.[18,24] Dietary adherence findings are also in line with a previous study in which only 1.85% of the respondents used to follow a diet plan “frequently” at home.[20]
Treatment seeking behavior
The study revealed that 29% of patients in urban and 7.5% of patients in a rural area were not taking any treatment for diabetes. The reason could be higher out of pocket expenditure and higher percentage of patients being unemployed in the urban area. In a study done in rural areas of Tanzania by Baskin (2012) reported 14.9% of the diabetic patients were not taking any treatment at the time of interview. Most common reasons for not taking treatment were lack of money and long waiting hours and queues apart from a distance of health facility from the residence. In the previous study also, cost burden was prime barrier to medications.[25] Poor availability of transport, physical distance to the health facility and the time taken to reach such facilities have been found to influence health-seeking behavior and health service utilization.[26]
In the present study, patients were using different systems of medicine apart from allopathic. This is similar to findings of a study carried out by Mehrotra et al. in Allahabad, India, which showed that 67.8% of patients were using the alternative system of medicine apart from allopathic system of medicine.[27]
Economic impact
The International Diabetes Federation, Diabetes Atlas (2006) reported that public mechanisms for financing health care are nonexistent in most developing countries, hence, health costs typically represent out-of-pocket expenditure.[28] Studies in India, for example, have shown that a low-income family with one adult with diabetes may spend as much as 25% of family income on the care of the patient.[29] Mean direct annual cost for outpatient care for all patients with diabetes was INR 4724/-, those without complication had 18% lower cost.[30] According to Ramachandran (2007), annual expenditure on inpatient care on investigations, physicians fees and medicine were Rs. 6725 (107.29$), on hospitalization was Rs. 5000 (79.77$) and transport was Rs. 300 (4.79$) for diabetes.[31]
The present study also found that patients have to bear a significant out of pocket expenditure on management of diabetes. Expenditure on drugs and hospitalization was higher than travel. For 66.4% of the patients, the cost of DM management was a burden that is consistent with a previous study where almost all patients considered treatment of DM as a cost burden on their families.[25]
Conclusion
Although patients have some knowledge about diabetes symptoms and complications, awareness about their management was lacking. Patients need to be made aware of long-term complications of diabetes on eye, heart, kidney, etc., and precautions that should be taken and that they can be prevented. At the same time, efforts should be made to sensitize them about the importance of taking regular treatment. Public health care facilities should be utilized for easy and affordable availability of drugs so that burden of disease on patient family can be reduced.
Strengths and Limitations
The present study focused upon an important emerging disease DM in India. Strengths of the study are its defined objectives, large sample size, use of validated tool and interpretation of results. Treatment compliance, health seeking behavior and expenditure incurred on management were mainstay of results. Possible limitations are rural study area chosen may not be representative of rural areas in other states in India due to the difference in pace of urbanization and health care facilities available in Delhi and other states.
Multi centric studies should be conducted in future so as to get the results with better external validity. Policy level changes can be undertaken to plan interventions to raise awareness, compliance, better availability of cheaper drugs and comprehensive health education services at the primary health centers.
Acknowledgements
Indian Council of Medical Research funded the project for rural area. For urban area, Dr. Ankur Garg, Dr. Tanu Anand, Dr. Urvi Sharma and Dr. Promod Lali Maulana Azad Medical College and Lok Nayak hospital, New Delhi, supported the project. Authors are grateful to all the study subjects for their contribution.
REFERENCES
- Mohan V, Sandeep S, Deepa R, Shah B, Varghese C.Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res 2007;125:217-30.
- Ghaffar A, Reddy KS, Singhi M. Burden of non-communicable diseases in South Asia. BMJ 2004;328:807-10.
- International Diabetes Federation. IDF Diabetes Atlas. 4th ed. Brussels, Beligium: International Diabetes Federation; 2009.
- Ahuja MM, editor. Epidemiological studies on diabetes mellitus in India. In: Epidemiology of Diabetes in Developing Countries. New Delhi: Interprint; 1979. p. 29-38.
- Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87:4-14.
- Khuwaja AK, Rafique G, White F, Azam SI. Macrovascular complications and their associated factors among persons with type 2 diabetes in Karachi, Pakistan – a multi-center study. J Pak Med Assoc 2004;54:60-6.
- Khuwaja AK. Evidence-based care of type 2 diabetes mellitus: Epidemiology, screening, diagnosis and initial evaluation. J Liaq Univ Med Health Sci 2003;2:63-7.
- Caro JJ, Ward AJ, O’Brien JA. Lifetime costs of complications resulting from type 2 diabetes in the U.S. Diabetes Care 2002;25:476-81.
- Aiello LP, Cahill MT, Wong JS. Systemic considerations in the management of diabetic retinopathy. Am J Ophthalmol 2001;132:760-76.
- Rani PK, Raman R, Subramani S, Perumal G, Kumaramanickavel G, Sharma T. Knowledge of diabetes and diabetic retinopathy among rural populations in India, and the influence of knowledge of diabetic retinopathy on attitude and practice. Rural Remote Health 2008;8:838.
- Abioye-Kuteyi EA, Ojofeitimi EO, Ijadunola KT, Fasanu AO.Assessment of dietary knowledge, practices and control in type 2 diabetes in a Nigerian teaching hospital. Niger J Med 2005;14:58-64.
- Sabri AA, Qayyum MA, Saigol NU, Zafar K, Aslam F. Comparing knowledge of diabetes mellitus among rural and urban diabetics. Mcgill J Med 2007;10:87-9.
- Kishore J, Ray PC, Gupta N. A Feasible Tool of Mass Screening for the Estimation of Prevalence of Type 2 Diabetes Mellitus in the Rural Community of Delhi: Report. ICMR; 2012.].
- Registrar General of India. Census of India; 2011. Available from: http://www.mhupa.gov.in/W_new/Slum_Report_ NBO.pdf. [Last accessed on 2013 Dec21].
- Mohan V, Mathur P, Deepa R, Deepa M, Shukla DK, Menon GR, et al. Urban rural differences in prevalence of self-reported diabetes in India – The WHO-ICMR Indian NCD risk factor surveillance. Diabetes Res Clin Pract 2008;80:159-68.
- Pardhan S, Mahomed I. Knowledge, self-help and socioeconomic factors in South Asian and Caucasian diabetic patients. Eye (Lond) 2004;18:509-13.
- Shah VN, Kamdar PK, Shah N. Assessing the knowledge, attitudes and practice of type 2 diabetes among patients of Saurashtra region, Gujarat. Int J Diabetes Dev Ctries 2009;29:118-22.
- Mukhopadhyay P, Paul B, Das D, Sengupta N, Majumder R. Perceptions and practices of type 2 diabetics: A cross sectional study in a tertiary care hospital in Kolkata. Int J Diabetes Dev Ctries 2010;30:143-9.
- Khandekar R, Harby SA, Harthy HA, Lawatti JA. Knowledge, attitude and practice regarding eye complications and care among Omani persons with diabetes – A cross sectional study. Oman J Ophthalmol 2010;3:60-5.
- Upadhyay D, Izham M, Alurkar V, Mishra P, Palaian S. Evaluation of knowledge, attitude and practice of newly diagnosed diabetes patients-a baseline study from Nepal. Int J Pharm Pract Teach 2012;3:245-52.
- Matwa P, Chabeli MM, Muller M, Levitt NS, Working Group of the National Diabetes Advisory Board, European IDDM Policy Group. Experiences and guidelines for footcare practices of patients with diabetes mellitus. Curationis 2003;26:11-21.
- Hasnain S, Sheikh NH. Knowledge and practices regarding foot care in diabetic patients visiting diabetic clinic in Jinnah Hospital, Lahore. J Pak Med Assoc 2009;59:687-90.
- Koenigsberg MR, Bartlett D, Cramer JS. Facilitating treatment adherence with lifestyle changes in diabetes. Am Fam Physician 2004;69:309-16.
- Raj P, Angadi MM. Hospital-based KAP study on diabetes in Bijapur, Karnataka. Indian J Med Spec 2010;1:80-3.
- Avi B, Colford J. Prevalence and Treatment of Diabetes in Rural Tanzania. Berkeley: University of California at Berkeley; 2012. Stephenson R, Hennink M. Barriers to family planning service use among the urban poor in Pakistan. Asia Pac Pop J 2004;19:5-26.
- Mehrotra R, Bajaj S, Kumar D. Use of complementary and alternative medicine by patients with diabetes mellitus. Natl Med J India 2004;17:243-5.
- International Diabetes Federation. Diabetes facts. Diabetes Atlas. 2nd and 3rd ed . Brussels, Belgium: International Diabetes Federation; 2006. Available from: http://www.worlddiabetesfoundation.org/composite-35. html. [Last retrieved on 2006 Apr 20].
- Shobhana R, Rama Rao P, Lavanya A, Williams R, Vijay V,Ramachandran A. Expenditure on health care incurred by diabetic subjects in a developing country – A study from southern India. Diabetes Res Clin Pract 2000;48:37-42.
- Kapur A. Economic analysis of diabetes care. Indian J Med Res 2007;125:473-82.
- Ramachandran A. Socio-economic burden of diabetes in India. J Assoc Physicians India 2007;55 Suppl: 9-12.
- Ramachandran A. Socio-Economic Burden of Diabetes in India. J Assoc Physicians India 2007;55:9-12.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.