Basal Cell Adenocarcinoma: A Population-Based Survival Analysis
Citation: Gore MR. Basal Cell Adenocarcinoma:A Population-Based Survival Analysis. Ann Med Health Sci Res. 2018;8:52- 56
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Basal cell adenocarcinoma is an uncommon basaloid malignancy seen most frequently in the salivary glands. Due to the rarity of this tumor data on survival and treatment is limited. Aim: The aim of this study was to examine factors affecting survival in patients with basal cell adenocarcinoma. Methods: The 1973-2014 Surveillance, Epidemiology, and End Results database was queried for patients with basal cell adenocarcinoma. The data was analyzed for tumor staging, site, and demographic characteristics. The Kaplan-Meier model was used to estimate actuarial survival. Results: A total of 247 patients were identified with complete TNM staging data. White patients represented 83.0% of the total (205/247). Patients were 51.0% female (126/247) and 49.0% male (121/247). Overall 5- and 10-year survival was 80.6% and 65.0%, respectively. Mean survival time was 100.8 months. Parotid gland was the most common site, followed by skin, submandibular gland, mouth/oral cavity, and vulva. Most patients were stage T1 or T2. Distant metastasis was present in only 1.6% (4/247) patients. 93.1% (230/247) of patients had surgical treatment. On univariate analysis T stage, primary tumor site, presence of distant metastasis, age, sex, and AJCC stage significantly affected survival. On multivariate analysis age and T stage remained significant. Conclusions: Basal cell adenocarcinoma is a basaloid malignancy most frequently seen in the parotid gland. The survival rate is high, and nodal and distant metastasis rates are low. Surgery is the mainstay of treatment, and T and M stage, primary site, age, sex, and AJCC stage all significantly affected survival.
Keywords
Basal cell adenocarcinoma; Salivary gland; SEER: Surveillance Epidemiology and End Results; Population based
Introduction
Basal cell adenocarcinoma is a rare malignancy most commonly seen in the salivary glands. [1,2] Basal cell adenocarcinoma represents ~ 1–2% of salivary gland neoplasms. It is indolent, with a local recurrence rate as high as 50% but a low metastasis and mortality rate. [1-4] Basal cell adenocarcinoma may arise from basal cell adenoma, is often a de novo malignancy. Basal cell adenocarcinoma may appear histologically similar to basal cell adenoma but will display local invasion and distinct morphology not seen in basal cell adenoma. [1] Given the rarity of basal cell adenocarcinoma, we utilized the SEER (Surveillance, Epidemiology, and End Results) database to identify patients diagnosed with basal cell adenocarcinoma. In 2016 Zhan and Lentsch published an excellent study of 509 patients with basal cell adenocarcinoma of the major salivary glands utilizing the 1998-2012 SEER database. This study sought to expand on and update that study with an examination of the 1973-2014 SEER cohort with patients with basal cell adenocarcinoma of any site, including the minor salivary glands and non-head and neck sites. This SEER cohort was used to identify demographic factors in this patient population, and to identify treatment, stage, and site characteristics that affect survival.
Methods
The most recent SEER database contains patient data from 1973-2014. Maintained by the National Cancer Institute, SEER collects data on cancer cases from various locations and sources throughout the United States, including various hospitals across many different states. The database, available at https://seer. cancer.gov/, was queried for malignant neoplasm, basal cell adenocarcinoma, any site, any age, and was extracted using SEER*Stat version 8.3.4 (National Cancer Institute, Bethesda, Maryland) and exported into Microsoft Excel 2016 (Microsoft Corporation, Redmond, Washington) for analysis. XLstat Biomed (Addinsoft, New York City, NY/Paris, France) was used for Kaplan-Meier overall survival analysis and log-rank analysis. Statistical significance was set at 0.05. SEER data was analyzed for overall survival, patient age, sex, and race, and overall AJCC (American Joint Committee on Cancer), tumor (T), nodal (N), and distant metastasis (M) stage, surgical treatment, and primary tumor site.
Results
A total of 247 patients with basal cell adenocarcinoma were identified from the SEER database. Patient demographics are summarized in Table 1. The majority of patients were > 55 years old, with age 60-64 years representing the largest group (40/247; 16.2%). The average age was 64.6 years, and the median age was 64.0 years (standard deviation 15.1 years). Basal cell adenocarcinoma had an almost equal sex predominance, with a 121:126 M:F ratio (1:1). Patients were 83.0% white (205/247), with black and other representing 16/247 (6.5%) and 23/247 (9.3%) of the remaining patients, respectively.
| Demographics | n | % |
|---|---|---|
| Total | 247 | 100% |
| Black | 16 | 6.5% |
| Other (American Indian/AK Native, Asian/Pacific Islander) | 23 | 9.3% |
| Unknown | 3 | 1.2% |
| White | 205 | 83.0% |
| Female | 126 | 51.0% |
| Male | 121 | 49.0% |
| Age | n | % |
| 05-09 years | 1 | 0.4% |
| 20-24 years | 1 | 0.4% |
| 25-29 years | 1 | 0.4% |
| 30-34 years | 6 | 2.4% |
| 35-39 years | 5 | 2.0% |
| 40-44 years | 10 | 4.0% |
| 45-49 years | 13 | 5.3% |
| 50-54 years | 22 | 8.9% |
| 55-59 years | 26 | 10.5% |
| 60-64 years | 40 | 16.2% |
| 65-69 years | 26 | 10.5% |
| 70-74 years | 27 | 10.9% |
| 75-79 years | 25 | 10.1% |
| 80-84 years | 23 | 9.3% |
| 85+ years | 21 | 8.5% |
Table 1: Patient demographics.
Table 2 illustrates the nodal metastasis, distant metastasis, and primary site characteristics of the SEER cohort. Parotid gland was the most common site, with 59.5% (147/247) of patients. Skin (any site) represented 16/247 (6.5%), submandibular gland represented 15/247 (6.1%), mouth/oral cavity represented 25/247 (10.1%), and vulva represented 25/247 (10. 1%). T stage was T0, T1a, or T2NOS (not otherwise specified), in 1/247 each (0.4%), T1 in 63/247 (25.4%), T1NOS in 12/247 (4.8%), T1b in 2/247 (0.8%), T2 in 67/247 (27.0%), T3 in 36/247 (14.5%), T4 in 2/247 (0.8%), T4a in 19/247 (7.7%), T4b in 5/247 (2.0%) and TX in 38/247 (15.3%). Distant metastasis (M) status was M0 in 230/247 (93.1%), M1 in 3/247 (1.2%), M1b in 1/247 (0.4%), and MX in 13/247 (5.3%). Nodal metastasis (N) status was N0 in 204/247 (82.6%), N1 in 22/247 (8.9%), N2 in 1/247 (0.4%), N2a in 1/247 (0.4%), N2b in 5/247 (2.0%), and NX in 14/247 (5.7%).
| AJCC stage | n | % |
|---|---|---|
| I | 66 | 26.7% |
| IA | 1 | 0.4% |
| IB | 2 | 0.8% |
| II | 55 | 22.3% |
| III | 44 | 17.8% |
| IV | 2 | 0.8% |
| IVA | 22 | 8.9% |
| IVB | 4 | 1.6% |
| IVC | 2 | 0.8% |
| IVNOS | 1 | 0.4% |
| NA | 2 | 0.8% |
| Unknown Stage | 46 | 18.6% |
| T stage | n | % |
| T0 | 1 | 0.4% |
| T1 | 63 | 25.4% |
| T1NOS | 12 | 4.8% |
| T1a | 1 | 0.4% |
| T1b | 2 | 0.8% |
| T2 | 67 | 27.0% |
| T2NOS | 1 | 0.4% |
| T3 | 36 | 14.5% |
| T4 | 2 | 0.8% |
| T4a | 19 | 7.7% |
| T4b | 5 | 2.0% |
| TX | 38 | 15.3% |
| Nodal Metastasis | n | % |
| N0 | 204 | 82.6% |
| N1 | 22 | 8.9% |
| N2 | 1 | 0.4% |
| N2a | 1 | 0.4% |
| N2b | 5 | 2.0% |
| NX | 14 | 5.7% |
| Distant Metastasis | n | % |
| M0 | 230 | 93.1 |
| M1 | 3 | 1.2% |
| M1b | 1 | 0.4% |
| MX | 13 | 5.3% |
| Primary Site | n | % |
| Anus | 1 | 0.4% |
| Breast | 1 | 0.4% |
| Colon | 1 | 0.4% |
| Lacrimal Sac | 1 | 0.4% |
| Lung | 1 | 0.4% |
| Parotid Gland | 147 | 59.5% |
| Penis | 1 | 0.4% |
| Prostate | 2 | 0.8% |
| Salivary Gland Other | 4 | 1.6% |
| Scrotum | 2 | 0.8% |
| Skin | 16 | 6.5% |
| Submandibular Gland | 15 | 6.1% |
| Vulva | 25 | 10.1% |
| Mouth/oral cavity | 25 | 10.1% |
| Nasal/sinus | 5 | 2.0% |
Table 2: Patient overall stage, TNM stage, and primary tumor site characteristics.
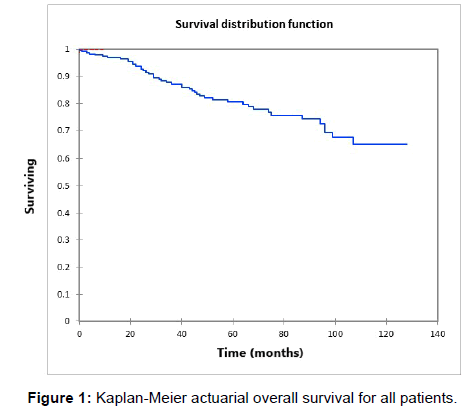
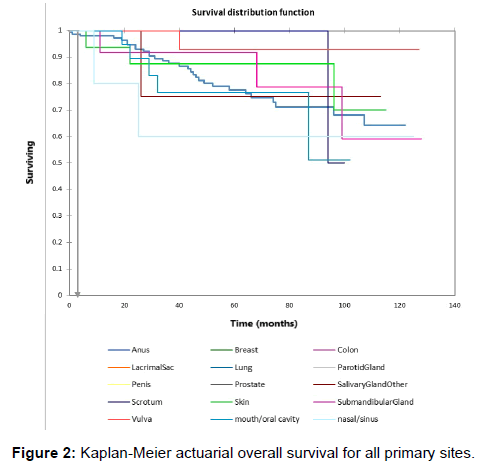
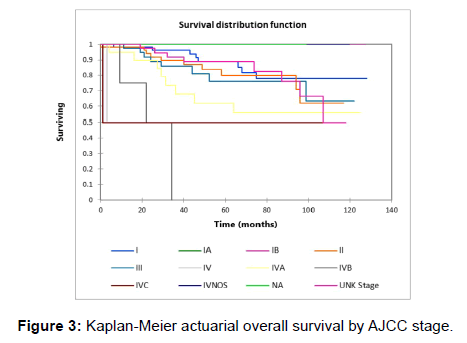
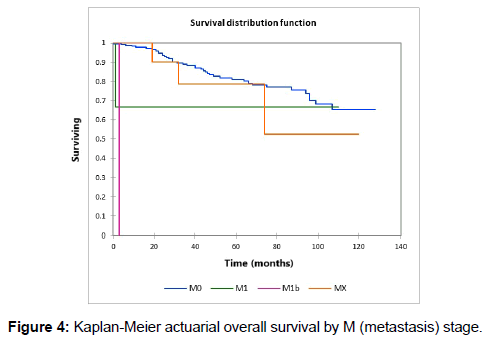
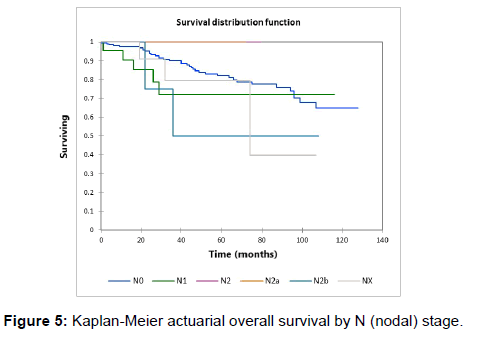
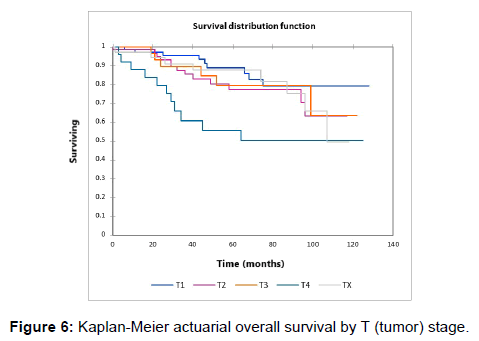
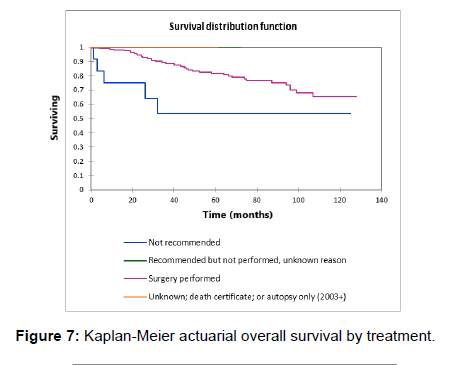
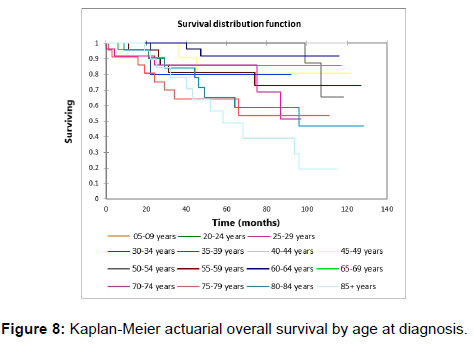
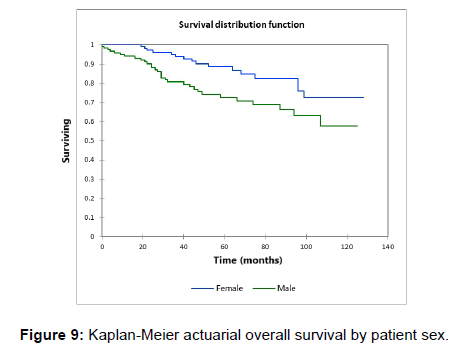
Figure 1 shows the Kaplan-Meier actuarial overall survival for the entire cohort. Five-year and 10-year overall survival was 80.6% and 65%, respectively. Figure 2 shows the Kaplan-Meier overall survival by primary site. Survival was lower for nasal/ sinus and prostate vs. vulva, parotid gland, and submandibular gland and other sites (p<0.001). Figure 3 illustrates the Kaplan-Meier overall survival by overall AJCC (American Joint Committee on Cancer) stage. Survival was significantly lower for Stage III and IV tumors than Stage I and II tumors (p=0.001). Figure 4 illustrates the Kaplan-Meier overall survival by M stage. Survival was significantly lower for M1 patients than M0 patients (p<0.001). Figure 5 shows the Kaplan-Meier overall survival by nodal (N) stage. There was no statistically significant difference in survival for differing N stages (p=0.7). Figure 6 shows the Kaplan-Meier overall survival by tumor (T) stage. Survival for patients with T4 tumors was significantly lower than survival for patients with T1, T2, or T3 tumors (p=0.02). Figure 7 illustrates the Kaplan-Meier overall survival for patients based on surgical vs. non-surgical treatment. Overall survival was lower for patients in whom surgery was not recommended vs. patients on whom surgery was performed, but this difference was not statistically significant (p=0.06). Figure 8 illustrates the Kaplan-Meier overall survival for patients by age at diagnosis. Survival was significantly lower for patients aged > 70 at time of diagnosis (p=0.001). Figure 9 illustrates the Kaplan-Meier overall survival by sex. Survival was significantly lower for males than for females (p=0.009). There was no significant difference in survival by race (p=0.9). Multivariate analysis using linear regression demonstrated that age >70 at diagnosis (p<0.001) and T4 stage vs. T1, T2, and T3 (p=0.01) remained significant predictors of survival. On multivariate analysis higher AJCC stage (p=0.07) and sex (p=0.05) approached significance.
Discussion
Basal cell adenocarcinoma is a malignant basaloid neoplasm most commonly seen in salivary tissue, particularly the parotid gland in older individuals. [1] It is relatively uncommon, representing approximately 1-2% of salivary gland neoplasms. [1] Zhan and Lentsch examined the records of over 500 patients with basal cell adenocarcinoma of the major salivary glands from the 1998-2012 SEER database in 2016 [5] and found that basal cell adenocarcinoma represented 1.4% of major salivary gland cancers, with the parotid gland representing the primary site in 88% (448/509). Submandibular gland and minor salivary gland tumors have also been reported. [5-7] Basal cell adenocarcinoma was first described by Klima et al., and can have a similar appearance and histologic patterns to basal cell adenoma (solid, trabecular, tubular, membranous), but with more prevalent necrosis and mitoses, and with local tissue invasion. [3,4,8] Wilson and Robinson noted a recurrence rate of 16.7% in a clinicopathological review of 29 basal cell adenocarcinomas, with one patient having distant metastasis (3.4%). [1] In the present study including all sites we noted that basal cell adenocarcinoma was most prevalent in patients over 60 years old, with a mean age of 64 years and an average age of 64.6 years. In their study of patients with major salivary gland adenocarcinoma Zhan and Lentsch also noted an average age of 64 years. In the present study we noted a distant metastasis rate of 1.6% (4/247). Zhan and Lentsch noted a distant metastasis rate of 1.8% (9/509). These relatively low metastasis rates are consistent with the relatively low-grade behavior of basal cell adenocarcinoma. Wilson and Robinson [1] reported 12 tumors in male patients and 17 in female patients (1:1.4 M:F ratio). We noted a minimal female predominance, with a 121:126 male to female ratio in the present cohort (1:1 M:F). Zhan and Lentsch noted 50.7% men/49.3% women in their study. [5] Wilson and Robinson also noted that basal cell adenocarcinoma was most prevalent in the parotid gland (75.9% of their cohort), while in the present cohort we noted the parotid gland as the primary site in 147/247 (59.5%), with skin (16/247; 6.5%), submandibular gland (15/247; 6.1%), Vulva (25/247; 10.1%) and Mouth/oral cavity (25/247; 10.1%) also representing significant number of patients. This prevalence of the parotid as the most common primary site is logical given the large size of the parotid and is seen with other salivary neoplasms as well. Wilson and Robinson [1,2] noted that histological evidence of local tissue invasion was superior to mitotic rate or immunohistochemical markers in differentiating basal cell adenocarcinoma from basal cell adenoma. The mean follow-up in the Wilson and Robinson study was 59 months, and they noted one death in the single patient noted to have distant metastasis, for a mortality rate of 3.4%. In the present cohort the mean survival time was 100.9 months, and we noted an overall survival at 5- and 10-years of 80.6% and 65%, respectively. Zhan and Lentsch noted overall survival at 5 and 10 years of 79% and 62%, respectively [5]. Ellis et al. noted a total of 3/29 patients with metastases to local lymph nodes or distant metastases (10.3%), and they noted one death from distant metastases (3.4%). [4] Zhan and Lentsch noted a regional metastasis (N+) rate of 11.9%, while the present study noted positive regional nodal metastasis in 29/247 (11.7%). Again, these relatively low regional metastasis rates and relatively high survival are consistent with the low-grade malignant behavior of basal cell adenocarcinoma.
Univariate Kaplan-Meier survival analysis of the present SEER cohort noted primary site, greater AJCC stage, presence of distant metastasis (M1), age > 70, male sex, and higher T stage as significant predictors of survival. N stage and race did not impact survival in the present cohort and while surgical treatment vs. nonsurgical treatment approached significance it was not found to be a significant predictor of survival in the present cohort (p=0.06). In the present cohort 5-year survival in M0 patients was 78%, while 5-year survival in M1 patients was 67% and in M1b patients’ 5-year survival was 0%. Patients who had surgery performed had 5- and 10-year survival rates of 81.7% and 65.3%, respectively, while patients for whom surgery was not recommended had 5- and 10-year survival rates of 53.6% and 53.6%, respectively (p=0.06). Primary site also significantly influenced survival on univariate analysis. Parotid, vulva, skin, and submandibular gland demonstrated significantly higher overall 5- and 10-year survival when compared to patients with nasal/sinus or prostate primary sites (p<0.001). While it is difficult to discern the cause for the higher mortality with nasal/sinus and prostate primary sites, it may be due to the less evident location of these tumors vs. the parotid, submandibular gland, skin, or vulva leading to a delay in discovery of basal cell adenocarcinoma in the nasal/sinus cavity or prostate. With regard to surgical vs. non-surgical treatment, it is possible that with the low-grade behavior of basal cell adenocarcinoma, surgery is more effective than radiation or chemotherapy, which are often more effective in tumors with higher mitotic and/or metabolic rates. On multivariate analysis age greater than 70 at the time of diagnosis (p<0.001) and T4 tumor vs. T1, T2, or T3 tumors (p=0.01) remained significant predictors of overall survival. Zhan and Lentsch similarly found that for major salivary gland tumors, on multivariate analysis, only age ≥ 65 (p < 0.001) and high primary tumor (T)-stage (p=0.01) remained significant predictors of survival. [5] This is logical, as higher tumor stage likely makes complete resection more difficult, and with regards to overall survival increasing age decreases overall life-expectancy and likely adds comorbidities that may make aggressive surgical treatment of basal cell adenocarcinoma more difficult.
This study has several limitations. The retrospective nature and reporting constraints of the SEER database make selection bias and recall bias possible. Additional data on chemotherapy and radiation treatment would also have been useful, although surgical treatment appeared to be the mainstay of treatment for this less aggressive tumor. The inclusion of non-salivary gland tumors vs. major salivary gland tumors only included in the Zhan and Lentsch study has the potential to add heterogeneity given the differing staging systems for different tumor sites, but the similar survival data and similar factors affecting survival, particularly the consistent significance of age and T stage on multivariate analysis, strengthens the body of data available for this rare tumor, especially with the updated 2013 and 2014 SEER data. The inclusion of the survival data for the less common sites such as vulva and nasal/sinus are useful as these sites are much less prevalent than the parotid gland, but represent a similar number of patient primary sites as the submandibular gland. The SEER database has been shown to represent a valuable source for population-based analyses of treatment and survival, especially in relatively rare malignancies. [8,9] The relatively large patient cohort allowed confirmation of observations seen in previous studies, namely the roughly equal male to female ratio with a slight female predominance, higher prevalence and worse survival in older patients, the most common primary site being the parotid, and the very low mortality, lymph node metastasis, and distant metastasis rates in basal cell adenocarcinoma. [10]
Conclusion
This study examined a relatively large cohort of patients from the SEER 1973-2014 database with a diagnosis of basal cell adenocarcinoma. The rates of local and distant metastasis were very low, and while N stage did not appear to effect survival, male sex, higher AJCC stage, higher T stage and the presence of distant metastases did have a significant relationship with overall survival. Additionally, the more prevalent primary sites such as parotid, submandibular gland, and vulva appeared to show statistically increased overall survival relative to less common primary sites such as prostate and nasal/sinus. Surgical treatment with negative margins appears to be the mainstay of treatment, and long-term survival is the norm, with low mortality rates seen in patients with basal cell adenocarcinoma.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Wilson TC, Robinson RA. Basal cell adenocarcinoma and Basal cell adenoma of the salivary glands: A clinicopathological review of seventy tumors with comparison of morphologic features and growth control indices. Head Neck Pathol. 2015; 9: 205-213.
- Wilson TC, Ma D, Tilak A, Tesdahl B, Robinson RA. Next-generation sequencing in salivary gland basal cell adenocarcinoma and basal cell adenoma. Head Neck Pathol. 2016; 10: 494-500.
- Muller S, Barnes L. Basal cell adenocarcinoma of the salivary glands. Report of seven cases and review of the literature. Cancer. 1996; 78: 2471-2477.
- Ellis GL, Wiscovitch JG. Basal cell adenocarcinomas of the major salivary glands. Oral Surg Oral Med Oral Pathol. 1990; 69: 461-469.
- Zhan KY, Lentsch EJ. Basal cell adenocarcinoma of the major salivary glands: A population-level study of 509 cases. Laryngoscope. 2016; 126: 1086-1090.
- Veeresh M, Bavle RM, Vinay KN, Nandakumar H. Basal cell adenoma of the submandibular gland. J Maxillofac Oral Surg. 2010; 9: 289-291.
- Fantasia JE, Neville BW. Basal cell adenomas of the minor salivary glands. A clinicopathologic study of seventeen new cases and a review of the literature. Oral Surg Oral Med Oral Pathol. 1980; 50: 433-440.
- Klima M, Wolfe K, Johnson PE. Basal cell tumors of the parotid gland. Arch Otolaryngol. 1978; 104: 111-116.
- Chung SY, Unsal AA, Kiliç S, Baredes S, Liu JK, Eloy JA. Pediatric sinonasal malignancies: A population-based analysis. Int J Pediatr Otorhinolaryngol. 2017; 98: 97-102.
- Unsal AA, Chung SY, Unsal AB, Baredes S, Eloy JA. A population-based analysis of survival for sinonasal rhabdomyosarcoma. Otolaryngol Head Neck Surg. 2017; 157: 142-149.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.