Bilobed Perirectal Epidermoid Cyst: An Unusual Cause of Hematochezia in a Middle‑aged Woman
- *Corresponding Author:
- Dr. Atolagbe AO
630 Lenox Avenue, New York, NY 10037, USA.
E-mail: eureka303d@gmail.com
Citation: Atolagbe AO, Ogunleye O, Apakama CT. Bi-lobed perirectal epidermoid cyst: An unusual cause of hematochezia in a middle-aged woman. Ann Med Health Sci Res 2016;6:190-2.
This is an open access article distributed under the terms of the Creative Commons Attribution–NonCommercial–ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non–commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Perirectal epidermoid cysts are congenital cysts originating from the ectodermal germ cell layer of the hind gut. Their presenting symptoms are most often nonspecific and distinguishing them from other presacral developmental cysts often present a diagnostic and therapeutic dilemma. We present a 58‑year‑old woman who presented with chronic dyschezia and hematochezia of a few days duration and no prior colonoscopies. Initial blood work and tumor markers were unremarkable. Pelvic magnetic resonance imaging (MRI) showed a 7.5 cm × 5 cm × 6 cm homogenous bi‑lobed cystic mass in the pelvis adherent to the left lateral wall of the rectum and posteriorly to the sacrum with a displacement of the rectum anteriorly and to the right. There was no pelvic sidewall adenopathy or free fluid in the pelvis. Preoperative colonoscopy showed rectal compression with no rectal involvement of the mass. The cyst was successfully resected posteriorly via the trans‑sacrococcygeal approach. An intraoperative proctosigmoidoscopy confirmed an intact rectum. The patient remains recurrence‑free 1 year postsurgical resection.
Keywords
Perirectal, Epidermoid cyst, Bi‑lobed, Posterior approach
Introduction
Perirectal epidermoid cysts are developmental cysts that rarely present in adulthood and are typically unilobular on imaging. They rarely cause hematochezia as opposed to tailgut cysts. We present a woman with clinical evidence of hematochezia and a bi‑lobed cystic tumor on pelvic MRI. We successfully resected the tumor via the posterior approach.
Case Report
We report a case of a 58‑year‑old Spanish woman resident in New York who presented at our facility with complaints of constipation which had worsened over the past 6 months and onset of hematochezia of a 3 days duration. Her past medical history was statistically significant for schizoaffective disorder and gastroesophageal reflux disease.
Clinical examination revealed a healthy middle‑aged woman with a body mass index of 28.1 kg/m2 and normal vital signs. The only abnormal finding on clinical examination was a palpable circumscribed mass compressing on her rectum by digital rectal examination. Her rectum was also filled with hard, pellet‑like feces, and altered blood. Blood electrolytes were normal and complete blood count was also normal. Her admitting hematocrit was 46%, and fecal occult blood test was positive. Alpha‑fetoprotein, carcinoembryonic antigen, and ca ‑ 199 tumor markers were all normal. The patient was admitted and serial hematocrit measurements remained within normal limits. An upper gastrointestinal endoscopy on the 2nd day of admission showed gastritis.
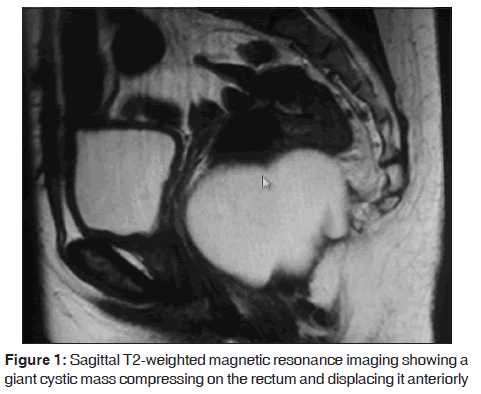
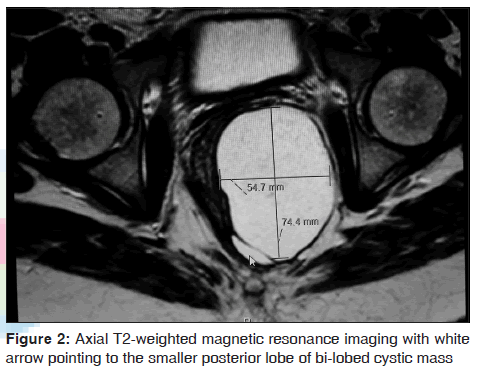
Pelvic MRI [Figures 1 and 2] revealed a 7.5 cm × 5 cm × 6 cm cystic pelvic mass adherent anteriorly to the left lateral wall of the rectum and also adherent to the sacrum posteriorly. There were compression and displacement of the rectal lumen anteriorly and to the right. There was an absence of the uterus from a prior hysterectomy. There was no pelvic sidewall adenopathy or free fluid in the pelvis.
The clinical consideration at this juncture was the possibility of a developmental cyst with low considerations for cystic ovarian or rectal neoplasms due to negative relevant symptomatology and negative tumor markers. A colonoscopy revealed a significant narrowing of the rectum with mucosal erythema and inflammation but no active bleeding. There was no evidence of intra‑luminal communication of the tumor.
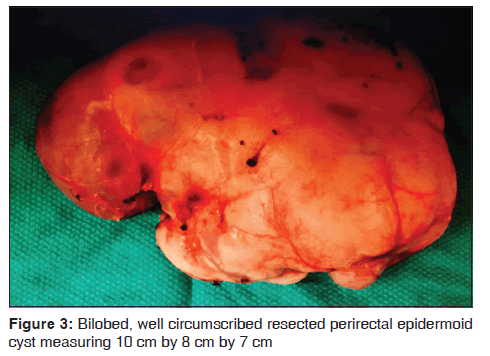
She underwent an elective surgical excision in which the posterior trans‑sacrococcygeal technique was utilized. The patient was positioned in the jackknife position, and a midline incision was made over the coccyx and deepened to the bone with resection of the coccygeal bone. The posterior rectal fat was carefully dissected utilizing both blunt, sharp dissection, and the mass [Figure 3] was completely excised from surrounding structures. Grossly, the cyst was tan – colored, weighed approximately 0.8 kg and measured 10 cm × 6 cm × 7 cm in its greatest dimension. It contained a cheesy gelatinous material. Intraoperative flexible proctoscopy confirmed an intact rectum. The surgical wound was closed in layers with a size 10 Jackson‑pratt drain left in situ. Pathology was compatible with the epidermoid cyst. No coccygeal involvement, no atypia or malignancy was identified on histology. She was subsequently discharged on the third postoperative day following drain removal. The patient remains recurrence‑free 1 year postsurgical resection.
Discussion
Perirectal epidermoid cysts are a form of congenital developmental cysts that arise from embryonic primordial germ layers in the hind gut.[1] There is no specific true incidence for perirectal epidermoid cysts; however, an incidence of 1 in 40,000 to 1 in 63,000 hospital admissions has been reported in the literature for presacral developmental cysts.[1] They are ectodermal in origin and are found in the potential space bounded by the sacrum posteriorly and the rectum anteriorly. The peritoneal reflection forms the superior margins of this space while the levator muscles form the inferior boundary.[1]
Perirectal epidermoid cysts are typically slow growing masses and very prone to recurrence if not completely resected. The typical picture is an asymptomatic middle‑aged woman with the incidental discovery of a cystic pelvic mass on imaging. Symptomatic compression of pelvic structures by the enlarging cyst may result in urinary complaints, constipation or dyspareunia. The hematochezia noted in our patient could be attributed to chronic irritation of the rectal mucosa. This is not surprising considering the statistically significant rectal luminal narrowing and collapse noted on colonoscopy.
Multiple forceful attempts at voiding impacted feces through a stenosed rectal lumen could also irritate the mucosa and cause bleeding. Symptoms of dyschezia and hematochezia may also be due to cyst inflammation or infection while patients may also present with complications such as perianal fistulous drainage.[2] Carcinomatous degeneration is unusual but has been reported in epidermoid cysts.[2]
Circumscribed unilobular fluid‑filled cystic lesions may be seen on ultrasound or tomographic imaging of epidermoid cysts. The cyst presented in this case report was bi‑lobed and filled with gelatinous material. Computed tomographic imaging can distinguish between solid and cystic masses and show evidence of adjacent organ, neural or bony involvement – this is unusual in epidermoid cysts and typically distinguishes them from other developmental cysts.[3] Contrast‑enhanced magnetic resonance imaging is the gold standard for diagnosis with a high sensitivity in determining tumor nature, tumor extent, and local invasion.[2,3] Tumor heterogeneity on MRI is a typical pointer to malignancy in presacral developmental cysts.[3,4]
The role of presurgical pathologic diagnosis is controversial. Cystic lesions are typically benign and do not require preoperative tissue diagnosis by either fine needle aspiration or core needle biopsy.[1] Complete surgical excision is the ultimate aim of management. This may be open or laparoscopic and is dependent on access to the mass, the size and relationship of the cyst with the rectum, surgeon technicality and the possibility of malignancy.[1]
An open or laparoscopic abdominal approach is often indicated for cysts with a primary intra‑abdominal component. Cystic tumors located in the upper rectum and abutting into the abdominal cavity may be surgically resected via an abdominal laparotomy. A combined abdominal‑perineal route is indicated for large cysts extending above and below S3 in which complete resection via a strictly perineal approach will be technically impossible. Posterior resection could be utilized for tumors located below the mid‑body of S3. Multiple techniques, such as the trans‑sacral or para‑sacrococcygeal, posterior sagittal, intersphincteric, transsphincteric or trans‑sacrococcygeal approaches, have been described. Disadvantages of the posterior approach include limited surgical space and a higher risk of pelvic neurovascular injury.[1]
The prognosis of resected pelvic epidermoid tumors is good especially when complete surgical resection is achieved, and intraoperative surgical spillage is avoided due to their propensity for recurrence.[5]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Saxena D, Pandey A, Bugalia RP, Kumar M, Kadam R,Agarwal V, et al. Management of presacral tumors: Our experience with posterior approach. Int J Surg Case Rep 2015;12:37–40.
- Yang DM, Kim HC, Lee HL, Lee SH, Kim GY. Squamous cell carcinoma arising from a presacral epidermoid cyst: CT and MR findings. Abdom Imaging 2008;33:498–500.
- Yang BL, Gu YF, Shao WJ, Chen HJ, Sun GD, Jin HY, et al.Retrorectal tumors in adults: Magnetic resonance imaging findings. World J Gastroenterol 2010;16:5822–9.
- Michael D, Cohen CR, Northover JM. Adenocarcinoma within a rectal duplication cyst: Case report and literature review. Ann R Coll Surg Engl 1999;81:205–6.
- Wang JY, Hsu CH, Changchien CR, Chen JS, Hsu KC, You YT, et al. Presacral tumor: A review of forty–five cases. Am Surg 1995;61:310–5.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.