Cervical Cytology among HIV Positive and HIV Negative Women in a Tertiary Hospital in North Central Nigeria: A Comparative Study
2 Department of Obstetrics and Gynaecology, College of Health Sciences, University of Abuja, Abuja, Nigeria, Email: etagida@yahoo.com
3 Department of Obstetrics and Gynaecology, University of Abuja Teaching Hospital, Abuja, Nigeria
4 Department of Pathology, College of Health sciences, University of Abuja, Abuja, Nigeria
Citation: Lawal I, Agida TE, Offiong RA, Oluwole PO. Cervical Cytology among HIV Positive and HIV Negative Women in a Tertiary Hospital in North Central Nigeria: A Comparative Study. Ann Med Health Sci Res. 2017; 7: 308-311
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Nigeria carries the second highest burden of HIV/AIDS disease in the world. Several studies have shown a higher prevalence of pre-invasive and invasive cervical pathology among HIV positive population compared to their HIV negative cohorts. Aim: The aim of this study was to look at the prevalence of cervical intraepithelial lesion among HIV positive women compared to their HIV negative counterparts seen at the University of Abuja Teaching Hospital, Gwagwalada. Subjects and Methods: This was a comparative analytical study of 135 HIV positive and 135 HIV negative women assessing healthcare services in the Special Treatment clinic, Gynaecological and Family Planning clinics of the hospital. Pap smear was collected from each of the study groups. The specimens went through processing and the slides were read by a Consultant Histopathologist. The data was analyzed using SPSS version 16 and level of significance was set at P<0.5. Results: Sixty three (46.7%) of the HIV positive and 111 (82.2%) of the HIV negative groups were married. Abnormal Pap smear results were seen in 17 (12.6%) HIV negative women and 76 (56.3%) HIV positive women, Six HIV positive women had CD4 count of <200 cells/ml. Among them, 3 had moderate cervical dysplasia while the other 3 had severe cervical dysplasia. Conclusion: The study has demonstrated that abnormal cervical smear is more prevalent among HIV positive than HIV negative women. Therefore, there is a need to incorporate routine cervical cancer screening services into the existing HIV/AIDS programmes in Nigeria.
Keywords
Cervical smear; HIV negative; HIV positive; Results; Women
Introduction
Human immunodeficiency Virus has been a major global public health issue of the century. At the end of 2014, there were approximately 36.9 million people living with HIV, with 2.0 million new infections that year [1]. Sub-Saharan Africa is the most affected region, with 25.8 million people living with HIV by the end of that year [1].
According to the United Nations Programme on HIV/AIDS (UNAIDS), Nigeria carries the second highest HIV/AIDS burden in the world with 3.4 million people living with the virus by the end of 2014. The National Prevalence as at 2014 was 4.1% [2].
An association between HIV and cervical cancer was first suspected in 1998 when Nicole et al. demonstrated that there was a significant change in the cell cycle through the expression of certain regulatory proteins in cervical smears from patients co-infected with HPV and HIV, compared to a control group [3]. Epidemiological, molecular and clinical evidences have shown that cervical cancer is caused by human papilloma virus, a sexually transmitted infection, especially serotype 16 and 18 [4-8].
Human papilloma virus infection is common in Nigeria as a study in Ibadan showed an overall prevalence of 26.3%, while the prevalence among women without cervical lesions was 24.8% [9]. It is estimated that about 23.7% of women in the general population in Nigeria harbor cervical HPV at a time [10]. Cervical cancer currently ranks as the second most frequent cancer among women in Nigeria, as every year, 14089 women are diagnosed with the disease [10].
Several studies have shown a higher prevalence of preinvasive and invasive cervical pathology among HIV positive population compared to their HIV negative cohorts [11-17]. Most of these studies were conducted outside Nigeria. Both HIV and HPV are sexually transmitted. In HIV negative women with competent immune systems, most of the infections are cleared spontaneously because of a cell mediated immune response regulated by CD4+ lymphocytes [12]. However, in HIV co-infected individuals, there is a higher risk of persistent HPV infection largely due to their impaired ability to clear HPV. They are therefore, at increased risk of developing cervical dysplasia and cancer [18]. In another study, it was found that the 5-year cumulative incidence of squamous intraepithelial lesions that were high grade or greater (HSIL+) and carcinoma in-situ (CIN) was similar in HIV positive and HIV negative women who had cytologically normal pap test at enrollment [19].
There is paucity of knowledge on this subject matter, especially from the Northern part of Nigeria. The aim of this study was, therefore to look at the prevalence of cervical intraepithelial lesion amongst HIV positive women compared to their HIV negative counterparts at the University of Abuja Teaching hospital, Abuja, Nigeria.
Materials and Methods
Study design and setting
This was a comparative analytical study of HIV positive and HIV negative women assessing healthcare in the Special Treatment clinic, Gynaecological and the Family Planning clinics of the University of Abuja Teaching Hospital, Abuja. The University of Abuja Teaching Hospital is a 350 bed Federal tertiary hospital located in Gwagwalada, a suburb of Abuja, the Federal Capital Territory. The hospital runs a busy Special Treatment clinic that caters for over 10,000 HIV positive men and women.
Study population
All the HIV positive clients were recruited from the Special Treatment Clinic while the HIV negative cohorts were recruited from the Family Planning and gynaecological clinics after proper counselling. All the subjects had documented evidence of their HIV status and written informed consent was obtained from them. HIV screening was done by qualified Laboratory scientists either in the main hospital laboratory or in the Special Treatment Clinic laboratory. Women with known HIV status who were eligible for screening for cervical cancer were included. Those who declined consent, had treatment for preinvasive cervical lesion, were diagnosed as having cervical cancer or who were pregnant were excluded from the study.
Sample size determination
The sample size was calculated using the formula Where:
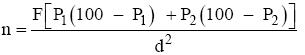
n = minimum sample size
F = a factor determined by Significance level and Power
P1= Prevalence of abnormal cervical cytology among HIV positive patients
P2 = Prevalence of abnormal cervical cytology among HIV negative patients
d = difference in prevalence of clinical significance
Using a Prevalence of abnormal cervical cytology of 12.6% in HIV positive and 4.6% in HIV negative patients as reported from a previous study in Nigeria [20]., to detect 10% difference in prevalence of cervical cytology abnormalities between the two arms of the study at a significance level of 5%, with a power of 80% at 95% Confidence Interval, a sample size of 121 was calculated for each arm of the study. This was rounded up to 135, given an attrition rate of 10%.
Methodology
After obtaining an informed consent, Pap smear was collected from each of the study groups between 2nd of May to 8th of June 2012. Study identification code, which was each participant’s serial enrolment number was generated to ensure confidentiality. Sample of exfoliated cells from the cervix of each participant was collected by placing the spatula firmly on the cervix, with the tip of the spatula within the cervical canal and rotating 360 degrees. The spatula was then smeared on a labelled frosted slide. The labelling was with the study code generated for the particular participant. The slide was fixed immediately in 95% alcohol and transported to the laboratory in a coupling jar.
The slides were stained using Papanicolaou staining technique. They were then stained with haematoxylin and decolorized with 95% alcohol solution, rinsed with water and stained with Orange G stain. They were then decolorized with 95% alcohol, stained with eosin azure and further decolorized with 95% alcohol and air dried.
The slides were read by the Consultant Histopathologist who was blinded to the HIV status of the participants. Data was analyzed using Statistical Package for Social Science (SPSS) version 16. Socio-demographic characteristics and other relevant information were obtained from the participants’ case notes. Descriptive statistics were used where appropriate. Chi Square test and Fisher’s exact test were used to compare proportions. Level of significance was set at P<0.05 for analysis, cytology results were categorized as normal, inflammatory, mild dysplasia, moderate dysplasia and severe dysplasia.
Ethical approval
Approval for the study was obtained from the Human Research Ethical Committee of the University of Abuja Teaching Hospital, Nigeria.
Results
A total of 270 women participated in the study, made up of 135 HIV positive and 135 HIV negative women.
The demographic characteristics are shown in Table 1. The mean age of all the participants was 34.5 (6.9) years. There was no significant difference between the mean ages of the two groups [34.47(6.21) and 34.49(6.91) years, P=0.25]. Majority of the participants were Christians in both groups [109/135 and 105/135 (80.7% and 77.8%) respectively]. Majority of them were petty traders. Their educational status showed that 46.7% (63/135) amongst the HIV positive group had secondary level of education, and they constituted the largest group. However, 56% (76/135) of the HIV negative group had tertiary education. The table also shows that 5.7% (77/135) of the HIV positive and 82.2% (111/135) of the HIV negative group respectively were married. This was statistically significant (X2=26.45, P<0.05).
| Age distribution | HIV Negative | % | HIV Positive | % |
|---|---|---|---|---|
| 20 – 30 | 35 | 25.9 | 35 | 25.9 |
| 31 – 40 | 72 | 53.3 | 58 | 43 |
| 41 – 50 | 28 | 20.7 | 36 | 26. 7 |
| 51 – 60 | - | - | 6 | 4.4 |
| Total | 135 | 100 | 135 | 100 |
| Religion | ||||
| Islam | 30 | 22.2 | 26 | 19.3 |
| Christianity | 105 | 77.8 | 109 | 80.7 |
| Total | 135 | 100 | 135 | 100 |
| Occupation | ||||
| Civil servant | 34 | 25.2 | 22 | 16.3 |
| Trader | 52 | 38.5 | 53 | 39.3 |
| Farmer | 3 | 2.2 | 4 | 3 |
| Artisan | 5 | 3.7 | 31 | 23 |
| Unemployed | 17 | 12.6 | 15 | 11.1 |
| Student | 24 | 17.8 | 10 | 7.4 |
| Total | 135 | 100 | 135 | 100 |
| Educational status | ||||
| None | 5 | 3.7 | 14 | 10.4 |
| Primary | 9 | 6.7 | 15 | 11.1 |
| Secondary | 45 | 33.3 | 63 | 46.7 |
| Tertiary | 76 | 56.3 | 43 | 31.9 |
| Total | 135 | 100 | 135 | 100 |
| Marital status | ||||
| Married | 111 | 82.2 | 77 | 57 |
| Single | 21 | 15.6 | 33 | 24.4 |
| Divorced | - | - | 6 | 4.4 |
| Widow | 3 | 2.2 | 19 | 14.1 |
| Total | 135 | 100 | 135 | 100 |
Table 1: Demographic characteristics.
Pap smear results are shown in Table 2. All the categories of cervical cytology abnormalities were proportionately higher among the HIV positive group.
| Result | HIV negative | % | HIV positive | % |
|---|---|---|---|---|
| Negative | 118 | 87.4 | 76 | 56.3 |
| Inflammatory | 9 | 6.7 | 23 | 17 |
| Mild dysplasia | 6 | 4.4 | 10 | 7.4 |
| Moderate dysplasia | - | - | 23 | 17 |
| Severe dysplasia | 2 | 1.5 | 3 | 2.2 |
| Total | 135 | 100 | 135 | 100 |
Table 2: Pap smear results.
Table 3 shows Pap smear results with the CD4 counts amongst the HIV positive participants. One hundred and twenty-nine out of the 135 (95.6%) participants had CD4 counts greater than 200 cells/ml while 4.4% (6/135) participants had CD4 count <200 cells/ml. Of the 6, 3 had moderate cervical dysplasia while 3 had severe dysplasia.
| Pap smear result | CD4 < 200 | % | CD4 > 200 | % |
| Negative | - | - | 76 | 56.3 |
| Inflammatory | - | - | 23 | 17.04 |
| Mild dysplasia | - | - | 10 | 7.41 |
| Moderate dysplasia | 3 | 2.22 | 20 | 14.81 |
| Severe dysplasia | 3 | 2.22 | - | - |
| Total | 6 | 4.44 | 129 | 95.56 |
Table 3: Distribution of Pap smear results and CD4 levels among HIV positive subjects.
Discussion
This study has demonstrated a higher prevalence of cervical cytology abnormalities among HIV positive women compared to their HIV negative counterparts. This is consistent with findings from other studies [11,13,16,20,21-25]. However, some other studies have not shown higher risk of these abnormalities among HIV positive women [19,26]. The prevalence of cervical dysplasia of 26.6% among HIV positive found in this study is similar to 29% found in Jos, Nigeria [24]. It is however, higher than 10.7%, 12.6% and 17.8% found in Lagos, Enugu and Makurdi respectively [20,21,25] and lower than 31.3% found in Maiduguri [22].
HIV positive women are said to carry a high risk HPV at higher rate (67%) and have higher rates of cervical dysplasia [27,28]. HPV can induce a local immune deficiency by depleting intraepithelial lymphocytes, Langerhans cells and CD4 + cells with down-regulation of cytokine production [29]. People with cell-mediated immune dysfunction have higher rates of HPV infection and are more likely to manifest large, multifocal and dysplastic lesions. This is because clearance of HPV can be impaired by decreased immune competence [29].
The varying prevalence could be due to differences in the study population. The observed lower tertiary level of education among the HIV positive arm of this study could be due to the fact that most of the HIV clients that belong to high socioeconomic class in Nigeria shun public hospitals for confidential reasons. Furthermore, Dim et al. observed that women with higher educational background are more likely to have better income, since poverty has been identified as an underlying factor driving HIV/AIDS in Nigeria [20]. Again, HIV positive patients with high economic purchasing powers are more likely to access HIV support services in private facilities. Even if they access the services in public health facilities, they are likely to sneak in and sneak out, possibly due to fear of stigmatization. That may explain why majority of the participants in this study were petty traders.
The introduction of HAART in the late 1990s led to dramatic improvement in clinical outcomes and life expectancies for people living with HIV/AIDS. It also gave hope that improved immunological status would lead to better clearance of HPV infection in HIV positive women [30].
Limitation
One limitation of this study is the fact that it did not look at effects of HAART on cervical cytology abnormalities. It has been observed that data regarding the impart of HAART on reducing incidence and progression or facilitating the regression of HPV infection and cervical abnormalities is largely inconsistent [30-32]. Future studies may have to address that.
Conclusion
This study has demonstrated significant difference in the prevalence of cervical cytology abnormalities between HIV positive and HIV negative women assessing healthcare services in our hospital. This therefore, emphasizes the need to incorporate routine cervical cancer screening into the existing HIV/AIDS programs in Nigeria.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- World Health Organization. HIV/AIDSFact Sheet no. 360. November 2015.
- UNAIDS-3.4 million Nigerians contracted HIV/AIDS in 2014. Available at http://www.informationng.com/2015/09/3-4m-nigerians-contracte-hivaids-in-2014-u Assessed on 15/03/2016.
- Nicol AF, Pires ARC, De Sauza SR, Nuovo GJ, Grinsztejn B, Tristao A, et al. Cell-cycle and suppressor proteins expression in uterine cervix in HIV/HIV co-infection: comparative study by tissue micro-array TMA). BMC Cancer 2008: 289.
- Prat J. Pathology of cancers of the female genital tract. Int J GynaecolObstet 2012; 119:S137-150.
- Stanley M. Human papilloma vaccines versus cervical cancer screening. ClinOncol 2008; 20: 388-394.
- Steller MA. Cervical cancer: A vaccine-preventable malignancy. Female Patient 2006; 31: 9-10.
- Haefner HK. Update on human papilloma virus. Supplement to SRM, Nov. 2008:15-16.
- Paavonen J. Human Papillomavirus infection and the development of cervical cancer and related neoplasia. Int J Infect Dis 2007; 11 Suppl 2: S3-S9.
- Thomas JO, Herrero R, Omigbodun AA, Ojeakinde K, Ajayi IO, Fawole A, et al. Prevalence of human papilloma virus infection in women in Ibadan, Nigeria: A population-based study. Br J Cancer 2004; 90: 638-645.
- Human Papilloma Virus and Related Diseases Report-Nigeria. WHO/ICO Information Centre on HPV and Cancer 2014. Available at www.hpvcentr.net Assessed on 15/03/2014.
- De Lemos PAP, Garcia-Zapata MTA, Tavares SBN. Cervical cytopathology in a population of HIV-positive and HIV-negative women. Journal of Tropical Medicine 2012; Article ID869758.
- Nweke IG, Nwadike VU, Kalu IE, Ojide KC. Human papilloma virus and cervical neoplasiain HIV positive women: A non-systematic review. African Journal of Microbiology Research 2014; 822: 2193-2201.
- Getinet M, Gelaw B, Sisay A, Mahmoud EA, Assefa A. Prevalence and predictors of Pap smear cervical epithelial cell abnormality among HIV-positive and negative women attending gynaecologicalexamination in cervical cancer screening centre at DebreMarkos referral hospital, East Gojjam, Northwest Ethiopia. BMC Clinical Pathology 2015; 15: 16.
- Mbu ER, Kongnyuy EJ, Mbopi-Keou FX, Tonye RN, Nana PN, Leke RJI. Gynaecological morbidity among HIV positive pregnant women in Cameroon. Reproductive Health 2008; 51:3.
- Moodely M, Garib R. The significance of human papillomavirus infection detected by cervical cytology among women infected with the human immunodeficiency virus. JObstetGynaecol2004; 248: 903-906.
- Bassey G, Jeremiah I, Ikimalo JI, Fiebai PO, Athanasius BP. Abnormal cervical cytology among HIV-positive women in Nigeria. Int J GynaecolObstet 2014; 1252:103-106.
- Morten F, Bigger RJ, Goedert JJ. Human papillomavirus associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. J Natl Cancer Inst 2000; 9218: 1500-1510.
- Firnhaber C, Zungu K, Levin S, Michelow P, Montaner LJ, Macphail P, et al. Diverse and high prevalence of human papillomavirus associated with a significant high rate of cervical dysplasia in human immunodeficiency virus women in Johannesburg, South Africa. ActaCytol 2009; 531: 10-17.
- Keller MJ, Burk RD, Xie X, Anastos K, Massad LS, Minkoff H, et al. Risk of cervical precancer and cancer among HIV-infected women with normal cervical cytology and no evidence of oncogenic HPV infection. JAMA 2012; 3084: 362-369.
- Dim CC, Ezegwui HU, Ikeme AC, Nwagha UI, Onyedum CC. Prevalence of cervical squamous intraepithelial lesions among HIV-positive women in Enugu, South-Eastern Nigeria. J ObstetGynaecol 2011; 31: 759-762.
- Anorlu RI, Igwilo CI, Akanmu AS, Banjo AA, Odunukwe NN, Okany CC, et al. Prevalence of abnormal cervical smears among patients with HIV in Lagos, Nigeria. West Afr J Med 2007; 26: 143-147.
- Chama CM, Ngadda H, Gashua W. Cervical dysplasia in HIV infected women in Maiduguri, Nigeria. J ObstetGynaecol 2005; 253: 286-288.
- Parham GP, Sahasrabuddhe VV, Mwanahamuntu MH, Shepherd BE, Hicks ML, Stringer EM, et al. Prevalence and predictors of squamous intra-epithelial lesions of the cervix in HIV- infected women in Lusaka, Zambia. GynecolOncol 2006; 1033: 1017-1022.
- PA, Thacher TD, Ekwempu CC, Idoko JA. Cervical dysplasia in Nigerian women infected with HIV. Int J GynaecolObstet 2009; 1072:99-102.
- Swende TZ, Ngwan SD, Swende LT. Prevalence and risk factors for cervical squamous intraepithelial lesions among women infected with HIV-1 in Makurdi, Nigeria. Int J Women’s Health 2012; 4:55-60.
- Kreiss JK, Kiviat NB, Plummer FA, Roberts PL, Waiyaki P, Ngugi E, et al. Human Immunodeficiency virus, human papillomavirus, and cervical intraepithelial neoplasia in Nairobi prostitutes. Sex Transm Dis 1992; 191: 54-59.
- Palesfsky JM. Human papillomavirus infection and anogenitalneoplasia in human immunodeficiency virus-specific men and women. J Natl Cancer Inst Monographs 1998; 15-20.
- De Sanjose S, Palesfky J. Cervical and anal HPV infections in HIV positive women and men. Virus Research 2002; 89: 201-211.
- SOGC Clinical Practice Guidelines no. 196, 2007. Consensus Guidelines on Human Papillomavirus. Journal of Obstetrics and Gynaecology of Canada 2007; 298: S1-S56.
- Bratcher LF, Sahararabuddhe VV. The impact of antiretroviral therapy on HPV and cervical intraepithelial neoplasia: current evidence and directions for future research. Infect Agent Cancer 2010; 5:8-20.
- Moodley JR, Constant D, Hoffman M, Salimo A, Allan B, Rybicki E, et al. Human papillomavirus prevalence, viral load and precancerous lesions of the cervix in women initiating highly active antiretroviral therapy in South Africa: a cross-sectional study. BMC Cancer 2009; 9: 275-285.
- ParamsothyP, Jamienson DJ, Heilig CM,Schuman PC, Klien RS, Shah KV, et al. The effect of highly active antiretroviral therapy on human papillomavirus clearance and cervical cytology. ObstetGynaecol 2009; 1131: 26-31.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.