Cervicogenic Headache: Diagnostic Evaluation and Outcomes of Various Physiotherapy Modes
Received: 07-Mar-2022, Manuscript No. AMHSR-22-52608; Editor assigned: 09-Mar-2022, Pre QC No. AMHSR-22-52608(PQ); Accepted Date: Apr 05, 2022 ; Reviewed: 25-Mar-2022 QC No. AMHSR-22-52608; Revised: 31-Mar-2022, Manuscript No. AMHSR-22-52608(R); Published: 05-Apr-2022, DOI: 10.54608.annalsmedical.2022.33
Citation: A, et al. Cervicogenic Headache: Diagnostic Evaluation and Outcomes of Various Physiotherapy Modes. Ann Med Health Sci Res. 2022;12:112-117.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Cervicogenic Headache (CGH) refers to any headache that arises from the cervical spine dysfunction. It is not a single disease; basically, it is a syndrome that characterized by chronic unilateral pain resulting from any disorder may be related to bony structure, soft tissue or any other structures that lie within or surround the joints. Cervicogenic headache is a type of referred pain that triggered by fatigue, bad posture or any other previous or current injury to cervical spine. Common patients are young, active and females are affected more than males. Objectives: To determine the Diagnostic evaluation of cervicogenic headache using a series of cases and compare the outcomes of treatment with various physiotherapy modalities/techniques. Methodology: Samples of 200 patients of cervicogenic headache were taken from physiotherapy department of fatima memorial hospital Lahore, using convenience non-probability sampling technique of data collection using clinical criteria; unilateral headache without side-shift, neck pain spreading to the fronto-ocular area and flexion-rotation test was performed. For pain severity NPRS was used. Results: All the 200 patients with an average age of 40 years (range 20 years-60 years) were diagnosed with cervicogenic headache and were managed with different modalities and therapeutic exercises. The clinical examination at the end of total treatment session (4 weeks) revealed; maximum patients (85%) had been improved after the physiotherapy treatment. Conclusions: Cervicogenic headache is a pathology arising from cervical spine at C2-C4 level as a result of biomechanical or pathophysiological factors and commonly affect the young active adults. Therapist relief the patient symptom by using different modalities, gentle motion and therapeutics exercises. A period of 4 weeks is usually adequate for resolution of symptoms. Successful long-term outcomes can be achieved with a comprehensive exercise program.
Keywords
Cervicogenic headache; Evaluation; Physiotherapy
Introduction
Cervicogenic headache also known as cephalalgia or cervical headache or neck related headache is a condition in which the head pain is originated from the neck. [1] The pain of cervicogenic headache is referred to head from soft tissue, bones and nerves, joint or vascular structures that are present in neck. [2] CGH primarily originate from musculoskeletal dysfunction in upper three segments of cervical spine. Cervical spinal neuron C1,C2,C3 converge with adjacent spinal fibers responsible for referred pain to occipital region of head and convergence between cervical and trigeminal fibers responsible for spreading the pain into the other areas of head and neck. [3]
It is one of the most common types of headaches that have a high prevalence rate among general population. It usually affects all age groups but it may commonly occur at ages between 20 years-60 years. CGH is more common among female than males. [4] Based on medical criteria cervicogenic headache usually accounts for 15%-20% of all types of headaches. [5]
International classification of headache disorders published by IHS, classify the headaches into two basic categories i.e. primary and secondary headaches. Primary headaches are those that have some definite cause like vascular or muscular abnormalities. Primary headaches include migraine or tension-type headaches and others. Secondary headaches are those headaches that have some other sources like head or neck injury, any degenerative disease and, inflammation etc. According to this classification cervicogenic headache is considered as “secondary headache”. [6]
The exact etiology is still not understood but some factors are considered to be associated with CGH like any traumatic injury (e.g. whiplash injury or heavy lifting), [7] repetitive working activities with poor biomechanics, any degenerative disc problem and other factors include stress and disturbed sleeping patterns.
Cervicogenic headache is usually presented by chronic unilateral headache that starts from one side of back of head and neck and then moves forward to the frontal and parietal areas of head. This headache is worsened by applying pressure on neck or by certain neck movements. Initially pain is intermittent in character but as times passes, pain becomes continuous and the intensity of pain also fluctuates. Pain may spread to ipsilateral shoulder and arm, [8] other symptoms include limitation of neck ROM, neck stiffness, and tenderness. Like migraine, cervicogenic headache may experience with photophobia, irritability, nausea but these are less occurring as that of migraine. [9,10]
IHS has designed diagnostic criteria for CGHs, it is summarized as; chronic unilateral headache, moderate pain that is non-throbbing in nature, headache that worsens by neck movement and prolong postures, limitation of range of motion of neck or tenderness, numbness and tingling sensations in arm, and others include photophobia, irritability, GIT disturbance. But its characteristics occasionally may be difficult to differentiate it from primary types of headaches like migraine and tension type headache.
Physical assessment of cervicogenic headache involves postural assessment, active range of motion measurement by goniometer, muscle strength by manual muscle testing, neck flexion and rotation test. Forward head posture is commonly seen in patient with cervicogenic headache. [11]
Active range of motion measured by goniometer is found to be decrease CGH. [12] Decrease muscle strength of cervical muscle especially neck flexors in CGH when done by manual muscle testing. [13] Neck flexion and rotation test performed, in this test the examiner flexes the neck of patient in order to fix the lower cervical segment and then passively rotate the neck at atlanto-axial joint. Limitation of ROM occurs in symptomatic side. [14]
Interventional diagnosis is another very strong indicator for CGH. In this technique, 3rd occipital nerve that supply the zygapophysial joint between C2 and C3 is block by injecting an anesthetic medicine. Complete relief from pain conform the cervicogenic headache. [10,15] Differential diagnosis is also done to confirm the CGH from other headaches. It is based principally on the pattern of presenting headache. Lab investigations are also useful to distinguish it from other systemic problems like RA, SLE etc. Other protocols used for diagnosis of CGHs include CT-Scan, MRI but these do not confirm the diagnosis. [16]
Cervicogenic headache may be managed by various methods including drugs (anti-inflammatory drugs like acetaminophen, analgesics, muscle relaxants in severe cases opioid may be considered), injection (local anesthetics, steroids), [17] physiotherapy , spinal manipulation performed by chiropractor, radiofrequency neurotomy (the procedure involve placing an electrode near the 3rd occipital nerve where it crosses the zygapophysial joint between C2 and C3. The electrode disrupts the nerve and complete pain relief achieved), relaxation techniques and spinal surgery which is the last option for CGHs.
Physiotherapy treats CGH by using different modalities like ice packs, hot packs and ultrasound etc. to reduce pain and spasm. Manual techniques include cervical traction to reduce nerve compression, stretching to lengthen the tight structures, strengthening to develop power in weak muscles and posture correction. Most of the patients completely recover from this condition by appropriate physical therapy treatment but recovery time may vary according to the patient’s health status.
Methodology
It was a descriptive case series study design. The data was collected from Fatima memorial hospital Lahore, Pakistan for the duration of 4 months. Sample size was calculated by using Rao software and 200 cases of cervicogenic headache were taken. The cases giving positive signs and symptoms of acute and chronic nature will be selected from the FMH department of orthopedic and physiotherapy, diagnosed by physiotherapist and orthopedics on the basis of clinical and other investigation. Data collected using clinical criteria; unilateral headache without side-shift, neck pain spreading to the fronto-ocular area and flexion-rotation test was performed. For pain severity NPRS (Numeric Pain Rating Scale) was used. An informed consent was obtained from the patients for including their data in study. They were informed about the procedure which is likely to be undertaken as the situation demand. A detailed socio-demographic data was obtained inquiring their habits and life style [Figure 1].
A history of onset of problem was obtained to assess the possible etiology. The symptoms, severity and duration were enquired; patient was examined for eliciting signs of cervicogenic headache. They were investigated by routine and special investigations to list the positive pathology. Measuring tools used for pain is Numeric pain rating scale (NPRS), goniometer was used to assess the range of motion of cervical spine and to confirm the diagnosis flexion and rotation test was performed. After the cervicogenic headache has been diagnosed patient was managed by different modalities that include hot pack, ultrasound and Transcutaneous Electrical Nerve Stimulation (TENS) and different therapeutic techniques were used for 4 weeks of follow up [Figure 2].
Different physical therapy modes were applied;
- Mode 1 consists of cervical traction, muscle stretching, and muscle strengthening.
- Mode 2 consists of myo fascial release, muscle strengthening and cervical stabilization exercises.
- Mode 3 consists of muscle stretching, muscle strengthening and cervical stabilization exercises.
In 200 patients, some patients receive mode 1 treatment, some received mode 2 and others were given mode 3.
Data Analysis
The data was analyzed through S.P.S.S version 20 descriptively. The socio-demographic data presented as frequency distribution Tables [1-5].The symptoms and signs listed and presented as proportions. Various physiotherapy modalities applied as felt appropriate, and their outcomes in the form of impairments or no impairment analyzed. Patterns of presentation of symptoms and diagnostic evaluation and outcome of individual modes of management and treatment were plotted in the frequency tables. The final outcome measures included, finding relative success and failure ratio by different approaches. Since it is a descriptive study, no test of significance applied.
| Sr. No. | Pain (severity) NPRS | Total n(%) | Duration | Total n(%) | Areas | Total n(%) |
|---|---|---|---|---|---|---|
| 1 | Mild | 16 (8%) | Intermittent | 80 (40%) | Occipital | 104 (52%) |
| 2 | Moderate | 144 (72%) | Continuous | 120 (60%) | Temporal | 56 (28%) |
| 3 | Severe | 40 (20%) | Total | 200 (100%) | Frontal | 40 (20%) |
| Total | 200 (100%) | Total | 200 (100%) | |||
| Mild: 1-4 NPRS Moderate: 5-7 NPRS Severe: 8+ NPRS | ||||||
Table 1: Distribution of cases by pain in head and neck (severity).
| Sr.No. | Vertigo Status | Total n (%) | Blurred vision | Total n (%) | Numbness status | Total n (%) |
|---|---|---|---|---|---|---|
| 1 | Present | 56 (28%) | Present | 56 (28%) | Present | 104 (52%) |
| 2 | Absent | 144 (72%) | Absent | 144 (72%) | Absent | 96 (48%) |
| Total | 200 (100%) | 200 (100%) | Total | 200 (100%) |
Table 2: Distribution of cases by status of vertigo, numbness and blurred vision.
| Sr.No. | Spasm | Total n (%) | Flexibility | Total n (%) |
|---|---|---|---|---|
| 1 | Moderate | 136 (68%) | Good | 120 (60%) |
| 2 | Severe | 64 (32%) | Fair | 80 (40%) |
| Total | 200 (100%) | Total | 200 (100%) |
Table 3: Distribution of cases by neck spasm and flexibility.
| Sr.No. | Exercises | Frequency | Percentage |
|---|---|---|---|
| 1 | Cervical traction+muscle stretching+muscle strengthening | 72 | 36% |
| 2 | Myofascial release+muscle strengthening+cervical stabilization exercises | 64 | 32% |
| 3 | Muscle stretching+muscle strengthening+cervical stabilization exercises | 64 | 32% |
| Total | 200 | 100% |
Table 4: Distribution of cases by application of therapeutic exercises.
| Sr.No. | Modalities | No. of cases n (%) | Pain relief n (%) | Spasm relief n (%) |
|---|---|---|---|---|
| 1 | Hot pack | 80 (40%) | 24 (30%) | 72 (90%) |
| 2 | TENS | 80 (40%) | 64 (80%) | - |
| 3 | Ultrasound | 40 (20%) | 8 (20%) | 24 (60%) |
Table 5: Distribution of cases by modalities outcomes.
Results
Among the cases 64% were females and 36% males. By age most patients 76% fell in age group ranged from 31 years to 50 years. One third of cases 24% were slightly higher in the younger age 20 years to 30 years of age. By occupation most females 63% were housewives and most males 77% were office worker. The numbers of cases in medical and teaching profession were equal 16% of each.
According to the severity of pain into mild, moderate and severe levels, it was found that majority of the patients had either moderate (72%) or severe (20%) level. Only 8% of cases had mild level of pain.
According the type of headache, majority of cases 60% gave the history of continuous type of pain and 40% gave the history of intermittent type of headache.
According to the distribution of pain in the head with respect to the area involved, most of the cases (52%) had pain in occipital region, 28% had pain in temporal region, and only 20% cases had pain in frontal region.
Regarding the status of vertigo, 100% of males were not having complained of vertigo while about 44% females were having complained of vertigo.
When history was taken about the presence or absence of blurred vision 28% of cases gave the history of blurred vision and 72% of cases were having no history of blurred vision. Regarding the status of numbness, 52% of cases have numbness and 48% have no history of it.
While assessing the severity of neck spasm into moderate and severe level, it was found that majority 68% had moderate and 32% of cases had severe level of spasm in neck.
While assessing the flexibility into good and fair level, it was found that majority of cases 60% were having a good flexibility in their neck muscles and 40% of cases were having enough flexibility.
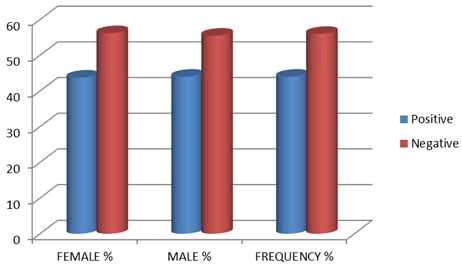
On physical examination, when flexion rotation test was performed, 44% of cases showed a positive result and 56% were show negative results.
According to the application of therapeutic exercises, 36% of patients had been treated with combination of cervical traction, muscle stretching, and muscle strengthening, 32% of patients had been treated with myofascial release, muscle strengthening and cervical stabilization exercises and 32% of patients had been treated with muscle stretching, muscle strengthening and cervical stabilization exercises.
By applying the hot pack pain relief was reported in 30% of cases and spasm relief was reported in 90% of cases. By the application of TENS pain relief was reported in 80% of cases and no spasm relief was found. By applying ultrasound pain relief was found in 20% of cases and spasm relief was reported in 60% of cases.
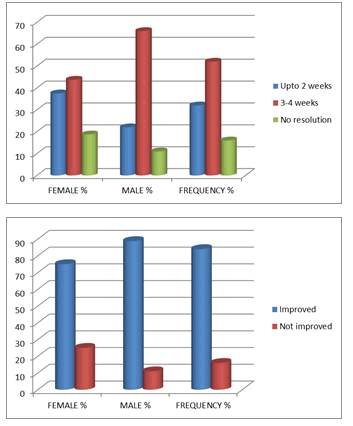
Regarding the time of resolution of symptoms after treatment it was found that majority 52% of cases showed their resolution of symptoms in the duration of 3 to 4 weeks. The resolution time for 32% of cases fell in less than 2 weeks. About 16% of cases were showed with no resolution of symptoms.
By final outcomes of patients, majority 84% of cases were improved, while only 16% of cases showed no improvement after physical therapy treatment.
Discussion
Cervicogenic headache is a syndrome. There are many causes of the pain, which may originate at various levels including the lower part of the neck. The clinical picture and diagnostic criteria for cervicogenic headache were accepted by the International Association for the Study of Pain (IASP).
The study was based on time duration of 6 months, in order to evaluate the cervicogenic headache and outcomes of its treatment. The data were taken from 200 individuals with cervicogenic headache. There were 72 males and 128 females. By age most patients 76% fell in age group ranged from 31 years-50 years showing that cervicogenic headache is more common in active adults. Among the patients interviewed female gender was higher than male. This incidence was more frequent in house-wives. Among males, incidence was higher in office worker. Pain in CGH is usually experienced unilaterally without side shift that can be aggravated by neck movement or sustained awkward posture. Cervicogenic headache is usually moderate, non-throbbing in nature that of varying duration or fluctuating or may be continuous type.
In present study when patients were enquired about the side of involvement of headache most of patient (84%) was having unilateral headache. Intensity of pain was mild in 8% of patient while it was moderate in 74% and was severe in 20% of cases. 60% of cases reported continuous type of pain.
Literature findings shows that associated manifestations of CGH, such as neck pain, focal neck tenderness, history of neck trauma, coexisting shoulder pain, nausea, vomiting, and photophobia are not unique to cervicogenic headache, the incidence of these clinical features was 4.5%-68.2%. [7] In this study the incidence of associated manifestation of CGH such that 52% of cases present with arm numbness, 28% presents with vertigo and blurred vision. Three forms of cervicogenic headaches can be distinguished; 52% of cases present with frontal headache, 28% present with temporal headache and 20% of cases present with occipital headache.
On examination more than 75% of patients present with forward head posture, 60% of patients present with normal range of motion at neck and show good flexibility in muscles surrounding the neck. More than 65% of cases present with muscle weakness that may contribute toward the cervicogenic headache. Flexion rotation test applied to diagnose CGH, 44% cases show negative results, and it is not a conformational test but may contribute in the diagnosis of CGH. Some researchers found that forward head posture may increase the stress on cervical region and reported significant decreases in active ROM in those with CGH, while in others have found no significant differences in AROM when compared to asymptomatic subjects. [14]
As numbness is present in majority of cases (52%) so cervical traction and muscle stretching were used for reducing the compression on the nerves. As the majority of patients in this study present with muscles weakness and neck spasm with moderate type of pain so combination of cervical muscles strengthening exercises and myofascial release along with TENS and hot pack were used.
Therapeutic exercise intervention should start by addressing and teaching postural awareness. Patients with cervical pain often exhibit forward head posture and rounded shoulders associated with muscle imbalance. Reinforcing good posture through regular cuing can help reinforce the stretching and strengthening exercises to restore muscle balance
Most patients are successfully treated by conservative means. The conservative treatment includes physiotherapy to address biomechanical issues, with cervical strengthening exercises; tight muscles stretching; and primarily focused on cervical stabilization exercises. A period of 2 weeks-4 weeks is usually adequate for resolution of symptoms.
In present study, 84% of patients showed the resolution of their symptoms within the ranges from 2 weeks-4 weeks and only 16 % of patients showed no resolution at all. By final outcome of the patients, majority (84%) of patients improved after the physical therapy treatment.
Conclusion
Cervicogenic headache is pathology that characterized by chronic headache that is referred to head from either bony structures or soft tissues present in the neck. The main diagnostic feature was unilateral headache moderate type, non-throbbing in nature that is aggravated by neck movement without side shift. It commonly affects the young active adults with the female gender prominent. Therapist relieves the patient symptoms by using different modalities, gentle motion and therapeutics exercises. A period of 2 weeks-4 weeks is usually adequate for resolution of symptoms. Successful long-term outcomes can be achieved with a comprehensive exercise program.
Limitation
The present study has several limitations. First, it is a retrospective review and secondly as the sampling method was non probability sampling so results can’t be generalized and its authenticity is debatable.
References
- Blumenfeld A, Siavoshi S. The challenges of cervicogenic headache. Curr Pain Headache Rep. 2018;22:1-5.
[Crossref], [Google Scholar], [Indexed]
- Fredriksen TA, Antonaci F, Sjaastad O. Cervicogenic headache: Too important to be left un-diagnosed. J Headache Pain. 2015;16:1-3.
[Crossref], [Google Scholar], [Indexed]
- Barmherzig R, Kingston W. Occipital neuralgia and cervicogenic headache: Diagnosis and management. Curr Neurol Neurosci Rep. 2019;19:1-8.
[Crossref], [Google Scholar], [Indexed]
- Biondi DM. Cervicogenic headache: A review of diagnostic and treatment strategies. J Am Osteopath Assoc. 2005;105:16-22.
[Crossref], [Google Scholar], [Indexed]
- Knackstedt H, Bansevicius D, Aaseth K, Grande RB, Lundqvist C, Russell MB. Cervicogenic headache in the general population: The Akershus study of chronic headache. 2010;30:1468-76.
[Crossref], [Google Scholar], [Indexed]
- Kim BK, Cho SJ, Kim BS, Sohn JH, Kim SK, Cha MJ, et al. Comprehensive application of the international classification of headache disorders third edition, beta version. J Korean Med Sci. 2016;31:106-13.
[Crossref], [Google Scholar], [Indexed]
- Antonaci F, Sjaastad O. Cervicogenic headache: A real headache. Curr Neurol Neurosci Rep. 2011;11:149-55.
[Crossref], [Google Scholar], [Indexed]
- Levin JH, Mellion M. Chronic daily headache: Challenges in treatment. R I Med J. 2015;98:22.
[Crossref], [Google Scholar], [Indexed]
- Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine. 2002;27:1835-43.
[Crossref], [Google Scholar], [Indexed]
- Hall T, Robinson K. The flexion-rotation test and active cervical mobility-a comparative measurement study in cervicogenic headache. Man Ther. 2004;9:197-202.
[Crossref], [Google Scholar], [Indexed]
- Ryu JH, Shim JH, Yeom JH, Shin WJ, Cho SY, Jeon WJ. Ultrasound-guided greater occipital nerve block with botulinum toxin for patients with chronic headache in the occipital area: A randomized controlled trial. Korean J Anesthesiol. 2019;72:479.
[Crossref], [Google Scholar], [Indexed]
- Lee JB, Park JY, Park J, Lim DJ, Kim SD, Chung HS. Clinical efficacy of radiofrequency cervical zygapophyseal neurotomy in patients with chronic cervicogenic headache. J Korean Med Sci. 2007;22:326-9.
[Crossref], [Google Scholar], [Indexed]
- Stovner L, Kolstad F, Helde G. Radiofrequency denervation of facet joints C2‐C6 in cervicogenic headache: A randomized, double‐blind, sham‐controlled study. Cephalalgia. 2004;24:821-30.
[Crossref], [Google Scholar], [Indexed]
- Espi LGV, Zurriaga LR, Monzani L, Falla D. The effect of manipulation plus massage therapy massage therapy alone in people with tension-type headache: A randomized controlled clinical trial. European journal of physical and rehabilitation medicine. 2016;52:606-17.
[Crossref], [Google Scholar], [Indexed]
- Jull G, Stanton W. Predictors of responsiveness to physiotherapy management of cervicogenic headache. Cephalalgia. 2005;25:101-8.
[Crossref], [Google Scholar], [Indexed]
- Goodman CC, Fuller KS. Goodman and Fuller's Pathology E-Book: Implications for the Physical Therapist. Elsevier Health Sciences. 5th 2020.
- Narouze SN, Casanova J, Mekhail N. The longitudinal effectiveness of lateral atlantoaxial intra-articular steroid injection in the treatment of cervicogenic headache. Pain Med. 2007;8:184-8.
[Crossref], [Google Scholar], [Indexed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.