Cesarean Delivery for a Life‑threatening Preterm Placental Abruption
- *Corresponding Author:
- Dr. Innocent I Okafor
Department of Obstetrics and Gynecology, Enugu State University of Science and Technology Teaching Hospital, Parklane, Enugu, Enugu State, Nigeria.
E-mail: okaforii@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Placental abruption is one of the major life‑threatening obstetric conditions. The fetomaternal outcome of a severe placental abruption depends largely on prompt maternal resuscitation and delivery. A case of severe preterm placental abruption with intrauterine fetal death. Following a failed induction of labor with a deteriorating maternal condition despite resuscitation, emergency cesarean delivery was offered with good maternal outcome. Cesarean delivery could avert further disease progression and possible maternal death in cases of severe preterm placental abruption where vaginal delivery is not imminent. However, further studies are necessary before this could be recommended for routine clinical practice.
Keywords
Cesarean delivery, Intrauterine fetal death, Preterm placental abruption
Introduction
Placental abruption is the premature separation of the normally implanted placenta after fetal viability and before the delivery of the baby. It is a significant cause of fetomaternal morbidity and mortality. The clinical diagnosis is based on a high index of suspicion, painful vaginal bleeding, uterine hypertonicity, and a nonreassuring fetal heart rate pattern or fetal death.
The condition complicates about 0.4–1.0% of pregnancies with 5.4% and 0.3% of it occurring at preterm and term gestations, respectively.[1-3] The perinatal mortality rate is approximately 12 times higher than in nonplacental abruption births.[4] The recurrence rate is about 4.4% following one previous history and 19–25% following two or more previous history.[5] The exact etiology is still unclear, however, associated risk factors include maternal hypertension, advanced maternal age, polyhydramnios, multiparity, abdominal trauma, intrauterine
growth restriction, intrauterine infection, premature rupture of membranes, threatened miscarriage, and cocaine abuse.[6] According to Sher and Statland, the degree of fetomaternal complications depends on the severity (grade) of the disease.[7] The most severe form is the Grade III disease, characterized by vaginal bleeding, uterine tenderness/tetany, fetal distress or intrauterine fetal death (IUFD), and maternal shock.[7] It is classified as Grade IIIa when there is no associated intravascular coagulation, and as Grade IIIb when there is associated intravascular coagulation.[8]
The fetomaternal outcomes of a severe placental abruption depend on the status of the fetus and mother, prompt maternal resuscitation, and delivery. We report a case of Grade IIIa preterm placental abruption to advocate early cesarean delivery to avert the disease progression to disseminated intravascular coagulation and other deadly complications.
Case Report
Mrs. A.U. was a 35-year-old Gravida 2, Para 1 +0 woman who is a known hypertensive patient since her last delivery in 2012. She booked for antenatal care in Semino Hospital and Maternity, Enugu at 11 weeks gestational age with a blood pressure of 160/100 mmHg. The ultrasound report confirmed a viable intrauterine pregnancy at 11 weeks plus 2 days. Other booking investigations were normal. She was commenced on tablets Aldomet 250 mg thrice daily and nifedipine 20 mg twice daily, but she did not adhere to her antihypertensive medications in spite of repeated counseling. The blood pressure remained uncontrolled and fluctuated between 150/100 mmHg and 160/110 mmHg despite increasing the dose of Aldomet to 500 mg 6 hourly. On November 11, 2014, at 29 weeks and 4 days gestational age, she was admitted as an emergency with severe abdominal pain, vomiting, and a pulse rate of 97 beats/min with blood pressure of 180/120 mmHg. The uterus was board-like, tender, and there was no fetal heart sound. The cervix was posterior, firm, and tubular. The cervical os was closed. Diagnoses of severe hypertension, preterm placental abruption, and IUFD were made. The packed cell volume was 30%, and there was no proteinuria. Her urgent bedside clothing time was 7 min. Her abdominal ultrasound confirmed IUFD but did not reveal any retro-placental blood clots. Resuscitation was commenced with intravenous infusion of normal saline, and the blood pressure was stabilized between 140/90 and 150/100 mmHg using intravenous hydralazine. Cervical ripening was commenced with 100 µg vaginal misoprostol at 4 hourly intervals; however, the cervix remained unfavorable for induction after 6 doses of administration. At about 36 h following admission, the patient complained of weakness, and dizziness. Her pulse rate was 128 beats/min, and the blood pressure was 90/60 mmHg. The cervix was still tubular, and the cervical os was closed. Her packed cell volume became 18%. The bedside clotting time which was done at regular intervals was noticed to have increased to 18 min. In view of the deteriorating clinical condition, she was counseled on the emergency cesarean section which she consented to. She was transfused with two units of fresh whole blood preoperatively. Following the transfusion, the pulse rate, blood pressure, and bedside clotting time became 107 beats/min, 110/70 mmHg, and 9 min, respectively.
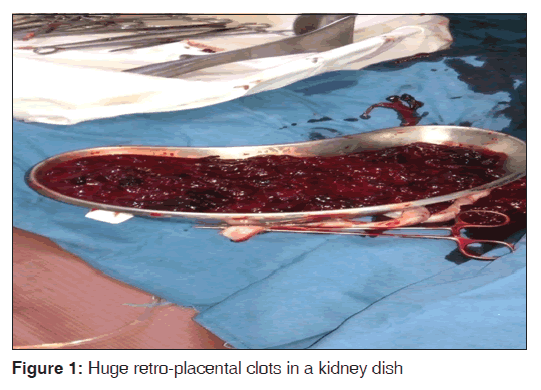
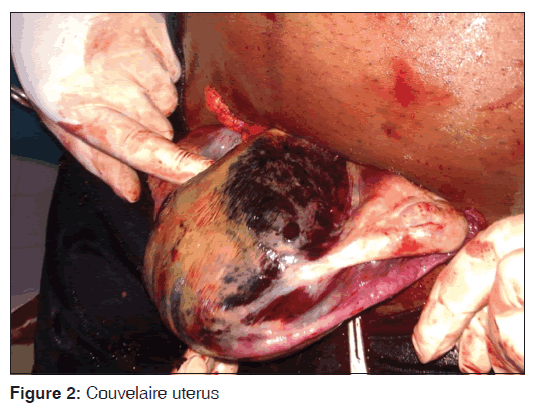
The intraoperative findings were a 1.25 kg female fresh stillbirth, postero-fundal placenta with about 1.5 L of retro-placental blood clots [Figure 1], and a Couvelaire uterus [Figure 2]. The fallopian tubes and ovaries were normal. She received one more unit of fresh whole blood intraoperatively. The postoperative recovery was satisfactory. The 3rd day post-operative packed cell volume was 25%. The blood pressure at discharge on the 6th postoperative day was 140/90 mmHg.
Discussion
Placental abruption is a serious maternal emergency that demands prompt resuscitation and immediate delivery to prevent further development of deadly complications that could result in maternal death.[8,9] The diagnosis of placental abruption is usually clinical, and features often include abdominal pain, vomiting, hypertension, board-like-tender uterus, and IUFD as seen in Mrs. A.U. It is usually confirmed at delivery by the presence of a huge retro-placental clots and a Couvelaire uterus.[10] Ultrasound scan often misses retro-placental clots[10] as observed in the case reported. This implies that ultrasound scan is not sensitive in diagnosing placental abruption as reported by previous authors.[10]
In cases where the fetus is alive and mature, cesarean delivery is no doubt the treatment of choice.[8] Grade IIIa preterm placental abruption with IUFD; however, poses a management dilemma when maternal life is threatened with shock and severe anemia while vaginal delivery is not imminent as seen in Mrs. A.U. Indecision and unnecessary delays in the induction of labor instead of performing cesarean section could worsen the maternal condition as in the case reported.[9] However, the swift resuscitation and prompt resort to cesarean delivery no doubt averted further progression of her disease condition.
Conclusion
Cesarean delivery could avert further disease progression and possible maternal death in cases of severe preterm placental abruption where vaginal delivery is not imminent. However, further studies are necessary before this could be recommended for routine clinical practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Pariente G, Wiznitzer A, Sergienko R, Mazor M, Holcberg G, Sheiner E. Placental abruption: Critical analysis of risk factors and perinatal outcomes. J Matern Fetal Neonatal Med 2011;24:698-702.
- Sheiner E, Shoham-Vardi I, Hadar A, Hallak M, Hackmon R, Mazor M. Incidence, obstetric risk factors and pregnancy outcome of preterm placental abruption: A retrospective analysis. J Matern Fetal Neonatal Med 2002;11:34-9.
- Sheiner E, Shoham-Vardi I, Hallak M, Hadar A, Gortzak-Uzan L, Katz M, et al. Placental abruption in term pregnancies: Clinical significance and obstetric risk factors. J Matern Fetal Neonatal Med 2003;13:45-9.
- Tikkanen M, Luukkaala T, Gissler M, Ritvanen A, Ylikorkala O, Paavonen J, et al. Decreasing perinatal mortality in placental abruption. Acta Obstet Gynecol Scand 2013;92:298-305.
- Tikkanen M. Etiology, clinical manifestations, and prediction of placental abruption. Acta Obstet Gynecol Scand 2010;89:732-40.
- Abu-Heija A, al-Chalabi H, el-Iloubani N. Abruptio placentae: Risk factors and perinatal outcome. J Obstet Gynaecol Res 1998;24:141-4.
- Sher G, Statland BE. Abruptio placentae with coagulopathy: A rational basis for management. Clin Obstet Gynecol 1985;28:15-23.
- Okonofua FE, Olatunbosun OA. Cesarean versus vaginal delivery in abruptio placentae associated with live fetuses. Int J Gynaecol Obstet 1985;23:471-4.
- Page EW, King EB, Merrill JA. Abruptio placentae; dangers of delay in delivery. Obstet Gynecol 1954;3:385-93.
- Nyberg DA, Cyr DR, Mack LA, Wilson DA, Shuman WP. Sonographic spectrum of placental abruption. AJR Am J Roentgenol 1987;148:161-4.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.