Chronic Cutaneous Draining Sinus of Dental Origin
- *Corresponding Author:
- Dr. Neha Sisodia
Department of Dentistry, PGIMER and Dr. RML Hospital, New Delhi - 110 001, India.
E-mail: nehasisodia86@gmail.com
Citation: Sisodia N, Manjunath MK. Chronic cutaneous draining sinus of dental origin. Ann Med Health Sci Res 2014;4:962-4.
Abstract
Extra oral sinus of odontogenic origin occurs when the purulent by‑products of dental pulp necrosis spread along the path of least resistance from the root apex to the skin on the face. Patients presenting with cutaneous sinus usually visit a general physician or dermatologist first, as the lesion can mimic various dermatologic pathologies, ranging from an infected sebaceous cysts to a basal cell carcinoma. Despite systemic antibiotics, symptoms often persist causing further confusion, and at times leading to unnecessary surgical interventions. The location of this sinus in the head and neck region should lead the physician to seek a dental opinion in order to avoid misdiagnosis.
Keywords
Dental fistula, Localized drug delivery, Root canal treatment
Introduction
A fistula is an abnormal connection between an organ, vessel, or another structure. Fistulas are usually the result of injury or surgery. It can also result from infection or inflammation. The root canal of a necrotic tooth is a source of predominantly anaerobic microbes. The tooth may present without any symptoms, except a cutaneous draining sinus.[1] Due to the extra-oral location of the sinus, patients tend to seek medical care first. These cutaneous lesions do not always arise close to the infected tooth, following the path of least resistance. The sinus tracts appear most commonly on the chin or jaw line, but they have been reported to occur as far away from the oral cavity as the chest.[2] Its similarity of presentation to various dermatologic conditions such as sebaceous cyst, coupled with the absence of dental signs and symptoms leads to antibiotic therapy as the first line of treatment. These symptoms however are refractory to such measures and require dental therapy for their permanent resolution.[3]
Case Report
A 20-year-old male patient had reported to the dental outpatient department with the chief complaint of intermittent pus discharge at the base of the chin since last 4 years. No relevant medical history was reported. He denied the presence of any tooth pain or swelling. A history of trauma while playing cricket 4–5 years back was elicited. The cutaneous draining sinus appeared 1 year after the accident. Fearing that he may be suffering from cancer, the patient went to a medical practitioner near his house. He had subsequently received multiple courses of oral antibiotics, but that did not provide long term relief. The ulcer-like lesion kept recurring at frequent intervals. Continuous foul smelling discharge led the patient to visit a dermatologist and an otorhinolaryngologist (ENT) specialist before being referred to the dental unit.
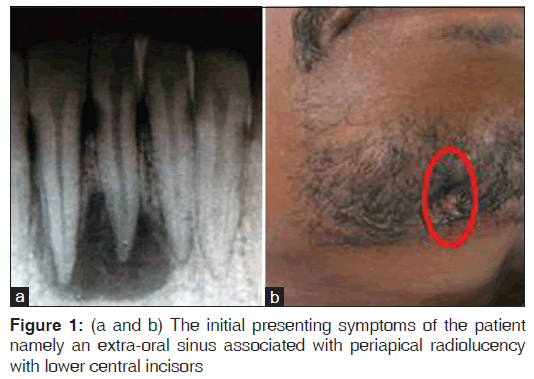
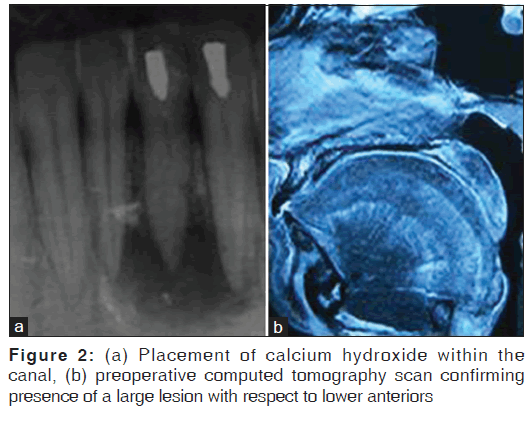
Extra-oral examination had revealed a cutaneous sinus about 1 cm in diameter along the chin, with a red halo at the margins [Figure 1b]. Palpation elicited purulent exudate. On detailed intraoral examination, no abnormalities like swelling or carious teeth were noted. Pulp vitality tests were negative for lower right central and lateral incisors. Intra-oral periapical radiograph revealed a large well defined unilocular, periapical lesion measuring around 3 cm by 2 cm in relation to these teeth. The well-defined margins of the lesion indicated a chronic-longstanding lesion such as a periapical cyst. A computed tomography (CT) scan was done, which displayed a radiolucency involving the cortical bone [Figures 1a and 2b].
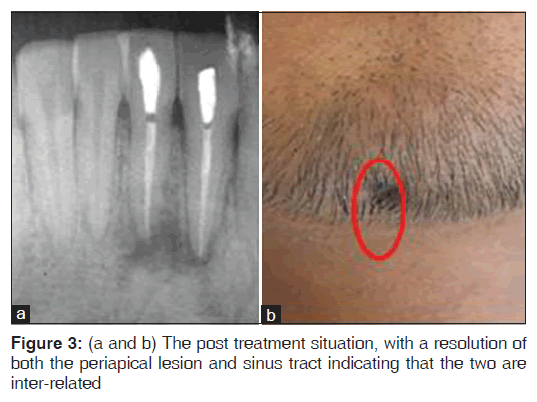
Root canal treatment was initiated for the teeth in question. Mild exudate drained through the canal was sent to the microbiology department for bacterial culture and antibiotic sensitivity testing. Thorough cleaning and shaping of the canal was done, and calcium hydroxide (Metapex, Chungcheongbuk-do, Korea) was placed within the root canal as an intracanal medicament (ICM).On 2 weeks recall, cutaneous sinus had stopped draining. Calcium hydroxide [Figure 2a] was removed, and an antibiotic paste was placed as intra-canal medicament (paste of ciprofloxacin 500 mg and metronidazole 400 mg−1:1 ratio) based on sensitivity testing of microbes within the pus sample.[4,5] Patient was recalled after 8 weeks, radiograph showed progressive reduction in the size of the lesion and rearrangement of bony trabeculae [Figure 2a] extraoral sinus had resolved considerably. Root canal treatment was completed [Figure 3a and b]. The patient was recalled at 6, 12 months for check-up. At each visit no recurrence of symptoms was reported, radiolucency grew progressively smaller, and adjacent teeth gave a positive response to sensibility testing.
Discussion
Cutaneous draining odontogenic sinus tracts can present a diagnostic challenge, as teeth are usually asymptomatic, and lesion can resemble common dermatological pathologies. Patient may reveal the history of trauma to the face some years ago. This injury could lead to dental pulp necrosis. Early radiographs, vitality testing of teeth can allow for detection of the culprit tooth. A panoramic or periapical radiograph will show radiolucency at apex of the infected tooth. Gutta percha can be used to trace the sinus tract to its origin, which is usually a non-vital tooth. A CT or CBCT are not ordinarily required, but it does help the clinician to understand the three-dimensional position of the lesion in relation to various anatomic structures. This provides invaluable help in recalcitrant cases where surgery may be required.
Once the diagnosis is made, non-surgical root canal treatment should be the first line of treatment. Successful outcome of root canal depends on the elimination of microorganism within the root canal system. Dentine which is tubular in nature may act as a safe haven for microorganism from which reinfection may occur, therefore, irrigants, and ICMs should be chosen keeping the target microbe in mind. In this case a combination of intra-canal irrigants was selected. Hypochlorite allows for removal of organic debris, while chlorhexidine shows substantivity and action against even Enterococcus. Calcium hydroxide, which is strongly alkaline, is popularly used as it raises the intracanal pH killing most of the intracanal microbes.[6]
Long-term use of antibiotics, (at times even anti-tubercular therapy) may make these organisms more resistant to conventional endodontics, hence selection of a suitable ICM must be done with care. In this study, local application of ICM of the mixture of antibiotics was implemented. Metronidazole was selected as the first choice drug as it is selectively toxic to anaerobic microorganisms and can penetrate deep within dentin. Ciprofloxacin exhibits very potent activity against Gram-negative bacteria, but very limited activity against Gram-positive bacteria. Tetracyclines were excluded from the preparation as antibiotic susceptibility isolated enterococcus strain which were resistant to it. Most primary endodontic lesions heal completely following non-surgical root canal therapy, rarely some resistant Gram-positive microbes may require additional surgical intervention.[7]
Lesion sterilization and tissue repair, refers to use of a combination of antibiotics to promote healing of the pulp,peri-radicular tissue and bone due to their synergistic action.[8] This approach may help reduce chances of even resistant microbes surviving as a combination of antibiotics is used. It has also been shown to be a great success in management of large periapical lesions and promoting regeneration of lost tissue by providing antimicrobials at the foci of infection.[9]
References
- Sammut S, Malden N, Lopes V. Facial cutaneous sinuses of dental origin‑a diagnostic challenge. Br Dent J 2013;215:555‑8.
- Donohue WB, Maisonneuve C. Sinus tracts of odontogenic origin in the face and neck. J Can Dent Assoc 1984;50:99‑102.
- Satish Kumar K, Subbiya A, Vivekanandhan P, Prakash V, Tamilselvi R. Management of an endodontic infection with an extra oral sinus tract in a single visit: A case report. J Clin Diagn Res 2013;7:1247‑9.
- Taneja S, Kumari M, Parkash H. Nonsurgical healing of large periradicular lesions using a triple antibiotic paste: A case series. Contemp Clin Dent 2010;1:31‑5.
- Ozan U, Er K. Endodontic treatment of a large cyst‑like periradicular lesion using a combination of antibiotic drugs: A case report. J Endod 2005;31:898‑900.
- Peters LB, van Winkelhoff AJ, Buijs JF, Wesselink PR. Effects of instrumentation, irrigation and dressing with calcium hydroxide on infection in pulpless teeth with periapical bone lesions. Int Endod J 2002;35:13‑21.
- Torabinejad M, Walton RE. Endodontics: Principles and Practice. 4th ed. Elsevier Health Sciences, Sydney, Australia: 2009. p. 45.
- Hoshino E, Takushige T. LSTR 3Mix‑MP method‑better and efficient clinical procedures of lesion sterilization and tissue repair (LSTR) therapy. Dent Rev 1998;666:57‑106.
- Jung IY, Lee SJ, Hargreaves KM. Biologically based treatment of immature permanent teeth with pulpal necrosis: A case series. J Endod 2008;34:876‑87.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.