Clinical Profile of Celiac Disease: Patient Epidemiological Prospective
2 Gastroenterology Division, Department of Medicine, King Fahad Specialist Hospital, Qassim University, Saudi Arabia
3 Gastroenterology & Hepatology Division, Department of Medicine, Qassim University Medical City, Saudi Arabia
4 Researcher at Prince Abdullah Bin Khaled Coeliac Disease Research Chair, Saudi Arabia
Citation: Albrady A, et al. Clinical Profile of Celiac Disease: Patient Epidemiological Prospective. Ann Med Health Sci Res. 2018; 8: 78-82
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
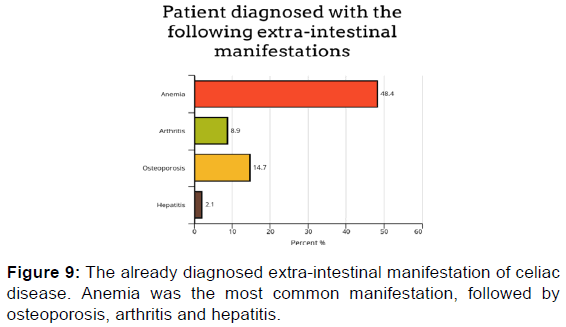
Objective: To explore the clinical profile (age of diagnosis, mode of presentations, and the diagnosis method) of celiac participants and to determine the incidence of the extra-intestinal manifestations. Methodology: A cross-sectional study of all participants diagnosed with celiac disease in the Kingdom of Saudi Arabia (KSA). An online questionnaire was sent to celiac disease participants via a well-known social media group. Responses were collected from 28 February 2017 until 8 July 2017. The target population of this study includes all celiac disease participants who live in KSA. To be representative, the required sample size was estimated as 384 responses. A study was conducted using an online questionnaire. Data were analyzed using google forms and SPSS. Results: Six-hundred-silty-nine responses were received. Most (56.2%) of the participants were between 18- and 50-years-old. Fifteen percent of participants had Diabetes mellitus type 1, and 13% have thyroiditis. The most common symptoms among the participants were abdominal pain (56%), weight loss (45.2%), and diarrhea (37.8%). Endoscopy was the most used mode of diagnosis in our cohort (81%). Almost half (48.4%) of the participants are anemic. We found that 47.2% of participants have joints pain, 8.9% have been diagnosed with arthritis and 14.8% have osteoporosis. Ten percent of the sample has increased liver enzymes, and 2% have been diagnosed with hepatitis. Conclusion: We found that the most common symptoms of celiac sufferers in KSA are abdominal pain, abdominal bloating, and weight loss. Almost half of the participants were anemic. Osteoporosis is the second most common extra-intestinal manifestation.
Keywords
Celiac disease; Extra-intestinal manifestation; Gluten free diet
Introduction
Celiac disease is an autoimmune disorder affecting genetically susceptible individuals, caused by the ingestion of glutencontaining grains (wheat, rye, and barley). [1] Celiac disease usually affects the digestive tract, which is classically associated with the presence of diarrhea, malabsorption, and weightloss. [2] The disease is highly prevalent around the world. For example, in North America, screening studies have shown that celiac disease is highly prevalent, occurring in almost 1% of the general population. [3,4] In Northern Sweden, a combined serological/endoscopic approach found a prevalence of almost 2%. [5] In Middle Eastern and North African countries, Celiac disease prevalence was believed to be low until the 1990s. However, with the introduction of serological testing for celiac disease, it is apparently more prevalent in these areas. [6] Recent studies suggest a high prevalence of celiac disease in Saudi Arabia. A study done in non-symptomatic participants from the eastern province reported a prevalence of 1%. Another study of the seroprevalence of celiac disease among healthy adolescents reported a prevalence of 2.2%. [7]
Although celiac disease usually affects the digestive tract, it is often accompanied by extra-intestinal manifestations, including anemia, osteoporosis, arthritis, and hepatitis. [8] Many studies Although celiac disease usually affects the digestive tract, it is often accompanied by extra-intestinal manifestations, including anemia, osteoporosis, arthritis, and hepatitis. [8] Many studies
Of the many forms of extra-intestinal manifestations of celiac disease, anemia is among the most prevalent, occurring in ~15% of adults with the disorder. [9,10] In contrast, a 2011 study reported that children (< 18-years-old) are less affected by celiac-disease associated anemia, totaling ~3% of individuals. [11] Participants who suffer from celiac disease also demonstrate varying levels of deficiencies in iron, folate, and vitamin B12, resulting in anemia.
A reduction in bone mineral density is a common extra-intestinal manifestation of celiac disease, affecting both children and adults. The exception, however, is for those who have been put on a gluten-free diet from a young age. [12] Conversely, a study conducted in the United States (US) found that celiac disease patients have an increased risk of bone fracture. [13]
Another study, in Argentina, found that an increased risk of bone fracture was associated only with those patients with typical celiac disease. [14] In a small-scale study conducted with participants diagnosed with celiac disease, ~10% were found to have osteopenia (reduced bone density) [10,12] although another study reported that 50% of the celiac disease patients had osteopenia. [15]
Contrary to what was previously thought, arthritis might be more common in patients with celiac disease. [16] A study conducted in 1985 identified a connection between seronegative arthritis and celiac disease. Patients with arthritis were observed and subsequently diagnosed with celiac disease. Following the diagnosis, patients were then put on a gluten-free diet, which resulted in a considerable improvement of arthritic pain. [17] Bone scintigraphy identified sacroiliitis in 60% of adult celiac patients. [18] Two studies involving 200 celiac patients and a control group showed that, of the 200 celiac disease sufferers, 26% had arthritis, whereas only 7.5% of the control group had arthritis. [19]
Several studies have shown that about 10% of participants who exhibit inexplicable elevations in alanine transaminase (ALT) or aspartate transaminase (AST) levels have celiac disease. [20,21] When participants are first diagnosed with celiac disease, approximately half of them have elevated levels of liver enzymes. [22-27] Although elevated liver enzymes are considered to be mostly subclinical, this can, however, develop into cirrhosis and liver failure. [28]
Epidemiological research shows that celiac participants are two to six times more likely to develop liver disease in the future, and up to eight times more likely to be at risk of death from liver cirrhosis. [26,29] The cause of liver-related injuries due to celiac disease is unclear. Compared with non-celiac participants, celiac participants are at greater risk of also having autoimmune liver diseases, such as autoimmune hepatitis and primary biliary cirrhosis. [30] Even so, approximately 75% of celiac participants with increased liver enzymes had good outcomes after following a gluten-free diet. [27]
Objectives
• To explore the clinical and epidemiological profile of celiac disease sufferers, including the age of diagnosis, mode of presentations, and the method of diagnosis.
• To determine the incidence of common extra-intestinal manifestations of celiac sufferers.
Methodology
This cross-sectional study included participants diagnosed with celiac disease in Saudi Arabia. An online questionnaire was designed to address our goals. The questionnaire was sent via patient advocacy WhatsApp groups. Responses were collected from 28 February 2017 until 8 July 2017. The target population of this study includes all celiac disease participants who live in Saudi Arabia, and no exclusion criteria were set. There is no published data for the number of celiac disease participants in Saudi Arabia, but there are some studies suggesting a prevalence of 1–3%, [7,31] corresponding to ~620,000 (2% of the Saudi population). To be representative, the required sample size was estimated as 384 responses. The study was conducted using a bespoke, structured online questionnaire. The questionnaire is in Arabic, and simple wording was used to make it easier for participants to understand. The data were analyzed using Statistical Package of Social Science (SPSS 20 for windows evaluation version). Also, ?2 tests were used for categorical variables and the Mann-Whitney U-test for continuous variables; P-values < 0.05 were considered statistically significant. The data were initially identified and coded on an Excel spreadsheet using a unique identification number. The data were stored on a password-protected laptop with principle investigator and co-investigator, and were maintained confidentially. Only the research team had access to the database for analysis purposes. Here, we only present a summary of the statistics, and no identifying information is given. The participant names, used for determining their current health status, were kept as a separate database; so that these cannot be linked with any medical data.
Results
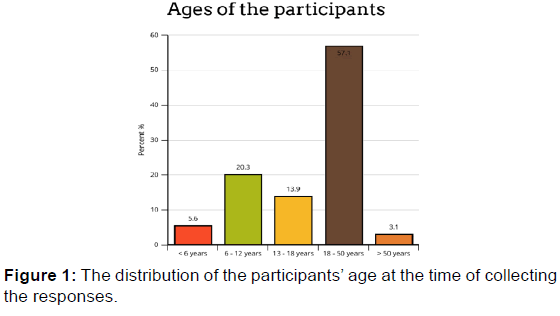
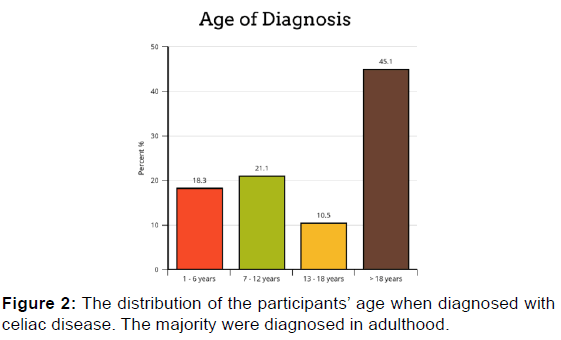
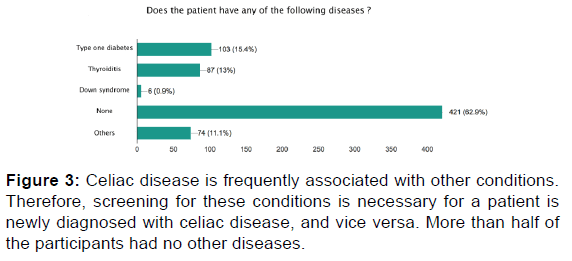
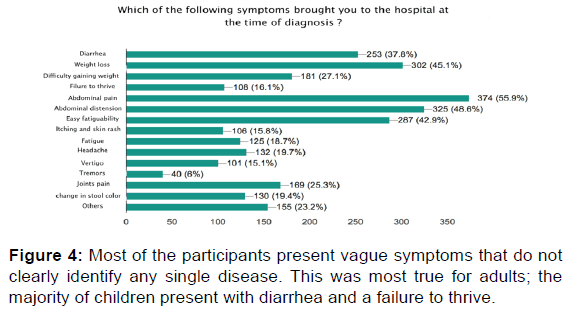
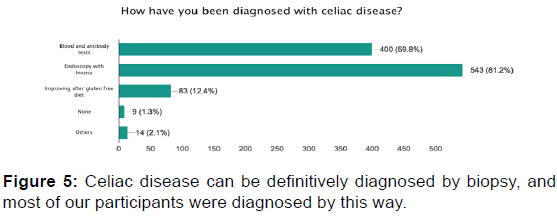
Six-hundred-sixty-nine responses were received from 775 sent questionnaires. The participants were mostly from Riyadh (47.8%), followed by Qassim (10.3%). The female to male ratio was (3:1). Most (56.2%) of the participants were between 18- and 50-years-old; 21.1% of the participants were between 6- and 12-years-old. Among our participants, 18.3% were diagnosed when between 1- and 6-years-old, 21.1% between 7- and 12-years-old, and 10.5% between 13- and 18-yearsold. Most of our participants have no other illnesses. Fifteen percent of participants have diabetes mellitus type 1, and 13% have thyroiditis. The most common symptom responsible for the participants seeking medical help was abdominal pain (56%), followed by abdominal distension and the feeling of gas accumulation in the abdomen (48.7%), weight loss (45.2%), easy fatigability (42.8%), diarrhea (37.8%), and difficulty in gaining weight (27%). The most used procedures for diagnosis of our participants were endoscopy and biopsy.
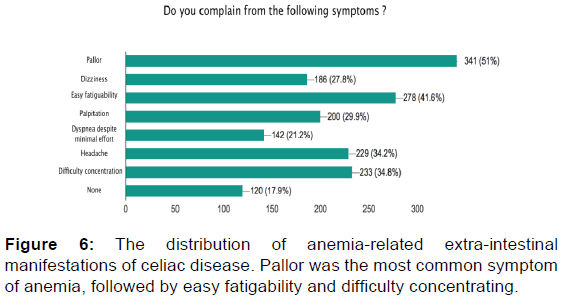
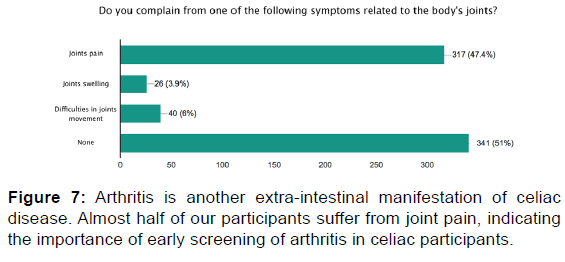
Regarding extraintestinal manifestations, we found that 48.4% of the celiac disease participants in our study complain of anemia. Many of the participants have pallor (50.8%) and complain of dizziness (27.7%). Among the questions related to joints symptoms, we found that almost half (47.2%) of our participants have joint pain, and 3.9% have joint swelling, but only 9% are diagnosed with arthritis. Approximately one-third (33%) of the sample suffer from bone pain and lower back pain, and only 4.3% stated that they have a bone fracture with minor trauma, while 14.8% have been diagnosed with osteoporosis.
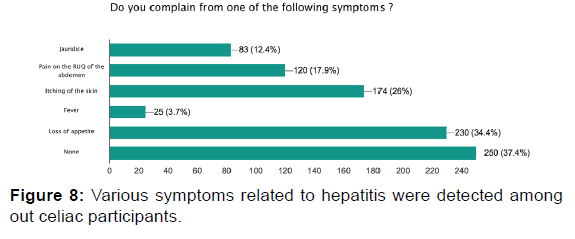
Among our participants, 12.4% have yellowish discoloration in the eyes (jaundice), and 17.9% have pain in the right upper quadrant of the abdomen. Twenty-six percent of participants reported experiencing itching. When we asked the participants if they had previously been diagnosed with hepatitis, only 2.1% answered yes. More than half of the participants (57.1%) did not have a liver enzymes test. Ten percent of the total sample has increased liver enzyme levels, and 32.9% were within the normal range [Figures 1-9].
Discussion
We found that the most common age of diagnosis was between 7- and 12-years-old. However, 35% of our participants were diagnosed at 18-years-old. These findings indicate that celiac disease can develop at any age. This should be kept in mind as an important differential diagnosis for patients complaining of suggestive symptoms.
We found that abdominal pain was mostly responsible for the patient visiting the hospital. This symptom can indicate many possible diseases. For this reason, many participants with celiac disease present at a later age with subtle symptoms, and the diagnosis of celiac disease might be delayed. Since blood tests are not always accurate, especially in very young children, 81% of our participants were diagnosed by endoscopy and biopsy.
Among our participants, we found that type 1 diabetes mellitus was the disease most associated with celiac disease, which is in line with the findings of other studies. [32,33] It was not clear whether the diagnosis of diabetes preceded the diagnosis of celiac disease or vice versa. However, 28 (15.7%) participants mentioned that the diabetes was the presenting illness that required them to seek medical attention at the time of celiac disease diagnosis, followed by thyroiditis (13%). Based on these findings, we recommend screening for celiac disease in diabetic and thyroiditis patients.
Anemia was the most common extra-intestinal manifestation, being diagnosed in around half of the participants and was the presenting illness in 27 of the participants. Of these 27 participants, 22 were adult female participants, suggesting a higher incidence in this group, which is in line with the findings of a previous study. [34]
Both celiac disease and inflammatory arthritis disease are autoimmune phenomena. Although the majority of our participants complain of joint pain, few have been diagnosed with arthritis. This is likely because the majority of our cohort is less than 40-years-old; a longer follow-up period will likely lead to more diagnoses. Therefore, we recommend earlier rheumatology evaluation for celiac disease patients.
Liver abnormality is another extra-intestinal manifestation of celiac disease. The exact cause of liver abnormality in celiac disease remains unclear. Intestinal permeability is increased in celiac disease; which might enable the entry of inflammatory materials, toxins, and antigens to the portal circulation, thereby leading to liver damage. Less than half of our cohort underwent a liver function test, and 10% showed elevated liver enzymes. Other liver-related manifestations were reported. Two percent of the cohort were diagnosed with hepatitis, and 12% complained of jaundice.
Based on our findings, we recommend more careful evaluation of liver abnormalities in celiac disease participants.
Conclusion
Our cohort is the largest yet reported epidemiological study of celiac disease in Saudi Arabia. We report that the most common presenting symptoms of celiac participants in Saudi Arabia are abdominal pain, abdominal bloating, and weight loss. Diarrhea was ranked as the fifth most common symptom. Almost half of the participants were anemic. Osteoporosis is the second common extra-intestinal manifestation.
Acknowledgements
The project were financially supported by Prince Abdullah Bin Khaled Celiac Disease Research Chair, Vice Deanship of Research Chairs, King Saud University
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Sollid LM, McAdam SN, Molberg O, Quarsten H, Arentz-Hansen H, Louka AS, et al. Genes and environment in celiac disease. Acta Odontol Scand 2001; 59: 183-186.
- Hernandez L, Green PH. Extraintestinal manifestations of celiac disease. Curr Gastroenterol Rep 2006; 8: 383-389.
- Riddle MS, Murray JA, Porter CK. The incidence and risk of celiac disease in a healthy US adult population. Am J Gastroenterol 2012; 107: 1248-1255.
- Catassi C, Kryszak D, Bhatti B, Sturgeon C, Helzlsouer K, Clipp SL, et al. Natural history of celiac disease autoimmunity in a USA cohort followed since 1974. Ann Med 2010; 42: 530-538.
- Walker MM, Murray JA, Ronkainen J, Aro P, Storskrubb T, D’Amato M, et al. Detection of celiac disease and lymphocytic enteropathy by parallel serology and histopathology in a population-based study. Gastroenterology 2010; 139: 112-119.
- Rostami K, Malekzadeh R, Shahbazkhani B, Akbari MR, Catassi C. Coeliac disease in Middle Eastern countries: A challenge for the evolutionary history of this complex disorder? Dig Liver Dis 2004; 36: 694-697.
- Aljebreen AM, Almadi M, Alhammad A, Al-Faleh FZ, Aljebreen AM, Almadi MA, et al. Seroprevalence of celiac disease among healthy adolescents in Saudi Arabia. World J Gastroenterol 2013; 19: 2374-2378.
- Leffler DA, Green PHR, Fasano A. Extraintestinal manifestations of coeliac disease. Nat Rev Gastroenterol Hepatol 2015; 12: 561-571.
- Halfdanarson TR, Litzow MR, Murray JA. Hematologic manifestations of celiac disease. Blood 2007; 109: 412-421.
- Rampertab SD, Pooran N, Brar P, Singh P, Green PHR. Trends in the presentation of celiac disease. Am J Med 2006; 119.
- Reilly NR, Aguilar K, Hassid BG, Cheng J, Defelice AR, Kazlow P, et al. Celiac disease in normal-weight and overweight children: clinical features and growth outcomes following a gluten-free diet. J Pediatr Gastroenterol Nutr 2011; 53: 528-531.
- Bianchi ML, Bardella MT. Bone in celiac disease. Osteoporos Int 2008; 19: 1705-1716.
- Jafri MR, Nordstrom CW, Murray JA, Van Dyke CT, Dierkhising RA, Zinsmeister AR, et al. Long-term fracture risk in patients with celiac disease: A population-based study in Olmsted County, Minnesota. Dig Dis Sci 2008; 53: 964-971.
- Moreno ML, Vazquez H, Mazure R, Smecuol E, Niveloni S, Pedreira S, et al. Stratification of bone fracture risk in patients with celiac disease. Clin Gastroenterol Hepatol 2004; 2: 127-134.
- Volta U, Caio G, Stanghellini V, De Giorgio R. The changing clinical profile of celiac disease: a 15-year experience (1998-2012) in an Italian referral center. BMC Gastroenterol 2014; 14: 194.
- Ghozzi M, Sakly W, Mankaï A, Bouajina E, Bahri F, Nouira R, et al. Screening for celiac disease, by endomysial antibodies, in patients with unexplained articular manifestations. Rheumatol Int 2014; 34: 637-642.
- Bourne JT, Kumar P, Huskisson EC, Mageed R, Unsworth DJ, Wojtulewski JA. Arthritis and coeliac disease. Ann Rheum Dis 1985; 44: 592-598.
- Usai P, Boi MF, Piga M, Cacace E, Lai MA, Beccaris A, et al. Adult celiac-disease is frequently associated with sacroiliitis. Dig Dis Sci 1995; 40: 1906-1908.
- Lubrano E, Ciacci C, Ames PR, Mazzacca G, Oriente P, Scarpa R. The arthritis of coeliac disease: Prevalence and pattern in 200 adult patients. Br J Rheumatol 1996; 35: 1314-1318.
- George EK, Hertzberger-ten Cate R, Van Suijlekom-Smit LW, Von Blomberg BM, Stapel SO, Van Elburg RM, et al. Juvenile chronic arthritis and coeliac disease in the Netherlands. Clin Exp Rheumatol 1996; 14: 571-575.
- Bardella MT, Vecchi M, Conte D, Del Ninno E, Fraquelli M, Pacchetti S, et al. Chronic unexplained hypertransaminasemia may be caused by occult celiac disease. Hepatology 1999; 29: 654-657.
- Bardella MT, Fraquelli M, Quatrini M, Molteni N, Bianchi P, Conte D. Prevalence of hypertransaminasemia in adult celiac patients and effect of gluten-free diet. Hepatology 1995; 22: 833-836.
- Bonamico M. Hepatic damage in celiac disease in children. Minerva Pediatr 1986; 38: 959-962.
- Vajro P, Paolella G, Pisano P, Maggiore G. Hypertransaminasemia and coeliac disease. Aliment Pharmacol Ther 2012; 35: 202-203.
- Sainsbury A, Sanders DS, Ford AC. Meta-analysis: Coeliac disease and hypertransaminasaemia. Aliment Pharmacol Ther 2011; 34: 33-40.
- Ludvigsson JF, Elfström P, Broomé U, Ekbom A, Montgomery SM. Celiac disease and risk of liver disease: a general population-based study. Clin Gastroenterol Hepatol 2007; 5: 63-69.
- Castillo NE, Vanga RR, Theethira TG, Rubio-Tapia A, Murray JA, Villafuerte J, et al. Prevalence of abnormal liver function tests in celiac disease and the effect of a gluten-free diet in the US population. Am J Gastroenterol 2015; 110: 1216-1222.
- Kaukinen K, Halme L, Collin P, Färkkilä M, Mäki M, Vehmanen P, et al. Celiac disease in patients with severe liver disease: Gluten-free diet may reverse hepatic failure. Gastroenterology 2002; 122: 881-888.
- Peters U, Askling J, Gridley G, Ekbom A, Linet M. Causes of death in patients with celiac disease in a population-based Swedish cohort. Arch Intern Med 2003; 163: 1566-1572.
- Garud S, Leffler D, Dennis M, Edwards-George J, Saryan D, Sheth S, et al. Interaction between psychiatric and autoimmune disorders in coeliac disease patients in the Northeastern United States. Aliment Pharmacol Ther 2009; 29: 898-905.
- Al Hatlani MM. Prevalence of celiac disease among symptom-free children from the Eastern Province of Saudi Arabia. Saudi J Gastroenterol 2015; 21: 367-371.
- Honar N, Karamizadeh Z, Saki F. Prevalence of celiac disease in patients with type 1 diabetes mellitus in the south of Iran. Turk J Gastroenterol 2013; 24: 122-126.
- Elfström P, Sundström J, Ludvigsson JF. Systematic review with meta-analysis: associations between coeliac disease and type 1 diabetes. Aliment Pharmacol Ther 2014; 40: 1123-1132.
- Qari FA. Clinical presentation of adult celiac disease in Western Saudi Arabia. Saudi Med J 2002; 23: 1514-1517.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.