Comparative Analysis of Distinct Methods for Cosmetic Visual Management of Gingival Hyperpigmentation: A Clinical Study
2 Department of Conservative Dentistry and Endodontics, Gitam Dental College and Hospital, Visakhapatnam, India
3 Department of Oral Pathology, Gitam Dental College and Hospital, Visakhapatnam, India
Received: 29-Nov-2024, Manuscript No. amhsr-24-155801; Editor assigned: 02-Dec-2024, Pre QC No. amhsr-24-155801 (PQ); Reviewed: 16-Dec-2024 QC No. amhsr-24-155801; Revised: 23-Dec-2024, Manuscript No. amhsr-24-155801 (R); Published: 30-Dec-2024
Citation: Kodem T. Comparative Analysis of Distinct Methods for Cosmetic Visual Management of Gingival Hyperpigmentation: A Clinical Study. Ann Med Health Sci Res. 2024; S6: 1-4.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: The focus of this study was to assess the effects of gingival depigmentation using scalpels and electrosurgery. Gingival color alters a person's smile and affects esthetics.
Methods: The study employed scalpel surgical technique and electrocautery as therapy methods due to their ease of use and reduced recovery time. After surgery, the healing and recurrence of pigmentation were assessed. At each follow-up appointment, intraoral photos were taken to assess any repigmentation and to compare the improvement. The statistical analysis methods employed were unpaired t-test and one-way Analysis of Variance (ANOVA).
Results: Three months following surgery, there was a statistically significant decrease for both study approaches compared to baseline and there were no problems that resulted in discomfort, infection, bleeding, or scarring. In both treatment modalities, there were no indications of repigmentation at the 3-month follow-up. Cases were longitudinally monitored for recurrences of pigmentation.
Conclusion: The outcomes of the electrocautery and surgical methods for gingival depigmentation were satisfactory. Therefore, the surgical method continues to be the most straightforward and successful depigmentation method. Using both of the methods used in this investigation, there was no recurrence of gingival hyperpigmentation during the follow-up period.
Keywords
Depigmentation; Electrocautery; Gingival melanin hyperpigmentation; Scalpel
Introduction
Gingival pigmentation can appear on its own or in conjunction with other skin lesions. Oral pigmentation on the lip, tongue, palate, or buccal mucosa may accompany it. On the associated gingiva, gingival pigmentation may appear as isolated patches or as a widespread dispersion. Pigmentation can have a variety of origins; some are physiologic, while others are malignant and have a high death rate [1]. In periodontal practice, gingival depigmentation is frequently performed. The process is thought to be straightforward and noninvasive. It is assured to patients that they will heal quickly. It is commonly known that the key pigment responsible for the color variations observed in complexion is melanin [1].
Changes in the activity of melanocytes in the basal cell layer of the oral epithelium, rather than their quantity, are thought to be responsible for variations in the melanin pigmentation that is specifically observed in racial pigmentation; this is more common in dark-skinned people of all ethnic backgrounds. Furthermore, because melanin acts as a barrier against the toxic substances found in tobacco smoke, smoking is one of the most well-known causes of oral pigmentation in people with light and dark skin. The length and quantity of smoking are significant variables that typically have a direct impact on pigmentation intensity [2-4]. The gold standard for removing unwanted gingival pigmentation is still the traditional, straightforward method of using a scalpel [5]. It is simply carried out under basic local anesthesia and does not require expensive or specialized equipment. Using this method, a layer of the underlying connective tissue and the gingival epithelium are surgically removed. Secondary intended healing of the denuded tissues is likely to occur and it may be accompanied with unpleasant bleeding both during and after the treatment, as well as some discomfort and pain afterward [2,3].
Different techniques used for depigmentation
• Scalpel technique
• Cryosurgery
• Electro surgery
• Lasers: Neodymium-doped Yttrium Aluminum Garnet (Nd-YAG) laser, Er-YAG laser, Co2-laser
• Chemical methods using caustic agents (method not used nowadays)
• Method aimed at masking the pigmented gingival from less pigmented areas
• Free gingival graft [6].
• Acellular dermal matrix allograft [7].
As the repigmentation may begin as a result of migrating melanocytes from these sites, it has been proposed that the gingival tissue, including free gingiva and interdental papilla, be entirely cleaned of melanin to prevent repigmentation [8]. Furthermore, it has been acknowledged that exposure to ambient tobacco smoke and race may both enhance gingival pigmentation. These factors may also be linked to an increase in repigmentation after effective therapy. There is still much to learn about the management, principles and procedures related to gingival melanin pigmentation issues [2]. In this case study, two different treatment modalities scalpels and electrocautery are compared for their clinical efficacy in treating gingival hyperpigmentation in two arches. This case study examines gingival hyperpigmentation and compares the clinical effectiveness of electroacupuncture and scalpel in treating the problem in two arches.
Case Presentation
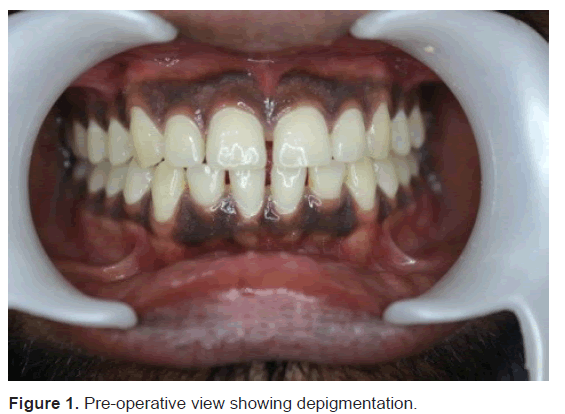
A male patient, age 25, came to the periodontics department with the chief complaint of "blackish gums." The patient's medical history was not relevant. Upon intraoral examination, the gingiva was found to have significant blackish pigmentation, but it was otherwise healthy and devoid of inflammation. The patient's aesthetic concerns were taken into consideration when discussing various possibilities with them and the treatment was scheduled once the institutional ethical committee gave its approval.
Procedure
The patient was informed of every step of the process and given written consent before electrosurgery was scheduled for the lower anterior region and scalpel method for the upper anterior region. To rule out any surgical contraindications, a thorough medical and family history were completed and blood tests were performed.
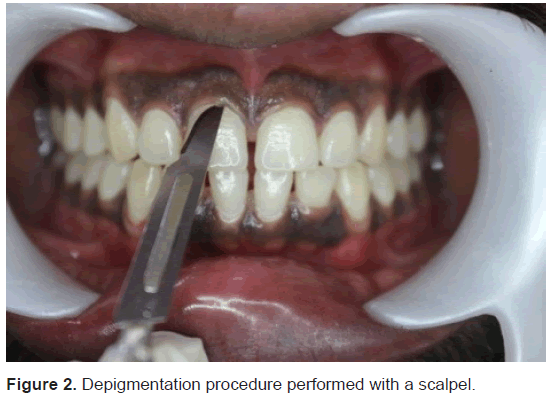
Conventional scalpel technique
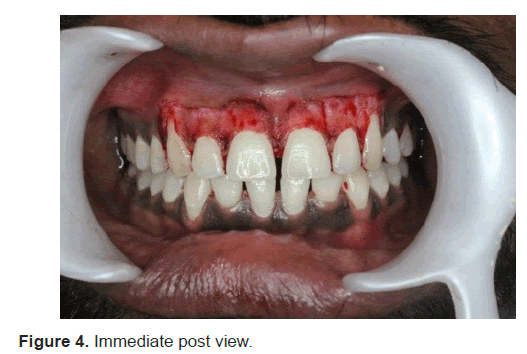
Using a No. 15 scalpel blade, two vertical incisions were made distal to the permanent canine right and left sides after block anesthesia with 2% lignocaine. In order to preserve the gingiva's natural architecture, a split-thickness flap was elevated and removed. Using sterile gauze and a pressure pack, the bleeding was managed. To stop the bleeding, sterile gauze soaked in saline was applied to the recipient site. Coe-Pak periodontal treatment was applied to the exposed depigmented area and left on for a week. It was decided to treat the pain with an analgesic. The surgical region was checked and the pack was removed after a week (Figures 1-6).
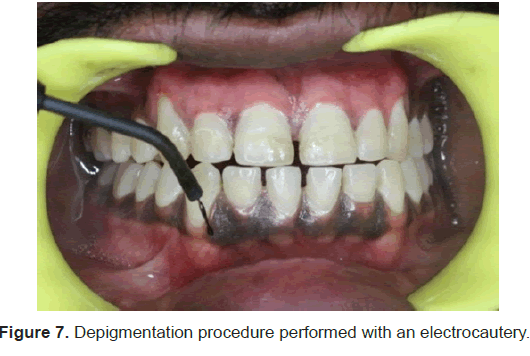
Electrosurgical technique
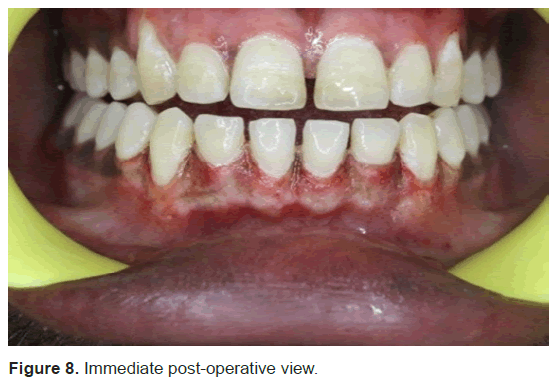
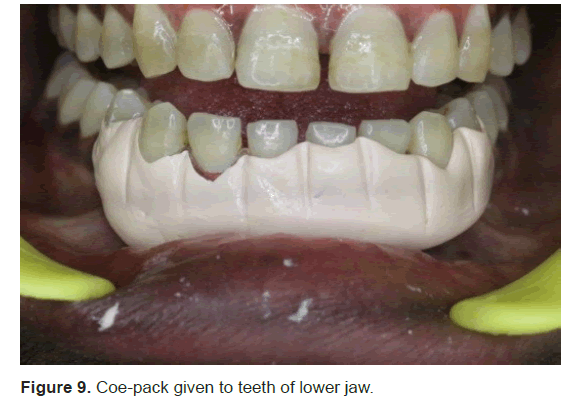
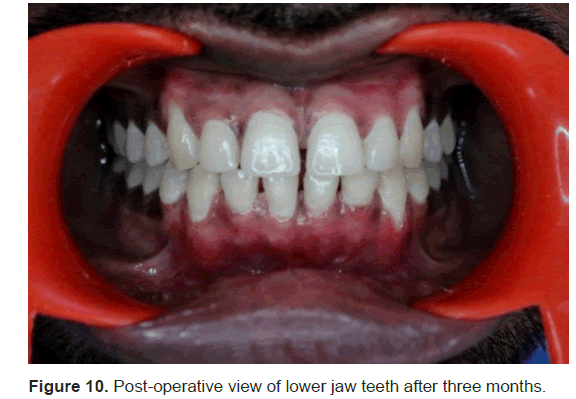
The hyperpigmented regions of the mandibular arch were de-epithelialized using an electrocautery device (also known as an electrosurgery unit). Using surgical loupes and an electrocautery machine, the pigmented tissues were ablationed while following conventional precautionary procedures. Using a sterile gauge dipped in saline solution, remnants of ablated tissues were extracted. Until the required depth of tissue removal was reached, this process was repeated. A noneugenol-based periodontal dressing “coe pack” was used to cover the surgical site and the patient was given postoperative instructions. After one week, the patient was summoned back for a follow-up visit and the removal of the periodontal dressing. An analgesic was provided for pain treatment (Figures 7-10).
Depigmentation procedure in relation to scalpel
The following figures depict the depigmentation procedure in relation to scalpel.
Depigmentation procedure in relation to electrocautery
The following figures illustrate the depigmentation procedure in relation to electrocautery.
Results
Following the application of the two methods, outcomes were compared in terms of post-operative discomfort, edema, time, cost effectiveness and healing. After a week, the scalpel technique wound area remained raw and erythematous. This was in contrast to the electrosurgical location, which had more edema but less erythema. There were no complications during the healing process for either the mandibular or maxillary arch. The gingiva appeared normal and healthy, with a pink colour, during intraoral inspection. After a month, the patient was called back and postoperative pictures were taken.
Discussion
Melanin is non hemoglobin derived brown pigments that often occur in the gingiva as a result of increased deposition of melanosomes in the basal layer. Pigmented gingival tissue forces the patient to go for esthetic treatment. Degree of vascularization, the thickness of the keratinized layer and the amount of the pigment- containing cells determines the color of gingiva [5]. Various treatment plans have a different outcome in respect of pain, bone exposure, bleeding, healing and patient comfort. The selection of a technique for the depigmentation of the gingiva should be based on clinical experience, patient’s affordability and individual preferences. The mechanism of repigmentation is not very clear, but according to the migration theory, active melanocytes moves from the adjacent pigmented tissues and migrate to the treated areas, causing repigmentation [9,5].
Scalpel surgical technique is highly recommended in consideration of the equipment constraints that may not be frequently available in clinics. However, scalpel surgery causes unpleasant bleeding during surgery, pain and discomfort after surgery and it is necessary to cover the surgical site with periodontal dressing for 7 to 10 days. The scalpel technique by some authors, has been reported to be relatively simple and versatile and it requires minimum time and effort but actually in the present case, more time in the dexterity was required [4,6].
Superior efficacy of electrosurgery as compared to scalpel has been explained on the basis of Oringer’s ‘exploding cell theory’. According to this theory it is stated that the electrical energy leads to molar disintegration of melanin cells in basal and sub basal layers of the operated and the surrounding sites. Thus electrosurgery has a strong influence in retarding migration of melanin cells from the locally situated cells. However, in the present case report, no difference in the recurrence of pigmentation was observed in scalpel and electrosurgical technique. The dissection of partial thickness flap by scalpel required more surgical expertise as compared to electrosurgery. Electrosurgery, however, has the disadvantage that prolonged or repeated application of current to tissue induces heat accumulation and undesired tissue destruction. Thus, contact with periosteum or alveolar bone and vital teeth should be avoided [10].
The electrosurgery group experienced less pain, reduced healing discomfort and scar formation. Other advantages were reduced bleeding and hence clear view of the surgical site, use in difficult to reach areas, reduced chair side time of the surgical procedure and operator fatique [10].
Conclusion
It may be concluded that there was no recurrence with any of the procedures and the two approaches yielded healing outcomes that were equivalent. But in terms of the immediate postoperative assessment, the electrosurgical technique did not show any bleeding since the burned layer acted as a surgical bandage to halt the bleeding, but the scalpel technique left a bleeding surface. Technical proficiency is necessary even though electrosurgery has the advantage of less bleeding but must be performed with prudence. In contrast to the scalpel method, electrosurgery provided the best recovery after one week. Thus, it can be said that, within the parameters of the current case study, all two modalities generated results that were equivalent over the long run.
References
- Attar NB, Gupta B, Deshmukh A, Shahabe S, Zope S, et al. Pigmentation on Gingiva: A diagnostic dilemma. Int J Periodontics Restorative Dent. 2018;38:137–140.
- Alhabashneh R, Darawi O, Khader YS, Ashour L. Gingival depigmentation using Er: YAG laser and scalpel technique: A six-month prospective clinical study. Quintessence Int. 2018;49(2).
- Müller S. Melanin‐associated pigmented lesions of the oral mucosa: Presentation, differential diagnosis and treatment. Dermatol Ther. 2010;23(3):220-229.
- Sreeja C, Ramakrishnan K, Vijayalakshmi D, Devi M, Aesha I, et al. Oral pigmentation: A review. J Pharm Bioallied Sci. 2015;7(Suppl 2):S403–S408.
- Cicek Y, Ertas U. The normal and pathological pigmentation of oral mucous membrane: A review. J Contemp Dent Pract. 2003;4(3):76-86.
- Tamizi M, Taheri M. Treatment of severe physiologic gingival pigmentation with free gingival autograft. Quintessence Int. 1996;27:555-558.
- Shah SS. Surgical esthetic correction for gingival pigmentation: Case series. J Interdiscip Dent 2012;2: 195–200.
- Kaur H, Jain S, Sharma RL. Duration of reappearance of gingival melanin pigmentation after surgical removal: A clinical study. J Indian Soc Periodontol. 2010;14:101-105.
- Almas K, Sadiq W. Surgical treatment of melanin-pigmented gingiva: An esthetic approach. Indian J Dent Res. 2002; 13:70–73.
- Oringer Mj. Electrosurgery in dentistry. 1975.







 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.