Comparative Study of Corpus Luteum Ultrasonographic Findings in Normal and Abnormal Pregnancies of the First Trimester in Patients Referred to the Hospital
Citation: Hajiahmadi S, et al. Comparative Study of Corpus Luteum Ultrasonographic Findings in Normal and Abnormal Pregnancies of the First Trimester in Patients Referred to the Hospital. Ann Med Health Sci Res. 2018;8:397-400
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: According to the limited number of studies in this field as well as the contradiction in the results of these studies, we performed this study to investigate corpus luteum RI in normal and abnormal pregnancies of the first trimester and comparison between the two groups. Methods: In this cross-sectional study, 50 abnormal pregnant and 50 normal pregnant women were selected and were underwent ultrasonography. Blood flow impedance was measured by using the PSV, EDV and RI and the average of three times measuring was considered as the final RI in each patient. Corpus luteum diameter and PSV were also measured in each patient and compared between the two groups. Results: The mean of Resistance index, peak systolic velocity and Diameter in the normal and abnormal groups were 0.509 ± 0.068 (p=0.308), 28.71 ± 13.83 and 25.16 ± 13.36(p=0.207), 19.85 ± 5 and 18.86 ± 5.17 (p=0.343) respectively. Conclusion: The results of our study showed that the profile of corpus luteum in normal and abnormal pregnancies was not differing significantly.
Keywords
Pregnancy; Corpus luteum; Sonography
Introduction
In a menstrual cycle leading to pregnancy, when ovulation occurred, the remaining part of ovarian follicles is transformed to corpus luteum by luteinizing hormones. New angiogenesis in granulosa cells of ovarian follicles is occurred, which provides appropriate vascular bed for releasing progesterone in to blood stream. Also, this rich vascular bed can lead to bleeding into the corpus luteum. The survival of corpus luteum in the early pregnancy is dependent on β-hCG level in the mother’s circulation. Corpus luteum naturally produces progesterone until the end of the first trimester of pregnancy, next it is diminished gradually and the placenta will act as the main source of progesterone production instead. Bleeding in corpus luteum leads to its cystic enlargement during pregnancy. [1-5]
Proper and adequate corpus luteum function is essential for the survival of pregnancy in the first weeks. The regulation of corpus luteum function in early pregnancy is not well known. However, it seems that the regulation of corpus luteum function is primarily performed by the rate of change in the β-hCG level in the mother’s circulation, although the validity of this issue is still questioned. Some studies have shown that progesterone levels in spontaneous abortions are significantly lower than normal pregnancies. Therefore, inadequate corpus luteum function may be considered as a possible cause of spontaneous abortion. Most studies about corpus luteum function in early pregnancy have been conducted by the measurement of blood hormone levels, however with the advent of Color Doppler Sonography, possibility of checking the uterus, ovarian and corpus luteum blood flow is provided by transvaginal or transabdominal sonography. [6] In a study by Tamura et al., It was shown that in a normal menstrual cycle, the RI (resistance index) of the follicle was high before ovulation and significantly reduced after ovulation. However, the RI has decreased in the beginning and middle part of the luteal phase, it become increased in the late part. In the mentioned study, it was also shown that RI in the middle of the luteal phase of menstruation in patients with luteal phase deficiency is significantly higher than those with proper luteal phase function. This study showed that RI of corpus luteum is normal up to the 7th week of pregnancy and then significantly increases. [7]
The vascularity of corpus luteum is known as an indicator of proper function of this cyst. [8-10] So far, limited studies have been conducted on the comparison of corpus luteum RI in normal and abnormal pregnancies.
According to the limited number of studies in this field as well as the contradiction in the results of these studies, we performed this study to investigate corpus luteum RI in normal and abnormal pregnancies of the first trimester and comparison between the two groups.
Methods
This is a cross-sectional study which was conducted in Al-Zahra Medical Center of Isfahan in 2017. The target population of the study was pregnant women.
Inclusion criteria were: abnormal early pregnancy ranging from 6 to 12 weeks of pregnancy including threatened abortion, missed abortion, and an embryonic pregnancy (blighted ovum) and normal intrauterine pregnancy between weeks 6 to 12 for the control group. Patient consent for participation in the study is necessary. Consumption of progesterone during pregnancy was also considered as exclusion criteria.
After obtaining permission from the university’s medical ethics committee, 50 pregnant women with abnormal pregnancy and 50 pregnant women with natural pregnancy were selected and after receiving written consent from them, they entered the study. All pregnant women entered the study were underwent ultrasonography by one experienced radiologist via Medison Ultrasound Apparatus 2005. After finding corpus luteum in sonography, color doppler box was placed on it to detect blood flow around corpus luteum. Then, the sample volume was centered on the highest degree of observed color to evaluate the spectral wave. At least three spectral waves were taken from each patient. Blood flow impedance was measured by using the PSV, EDV and RI (RI=(PSV-EDV) / PSV} formula, and the average of three times measuring was considered as the final RI in each patient. Corpus luteum diameter and PSV were also measured in each patient, and along with other patient data (including age, parity status, gestational age based on the last menstrual period) were recorded in each patient’s profile and if the fetus was not seen at the 6th week of gestation based on LMP, the ultrasonography was repeated one week later. Also, if there is a difference of more than a week between gestational age based on LMP and ultrasound measurement, sonography measurement was considered as the gestational age of the patient. This correction of the gestational age will only take place in cases of natural pregnancy and the threatened abortion.
Definition of threatened abortion in this study is the presence of vaginal bleeding with a closed cervix in a clinical examination. The presence of a gestational sac (GS) containing the embryo without cardiac activity is called missed abortion and a pregnancy with gestational sac larger than 25 mm without embryo in transvaginal ultrasonography was known as an embryonic pregnancy or blighted ovum. Data were analyzed by SPSS software version 24 and analyzed by Chi-square T-test and Pearson correlation.
Results
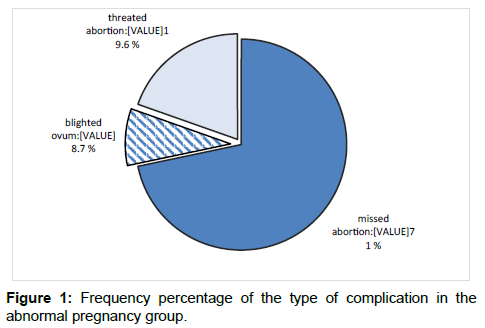
In this study, 50 pregnant women with normal pregnancy and 50 pregnant women with abnormal pregnancy were enrolled. In the course of the study, 4 patients from abnormal pregnancy group were excluded from the study due to non-visualization of corpus luteum in ultrasonography. Data were analyzed on 50 controls and 46 patients. Of 46 abnormal pregnancies, 33 cases (71.7%) were threatened abortion, 4 cases (8.7%) were blighted ovum, and 9 cases (19.6%) were missed abortions [Figure 1].
Table 1 shows the distribution of demographic variables and medical records of both normal and abnormal pregnancy groups. The mean age of the mother, the gestational age, gestational parity, abortion history, spotting in previous pregnancy and the underlying disease were not significantly different between the two groups, but visualized FHR (fetal heart rate) in the two groups was significantly different (p=0.007) and the frequency of not visualized FHR was higher in the abnormal pregnancy group.
| Variables | Groups | p-value | ||
|---|---|---|---|---|
| Normal | Abnormal | |||
| Maternal age (years) | 31.4 ± 5.52 | 30.67 ± 5.44 | 0.519 | |
| Gestational age (week) | 8.52 ± 2 | 7.81 ± 1.77 | 0.072 | |
Gestational parity |
1 | 24(48) | 22(47.8) | 0.76 |
| 2 | 17(34) | 18(39.1) | ||
| 3 and more | 9(18) | 6(13) | ||
| Abortion history | 6(12) | 6(13) | 0.877 | |
| Spotting in previous pregnancy | 1(2) | 2(4.3) | 0.606 | |
| Underlying disease | 7(14) | 1(2.2) | 0.061 | |
| Visualized FHR | 41(82) | 26(56.5) | 0.007 | |
Table 1: Distribution of demographic and clinical variables in both patient and control groups.
In Table 2, mean and standard deviation of the resistance index (RI), peak systolic velocity (PSV), and diameter of corpus luteum are shown in normal and abnormal pregnancy groups. According to the T-test, there was no significant difference between the mean of the three indices in normal and abnormal pregnancies (p>0.05).
| Variable | Groups | p-value | |
|---|---|---|---|
| Normal | Abnormal | ||
| Resistance index | 0.509 ± 0.068 | 0.524 ± 0.073 | 0.308 |
| peak systolic velocity | 28.71 ± 13.83 | 25.16 ± 13.36 | 0.207 |
| Diameter | 19.85 ± 5 | 18.86 ± 5.17 | 0.343 |
Table 2: Mean and standard deviation of resistance index (RI), peak systolic velocity (PSV) and diameter of corpus luteum.
In Table 3, the mean and standard deviation of the three variables i.e., resistance index, peak systolic velocity, and diameters of corpus luteum are shown by type of complication. According to one-way ANOVA, the mean of the three parameters was not significantly different in terms of the type of complication (p>0.05).
| Type of complication | RI | PSV | Diameter |
|---|---|---|---|
| Uncomplicated (normal) | 0.509 ± 0.068 | 28.71 ± 13.83 | 19.85 ± 5 |
| Threatened abortion | 0.522 ± 0.074 | 24.91 ± 12.89 | 19.61 ± 5.68 |
| Blighted Ovum | 0.588 ± 0.067 | 25 ± 18.38 | 17.25 ± 2.75 |
| Missed abortion | 0.498 ± 0.067 | 26.25 ± 14.72 | 16.56 ± 2.67 |
| p-value | 0.0138 | 0.651 | 0.304 |
Table 3: Mean and standard deviation of resistance index (RI), peak systolic velocity (PSV) and diameter of corpus luteum according to type of complication.
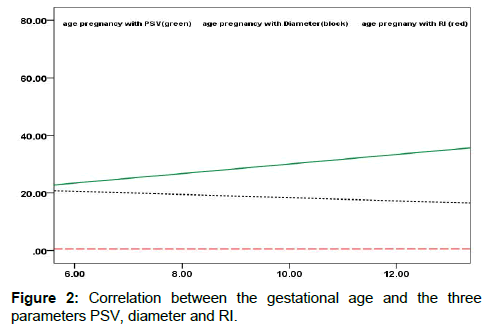
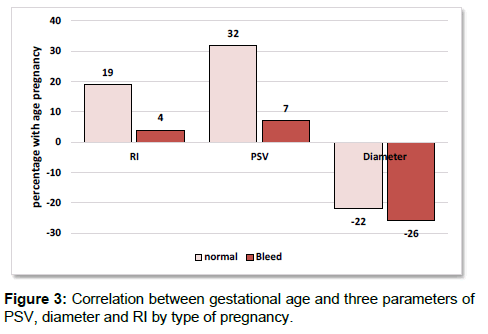
Analysis of the data using Pearson correlation test showed that there was no significant relationship between three parameters of RI, PSV and diameter of corpus luteum with maternal age but there was a direct and significant correlation between gestational age and PSV (0.23) (p=0.023). Also, there was a reverse correlation between the gestational age and diameters (0.12) which was statistically significant (p=0.041). However, there was no significant relationship between gestational age and RI (p=0.36). On the other hand, the correlation between gestational age and corpus luteum characteristics in normal and abnormal pregnancies showed that there is a direct and significant correlation (0.32) between gestational age and PSV in the normal group (p=0.024) however, the correlation between gestational age and RI was 0.19 (p=0.19) and the correlation between gestational age and diameter was -0.22 (p=0.12). However, there was no significant correlation between gestational age and none of the corpus luteum (corpus luteum) features in the group of abnormal pregnancies. In this group, the correlation between gestational age, RI, PSV and diameter of corpus luteum was 0.04, 0.07 and 0.02% respectively. In Figures 2 and 3, the correlation between the gestational age and the three parameters is shown.
Logistic regression analysis showed that among the variables of maternal age, gestational parity pregnancy, history of abortion, spotting in previous pregnancy, underlying disease, gestational age, visualization of FHR and corpus luteum characteristics (PSV, diameter and RI), only two variables i.e., the visualization of FHR and gestational age are associated with abnormal pregnancy, as the incidence of abnormal pregnancy decreases by 0.78 times as the gestational age increases each week (OR=0.78, 95% CI=0.62-0.99, p=0.044). Also, non-visualized FHR increases the chance of abnormal pregnancy by 3.5 times (OR=3.5, 95% CI: 1.29-9.37, p=0.014).
Discussion
Abnormal pregnancies, which mainly include threatened abortion, blighted ovum, missed abortion are of the most important problems in pregnancy and are a serious challenge among gynecologists. So far, several methods for its diagnosis and management have been presented, however no single theory has been presented in this regard. Some previous studies have shown that corpus luteum features such as RI, PSV, and diameter can help in the diagnosis of abnormal pregnancy, but in our study, the values of the above parameters were not significantly different between the two groups of normal and abnormal pregnancies considering that the two groups did not differ significantly in terms of demographic and clinical characteristics. Also, according to the results of our study, the features of corpus luteum were not significantly different in terms of type of complication (natural pregnancy, threatened abortion, blighted ovum, missed abortion). In a study by Alcázar et al., it has been shown that in cases of missed abortion, the RI of corpus luteum is significantly higher than in normal pregnancies. However, in that study, there was no significant difference between threatened abortion and an embryonic pregnancy cases with normal pregnancy. [6] However, in another study by Frates et al. in 2001, there was no obvious relationship between the ultrasonographic profile of corpus luteum and the results of pregnancy in the first trimester. [11] On the other hand, in a study conducted by Kupesić, it has been shown that RI is significantly increased in cases of threatened abortion, complete and incomplete abortion. [12] Of course, in our study, the average of RI was higher in cases of threatened abortion and blighted ovum than normal pregnancies, but this difference was not significant, statistically. According to the results of our study, there was a direct and significant correlation between gestational age and PSV of corpus luteum and also reverse correlation between gestational age and diameter of corpus luteum. However, there was no significant relationship between gestational age and RI. On the other hand, the correlation between gestational age and corpus luteum characteristics in normal and abnormal pregnancies showed that there is a direct and significant correlation between gestational age and PSV of 0.32 (p=0.024) in normal pregnancies but the correlation between gestational age and RI was 0.19 (p=0.19) and the correlation between gestational age and diameter was - 0.22 (p=0.12). However, in the group of abnormal pregnancies, there was no significant correlation between gestational age and none of the characteristics of corpus luteum, which is quite normal due to the lack of growth of the fetus in abnormal pregnancies. Regarding changes in the characteristics of corpus luteum during pregnancy, Tamura et al. showed that in a normal menstrual cycle, the follicle RI was high before ovulation and significantly decreased after ovulation, while the RI is lowered at the beginning and middle of the luteal phase and then increases in the late luteal phase. It was also shown in this study that RI in the middle of the luteal phase of menstruation in patients with luteal phase deficiency is significantly higher than those with proper luteal phase function. This study showed that luteal RI is normal up to the 7th week of pregnancy and then significantly increases. [7] Therefore, the findings of that study show that the relationship between the RI and the gestational age is not linear and direct, and its values change in different weeks of pregnancy. Therefore, measurement of corpus luteum profile should be proportional to the gestational age, and in fact, all individuals who are under went the measurement of these indices in two groups of normal and abnormal pregnancies, should not have a significant difference in gestational age. However, in our study, although the gestational age did not differ significantly between normal and abnormal pregnancies, but the mean age of the gestational age in normal group was about one week more than the abnormal group and the difference between the two groups age was very close to the significant level.
The results of our study showed that two factors of gestational age and visualization of FHR can be helpful in determining the nature of pregnancy, so that with the increase in the gestational age, the chance of abnormal pregnancy decreases significantly and when FHR is notvisualized, the chance of abnormal pregnancy is increased. Therefore, in clinical trials of pregnant mothers, these two items, especially the visualization of FHR, should be carefully considered.
Conclusion
The results of our study showed that the profile of corpus luteum in normal and abnormal pregnancies was not differing significantly, but some features such as PSV and diameter of corpus luteum change during different gestational age, therefor considering gestational age for measurement of characteristics of corpus luteum is necessary.
Study limitations
This is a descriptive study on a small sample size which may lead to the imprecise estimation of sonography findings. Furthermore, lack of comparison group pushed us just to describe findings. On the other hand, due to the limitations of this study, including the difference between the gestational week in both normal and abnormal pregnancies, further studies are recommended.
Financial support and sponsorship
This study was supported by Isfahan University of Medical Sciences. This design was registered in research faculty of medical school of Isfahan by code 395112.
Conflict of Interest
The authors disclose that they have no conflicts of interest.
REFERENCES
- Warren MP, Vu C. Central causes of hypogonadism--functional and organic. Endocrinol Metab Clin North Am. 2003;32:593-612.
- Speroff L, Glass RH, Kase NG. Anovulation and the polycystic ovary syndrome. Clinical Gynecologic Endocrinology and Infertility. Philadelphia, PA: Lippincott Williams & Wilkins; 1999;487-513
- Butler L, Santoro N. The reproductive endocrinology of the menopausal transition. Steroids. 2011;76:627-635.
- Potter AW, Chandrasekhar CA. US and CT evaluation of acute pelvic pain of gynecologic origin in nonpregnant premenopausal patients. Radiographics. 2008;28:1645-1659.
- Di Salvo DN. Sonographic imaging of maternal complications of pregnancy. J Ultrasound Med. 2003;22:69-89.
- Alcázar JL, Laparte C, López-Garcia G. Corpus luteum blood flow in abnormal early pregnancy. J Ultrasound Med. 1996;15:645-649.
- Tamura H, Takasaki A, Taniguchi K, Matsuoka A, Shimamura K, Sugino N. Changes in blood-flow impedance of the human corpus luteum throughout the luteal phase and during early pregnancy. Fertil Steril. 2008;90:2334-2339
- Razika MA, Faraga MAH, Shetab M. Uterine and ovarian arteries blood flow during the mid-luteal phase in women with unexplained infertility. MEFS J. 2014;20:209-212.
- Qiu JJ, Liu YL, Liu MH, Chen LP, Xu DW, Zhang ZX, et al. Ovarian interstitial blood flow changes assessed by transvaginal colour Doppler sonography: predicting ovarian endometrioid cyst-induced injury to ovarian interstitial vessels. Arch Gynecol Obstet. 2012;285:427-433
- Pinaffi Fábio LV, Santos Ériko S, Silva Maurício G da, Maturana Filho, Milton Madureira Ed H, Silva Luciano A. Follicle and corpus luteum size and vascularity as predictors of fertility at the time of artificial insemination and embryo transfer in beef cattle. Pesquisa Veterinária Brasileira. 2015;35:470-476.
- Frates MC, Doubilet PM, Durfee SM, Di Salvo DN, Laing FC, Brown DL, et al. Sonographic and Doppler characteristics of the corpus luteum: can they predict pregnancy outcome? J Ultrasound Med. 2001;20:821-827
- Kupesic S. The first three weeks assessed by transvaginal color Doppler. J Perinat Med. 1996;24:301-317.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.