Comparative Ultrasonographic Evaluation of the Carotid Intima-media Thickness in Hypertensives with Computed Tomographic Features of Stroke and Normotensives in Benin
2 Department of Radiology, College of Medical Sciences, University of Benin, Benin, Edo, Nigeria, Email: blessing.igbinedion@uniben.edu
Citation: Denise OO, et al. Comparative Ultrasonographic Evaluation of the Carotid Intima-media Thickness in Hypertensives with Computed Tomographic Features of Stroke and Normotensives in Benin. Ann Med Health Sci Res. 2018;8:24-28
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Hypertension is a major public health problem, and it is a major risk factor for stroke. The most important pathophysiologic mechanism for the development of stroke is the induction of atherosclerosis. Carotid intima-media thickness (CIMT) is a very reliable and reproducible marker of the degree of atherosclerosis and has a good correlation with the onset/ severity of clinical manifestations. Materials and Methods: This study is an observational comparative cross-sectional type which measured the CIMT (using B-mode ultrasound) of 100 hypertensive patients with CT evidence of stroke and 100 normotensive age and sex-matched controls. The data was analyzed using SPSS version 17. Statistical tests were considered significant at p-value ≤0.05 at a confidence interval of 95%. Results: The mean age of the cases was 62.4 ± 11.8 years while that for the controls was 58.3 ± 12.5 years. The mean right and left CIMT were 1.02 ± 0.24 mm and 1.04 ± 0.32 mm respectively, with a range of 0.8 to 1.8 mm when compared to matched normotensive controls with a mean CIMT of 0.72 ± 0.15 mm and 0.76 ± 0.14 mm on the right and left respectively, and a range of 0.5 to 0.9 mm. Conclusion: This study found a consistent statistically significant increase in CIMT of hypertensive adults with stroke when compared with normotensive controls (p<0.001). In addition, CIMT values were found to increase with increasing age among the normotensives.
Keywords
CIMT; IMT; Carotid; Intimal-medial thickness; Stroke
Introduction
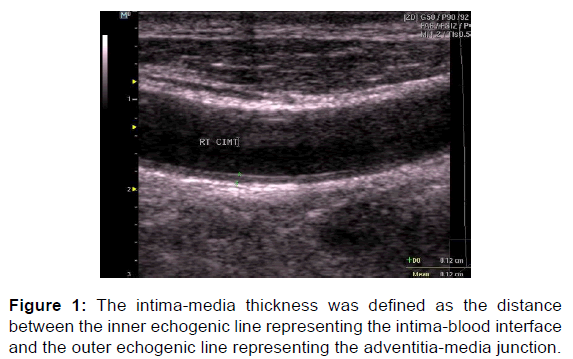
The carotid arteries are the major arteries that supply the brain. Consequently, compromise of blood flow through it may have significant neurological sequelae. The vascular compromise can be from thickening of its wall, constriction, atherosclerosis, plaque formation and other morphological causes of carotid hemodynamic flow disturbance. Thickening of the carotid artery walls (intima-media thickening) is a complex process which depends on a variety of factors especially vascular hemodynamics like elevated blood pressure and changes in vascular wall shear stress. Other mechanisms for intima thickening include intima hyperplasia and intimal fibrocellular hypertrophy. [1] The intimal-medial thickness is sonographically defined by the two parallel echogenic lines (double line pattern) which correspond to the lumen-intima and the media-adventitia interfaces. [2]
Thickened CIMTs are associated with plaque formation. CIMT is dependent on a wide range of vascular risk factors such as age, gender, race, smoking, systemic hypertension, diabetes mellitus, body mass index, dyslipidemia and hereditary factors. [3,4] The intima-media thickness of the common and internal carotid arteries is a sensitive assessment tool which correlates well with the onset and severity of atherosclerosis which is the single most important mechanism of development of most cerebrovascular accidents. [2,3] CIMT is also useful in serial monitoring as well as follow-up of hypertensive patients with stroke.
An epidemiological study established that CIMT, as measured by ultrasound, is a good marker of atherosclerosis and has repeatedly been used to predict the occurrence of stroke, peripheral vascular disease and myocardial infarction in the general population. [5] Despite these reports ultrasound determined CIMT is not adequately utilized even in high-risk groups such as in hypertensives in developing countries like Nigeria. Thus, complications from atherosclerosis such as stroke continue to impose a great burden on us, unlike the significant decline of its impact on developed nations.
Ultrasonography is a non-invasive, reliable and safe method for evaluating CIMT in hypertensives patients with symptomatic carotid artery disease such as stroke. It can be used to monitor disease progression such that timely therapeutic interventions can be instituted which will lower the risk of a repeat stroke and other complications. The carotid artery is best appreciated sonologically using Doppler application and standardized protocol. However, the expertise for Doppler scan of the carotid artery is limited in Nigeria due to lack of trained personnel, unavailability of ultrasound machines with Doppler capability, lack of interest in Doppler scans, unfavorable government policies, poverty, long duration of completing a Doppler scan, amongst other reasons. However, with grey-scale ultrasound important vital information for the management of patients with hypertension and stroke can be obtained.
The aim of this study is to document grey-scale ultrasound scan findings in hypertensives with stroke and in normotensives. In addition, this study will provide some useful information in the early detection and in the recognition of carotid artery disease progression so that prompt interventions may be commenced (which may prevent the occurrence of a repeat stroke as well as other associated complications and co-morbidities).
Materials and Methods
The study is a descriptive comparative cross-sectional type conducted on 100 consecutive consenting hypertensive patients with CT evidence of stroke and 100 age-and-sex matched ‘controls’ who were normotensive without stroke or cardiovascular risk factors. This study is in compliance with the Code of Ethic of the World Medical Association (Declaration of Helsinki) for experiments involving humans. Full respect to human right and privacy was maintained all through the study. Informed consent was obtained from the study participants for study on human subjects, and ethical approval was granted by the Ethics Committee of the reference institution. History and duration of hypertension were obtained from the case-note or the patient. The participants’ age, gender and blood pressure were obtained prior to the ultrasound examination.
Real-time gray scale ultrasound scans were done using a Mindray Z5 unit (Shenzhen Mindray Bio-Medical Electronics Co., Ltd. China 2010) with a linear transducer of frequency range 7.5 to 10 MHz. The examinations were carried out with the patients lying supine, neck slightly extended and turned contralateral to the carotid artery being examined. The scans were done in the antero-posterior and transverse planes after the application of ultrasound acoustic gel.
All measurements of the intima-media thickness were made in the longitudinal plane at a point 1 to 1.5cm proximal to the carotid bulb on the far wall of the common carotid artery (CCA). Internal carotid artery (ICA) intima-media thickness measurements were taken at the far wall of the internal carotid artery 0.5 to 1cm distal to the carotid bifurcation. The intima-media thickness measurements were also taken on the far wall of the carotid bulb. Both sides of the patients were scanned and measured.
the inner echogenic line representing the intima-blood interface and the outer echogenic line representing the adventitia-media junction [Figure 1]. The measurements of the intima-media thickness of the common carotid, bulb and internal carotid arteries were taken at a site free from plaques (as plaques are associated with atherosclerosis). Magnification of the ultrasound image was used to improve the accuracy of the measurements. The presence and sonographic appearance of atherosclerotic plaques were also assessed and documented.
Data collected were analyzed using SPSS version 20 (IBMSPSS, Il, USA). Mean values and frequencies of observed variables were determined. Analysis of variation (ANOVA) was done. Chi-Square correlation studies were done with the significant level set at or below 0.05.
Results
Overall, 114 (57%) females and 86 (43%) males participated in the study. The sex distribution for the females and males was 58% and 42% for the cases and 56% and 44% for the controls. The mean age of the cases was 62.4 ± 11.8 years with a range of 35 to 90 years, while the mean age for the controls was 58.3 ± 12.49 years (range of 29 to 86 years). The sex and the mean age differences between the cases and control were not statistically significant (p=0.433 and 0.062 respectively). In terms of marital status, those that were married were the most numerous (79%). Those that had tertiary education were similarly highest in proportion (50%) on the educational level of the entire study population [Table 1].
| Variables | Cases 100 (%) |
Controls 100 (%) |
Total 200 (%) |
|
|---|---|---|---|---|
| Gender | Females | 58 (58.0) | 56 (56.0) | 114 (57.0) |
| Males | 42 (42.0) | 44 (44.0) | 86 (43.0) | |
| Marital status | Divorced | 3 (3.0) | 2 (2.0) | 5 (2.5) |
| Married | 77 (77.0) | 81 (81.0) | 158 (79.0) | |
| Single | 5 (5.0) | 15 (15.0) | 20 (10.0) | |
| Widowed | 15 (15.0) | 2 (2.0) | 17 (8.5) | |
| Educational level | None | 19 (18.0) | 6 (6.0) | 25 (12.5) |
| Primary | 21 (21.0) | 14 (14.0) | 35 (17.5) | |
| Secondary | 22 (22.0) | 17 (17.0) | 39 (19.5) | |
| Tertiary | 38 (38.0) | 63 (63.0) | 101 (50.5) |
Table 1: Social demographic characteristics of the study population.
Comparison of the mean CIMT values between the cases and controls [Table 2] showed higher measurements in the cases than the controls, which was statistically significant in all carotid segments, p=0.001. The left CCA IMT was significantly higher than the measurements on the right side in both the cases and controls, with p-values of 0.041 and 0.006 respectively. Similarly, higher IMT values were also seen in the left ICA when compared to the right. However, it was not at a statistically significant level in the cases (p=0.056), but was statistically significant in the controls - p=0.001. In the carotid bulbs, the IMTs were also statistically significantly higher in the left than the right in the cases and also in the controls; p=0.046 Vs. 0.003 respectively. In addition, consistently higher mean CIMT values were observed in the male than in the female participants [Table 3] and this was statistically significant in all the carotid measurements; all p-values were less than 0.05.
| Variables | Mean CIMT ± SD (mm) | T-test | p-value | ||
|---|---|---|---|---|---|
| CCA | Right | Cases | 1.02 ± 0.24 | 10.67 | 0.001 |
| Controls | 0.72 ± 0.25 | ||||
| Left | Cases | 1.04 ± 0.32 | 7.99 | 0.001 | |
| Controls | 0.76 ± 0.14 | ||||
| ICA | Right | Cases | 0.72 ± 0.25 | 6.73 | 0.001 |
| Controls | 0.58 ± 0.10 | ||||
| Left | Cases | 0.73 ± 0.15 | 5.64 | 0.001 | |
| Controls | 0.63 ± 0.11 | ||||
| Bulb | Right | Cases | 1.09 ± 0.04 | 6.57 | 0.001 |
| Controls | 0.78 ± 0.08 | ||||
| Left | Cases | 1.12 ± 0.13 | 5.81 | 0.001 | |
| Controls | 0.80 ± 0.17 |
Table 2: Comparison of mean CIMT values between the cases and controls.
| Variables | Sex | Cases Mean ± SD (mm) |
Controls Mean ± SD (mm) |
t-test | p-value |
|---|---|---|---|---|---|
| RCCA | Female | 0.95 ± 0.05 | 0.66 ± 0.10 | 2.08 | 0.031 |
| Male | 1.05 ± 0.12 | 0.73 ± 0.05 | 0.99 | 0.037 | |
| LCCA | Female | 0.99 ± 0.03 | 0.69 ± 0.07 | 1.90 | 0.010 |
| Male | 1.08 ± 0.11 | 0.78 ± 0.14 | 1.93 | 0.004 | |
| RT Bulb | Female | 1.01 ± 0.18 | 0.72 ± 0.03 | 0.93 | 0.040 |
| Male | 1.10 ± 0.09 | 0.79 ± 0.26 | 0.88 | 0.008 | |
| LT Bulb | Female | 1.06 ± 0.07 | 0.73 ± 0.04 | 2.17 | 0.013 |
| Male | 1.14 ± 0.13 | 0.82 ± 0.11 | 1.95 | 0.006 | |
| RICA | Female | 0.69 ± 0.21 | 0.52 ± 0.05 | 2.93 | 0.001 |
| Male | 0.74 ± 0.05 | 0.61 ± 0.12 | 0.87 | 0.027 | |
| LICA | Female | 0.68 ± 0.32 | 0.58 ± 0.09 | 1.39 | 0.008 |
| Male | 0.74 ± 0.37 | 0.68 ± 0.17 | 1.06 | 0.005 |
Table 3: Comparison of CIMT based on gender within the study population.
Correlation of the participants’ ages with IMT showed a positive correlation between the IMT values and ages of the cases as well as those of the controls bilaterally [Table 4]. This correlation was stronger in the controls than in the cases. A weak positive correlation between the duration of hypertension with the CIMT was not statistically significant in all the measurements.
| Variables | Artery | Study groups | r | P-value |
|---|---|---|---|---|
| Age and CIMT values for cases and controls. | ||||
| CCA | Right | Cases |  0.185 | 0.035 |
| Controls |  0.439 | 0.000 | ||
| Left | Cases |  0.245 | 0.014 | |
| Controls |  0.363 | 0.000 | ||
| ICA | Right | Cases |  0.187 | 0.043 |
| Controls | 0.533 | 0.000 | ||
| Left | Cases | 0.219 | 0.030 | |
| Controls | 0.354 | 0.000 | ||
| CIMT with duration of hypertension of the participants. | ||||
| CCA | Right |  0.109 | 0.292 | |
| Left |  0.169 | 0.101 | ||
| ICA |  Right |  0.137 | 0.186 | |
|  Left |  0.053 | 0.616 | ||
Table 4: Correlation study of age and CIMT values for cases and controls, as well as with duration of hypertension of the participants.
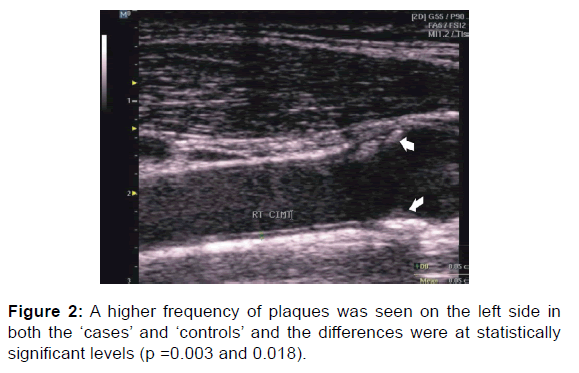
Carotid plaques [Figure 2] were observed in 55 subjects, comprising 27.5% of the study population [Table 5]. The presence of plaques was found in 40 (20%) of the ‘cases’ category and in 15 (7.5%) plaques in the ‘controls’. This difference was statistically significant with a p-value of 0.021. A higher frequency of plaques was seen on the left side in both the ‘cases’ and ‘controls’ and the differences were at statistically significant levels (p =0.003 and 0.018). About 11 (20%) participants had bilateral plaques.
| Variables | Cases N (%) |
Controls  N (%) |
Total N (%) |
P-value |
|---|---|---|---|---|
| Right | 13 (23.6) | 4 (7.3) | 17 (30.9) | 0.003 |
| Left | 19 (34.5) | 8 (14.5) | 27 (49.1) | 0.018 |
| Bilateral | 8 (14.5) | 3 (5.5) | 11 (20.0) | 0.037 |
| Total | 40 (72.7) | 15 (27.3) | 55 (100.0) | 0.021 |
Table 5: Ultrasonographic evaluation of carotid plaque frequency in the study population.
On localizing the plaques, the majority of the carotid plaques were in the carotid bulb with 28 plaques on the left and 16 on the right [Table 6]. There were 22 plaques in the left CCA and 16 in the right; while 10 plaques were in the right ICA and 7 in the left. There were statistically significant differences in the frequencies of plaque distribution between the cases and controls in all the carotid arteries and bulb bilaterally, with p values <0.05 [Table 6]. Heterogenous plaques were more common in the stroke patients compared to the predominantly homogenous plaques found in the normotensive ‘controls’ which was consistent in all the carotid arteries [Table 7].
| Variables | Case N (%) |
Controls N (%) |
Total N (%) |
Chi-square | P-value | |
|---|---|---|---|---|---|---|
| CCA | Right | 12 (12.0) | 4 (4.0) | 16 (8.0) | 4.348 | 0.037 |
| Left | 14 (14.0) | 8 (8.0) | 22 (11.0) | 1.839 | 0.017 | |
| ICA | Right | 8 (8.0) | 2 (2.0) | 10 (5.0) | 3.789 | 0.042 |
| Left | 5 (5.0) | 2 (2.0) | 7 (3.5) | 1.332 | 0.048 | |
| Bulb | Right | 13 (13.0) | 3 (3.0) | 16 (8.0) | 6.793 | 0.009 |
| Left | 20 (20.0) | 8 (8.0) | 28 (14.0) | 5.980 | 0.014 | |
| Total | 100 (100.0) | 100 (100.0) | 200 (100.0) |
Table 6: Ultrasonographic evaluation of plaques in the various carotid segments.
| Artery | Plaque echotexture | Cases N (%) |
Controls N (%) |
Chi-square | P-value | |
|---|---|---|---|---|---|---|
| CCA | Right | Homogenous | 3 (3.0) | 2 (2.0) | 2.359 | 0.012 |
| Heterogenous | 9 (9.0) | 2 (2.0) | ||||
| Left | Homogenous |  4 (4.0) | 6 (6.0) | 3.867 | 0.036 | |
| Heterogenous | 10 (10.0) | 2 (2.0) | ||||
| ICA | Right | Homogenous | 3 (3.0) | 2 (2.0) | 2.225 | 0.042 |
| Heterogenous | 5 (5.0) | 0 (0.0) | ||||
| Left | Homogenous | 2 (2.0) | 1 (1.0) | 1.982 | 0.048 | |
| Heterogenous | 3 (3.0) | 1 (1.0) | ||||
| Bulb | Right | Homogenous | 2 (2.0) | 2 (2.0) | 3.984 | 0.017 |
| Heterogenous | 11 (11.0) | 1 (1.0) | ||||
| Left | Homogenous | 6 (6.0) | 6 (6.0) | 4.116 | 0.009 | |
| Heterogenous | 14 (6.0) | 2 (2.0) | ||||
Table 7: Ultrasonographic evaluation of carotid plaque echogenicity in the study population.
Discussion
There are variations in normal reference values for CIMT. Normal mean values of 0.66mm ± 0.18mm have been reported. [4] A study by Freitas et al. [6] considered a pre-bifurcation value of less than 0.8 mm as normal while values between 0.9-1.4 mm were considered as thickening. Values higher than 1.4mm indicated atheromatous plaque. [6] In this study, the mean CIMT of the hypertensive cases was significantly higher than the mean CIMT of the normotensive controls bilaterally. Other studies have shown similar changes in the CIMT of the common carotid arteries in hypertensives when compared to normotensive individuals. [4,6,7]
Furthermore, CIMT has been documented to increase significantly with age, males and hypertensives. [3,8] Furthermore, in the hypertensive cases of the index study the contribution from age was significantly reduced suggesting another contributor to the CIMT which was absent in the controls and it is probably the effect of systemic hypertension.
The duration of hypertension showed a weak positive correlation with the CIMT in the common and internal carotid arteries bilaterally, although not statistically significant. This agreed with findings in a similar study at Ibadan by Umeh et al. [9] The weak correlation between duration of hypertension and CIMT in this study may be due to recall bias or poor healthseeking behavior (as uncomplicated systemic hypertension is predominantly asymptomatic which results in late presentation with features of complications, thus giving a spurious short duration of hypertension).
There was consistently higher CIMT measurement on the left side when compared to the right side in both the cases and controls in all carotid arteries sections. This finding is in agreement with studies which have recorded greater CIMT on the left as compared to the right side. [7,10] A possible explanation may be due to the anatomy and hemodynamics of the left common carotid artery as it is a direct branch of the thoracic aorta resulting in different shear stress conditions that may lead to a faster development of atherosclerosis. [10]
In this study, higher mean CIMT values were observed in males’ common, internal carotid and carotid bulbs bilaterally for the cases and controls. This is in agreement with most studies which showed slightly higher values in males. [11] Reasons for this may be the female sex hormones are protective to the cardiovascular system before the onset of menopause or that female tolerates hypertension better than males. [11] On the other hand, this variation with gender among the hypertensive group was at variance with a study by Frietas et al. [6] in which no gender variation was observed.
The atherosclerotic changes responsible for increases in intimamedia thickness also lead to the formation of carotid plaques within the wall of vessels. This study found a predominance of plaques in the hypertensive stroke cases. It is consistent with other studies that have reported a higher incidence of carotid plaques in stroke patients than controls. [10,12] The commonest site of atherosclerotic plaques is the carotid bulb. [3,13] This is thought to originate from endothelial damage caused by disturbances in local blood flow resulting from bifurcation anatomy. [13]
It has also been documented that plaque morphology is an important factor in the development of embolic events, one of which is a stroke. [14] Plaques associated with large lipid pools or soft extracellular components are more prone to rupture and produce emboli and therefore cause symptoms. The finding of relatively more homogenous plaques in the non-stroke controls is probably as a result of homogenous plaques being stable plaques when compared to the heterogeneous unstable plaques that usually culminate in embolic phenomena. Some studies have shown that about a third of strokes were thromboembolic in origin, with carotid plaques as the embolic source. [13,14]
Among the stroke cases, there was significantly higher CIMT in the ischemic stroke subtype compared to the hemorrhagic and mixed stroke subtypes in common and internal carotid arteries bilaterally. However, the CIMT values in this study were lower than the findings by Sahoo et al. [12] who observed a mean CIMT of 0.798mm in patients with acute ischemic stroke. This difference is probably due to racial and geographical differences.
Ultrasonography can thus serve as a useful tool in the noninvasive assessment of the carotid arteries with the intima-media thickness serving as a well-recognized and easily assessed sonographic marker of carotid atherosclerosis although other risk factors like metabolic syndrome and carotid blood flow velocity are important for risk factor stratification. [15]
Hypertension has being shown in this study to increase CIMT. Thickened CIMT may increase the likelihood of developing stroke. Hence we recommend that periodic carotid scan be done on hypertensive, aged and other individuals with risk factors for stroke for proper stroke risk stratification. Management of these patients may be instituted as appropriate which may include hypotensive drugs, statins, niacin and other lipid-lowering drugs.
Limitations of this study include the fact that color Doppler and spectral analysis were not conducted as it’s beyond the study scope. In addition, it is not a cohort study as the participants were not followed over time. These may have provided additional information probably with some clinical importance but can be added in future studies.
Conclusion
The use of grey scale ultrasound can give insight into carotid disease especially when CIMT is measured and plaque sought out and characterized. Hence centers that do not have Doppler capable ultrasound may be able to do some form of carotid interrogation which can give some prognosis to possible CVA development, rather than do nothing. This can serve as a screening test for reference to other facilities with adequate carotid vascular Doppler examination.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Vicenzini E, Ricciardi MC, Puccinelli F, Altieri M, Vanacore N, Piero V, et al. Common carotid artery intima-media thickness determinant in a population study. J Ultrasound Med 2007; 26: 427-432.
- Mancia G, De Backer G, Dominiczak A, Cifkova R, Heagerty AM, Kjeldsen SE, et al. 2007 Guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105-1187.
- Onut R, Balanescu S, Constantinescu D, Calmac L, Marinescu M, Dorobantu M. imaging atherosclerosis by carotid intima-media thickness in vivo: How to, where and in whom? Maedica 2012; 7 (2): 153-162.
- Bhuyan R, Das GC, Mandal A, Pegu D, Deori I, Ujawane S, et al. Correlation between carotid intima media thickness and newly diagnosed hypertensive patients. Journal of Evolution of Medical and Dental Sciences 2015; 75 (4): 13049-13056. DOI: 10.14260/jemds/2015/1879.
- Qu B, Qu T. Causes of changes in carotid intima-media thickness: A literature review. Cardiovascular Ultrasound 2015; 13: 46.
- Freitas P, Piccinato CE, Paula Martins WP, Filho MF. Carotid atherosclerosis evaluated by Doppler ultrasound. Association with risk factors and systemic arterial disease. J Vasc Bras. 2008; 7:298-307.
- Sharma P, Lohani B, Chatauts SP. Ultrasonographic evaluation of carotid intima-media thickness in hypertensive and normotensive individuals. Nepal Medical College Journal. 2009; 11:133-135.
- Kolade-Yunusa, Ibinaiye PO, Abdukadir AY, Yunusa T. Comparative evaluation of ultrasound measurement of carotid artery intima media thickness in hypertensive and normotensive adult patients in Jos, Nigeria. West African Journal of Ultrasound 2014; 5 (2): 63-68.
- Umeh EO, Agunloye AM, Adekanmi AJ, Adeyinka AO. Ultrasound evaluation of intima-media thickness of carotid arteries in adults with primary hypertension at Ibadan, Nigeria. West Afr J Med. 2013; 32: 62–7.
- Agunloye AM, Owolabi MO. Exploring carotid sonographic parameters associated with stroke risk among hypertensive stroke patients compared to hypertensive controls. J Ultrasound Med. 2014; 33: 975-83.
- Ogunrin AO. Recent advances in the management of cerebrovascular accident. Benin Journal of Postgraduate Medicine. 2007; 9: 28-40.
- Sahoo R, Krishna MV, Subrahmaniyan DK, Dutta DK, Elanyovan S. Common intima-media thickness in acute ischemic stroke. Neurology India. 2009; 57: 627-630.
- Mughal MM, Khan MK, DeMarco JK, Majid A, Shamoun F, Abela GS. Symptomatic and asymptomatic carotid artery plaque. Expert Rev Cardiovasc Ther 2011; 9 (10): 1315-1330. doi: 10.1586/erc.11.120.
- Malgor RD, Wood EA, Lavarone OA, Labropoulos N. Stratifying risk: Asymptomatic carotid disease. J Vasc Bras 2012; 11 (1): 43-52.
- Kim GH, Youn HJ. Is carotid artery ultrasound still useful method for evaluation of atherosclerosis? Korean Circulation Journal 2016.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.