Concurrent Occurrence of Uterovaginal and Rectal Prolapse: An Uncommon Presentation
- *Corresponding Author:
- Dr. Uchenna Anthony Umeh
Department of Obstetrics and Gynecology, University of Nigeria Teaching Hospital, Ituku-Ozalla, Enugu, Nigeria.
E-mail: carn9000@yahoo.com
Abstract
Concomitant uterovaginal and rectal prolapse is an uncommon occurrence. Where laparoscopic equipment and skills are lacking, sacrohysteropexy with synthetic mesh and rectopexy can be accomplished by laparotomy, especially in women who desire to retain their uterus for either biological or psychological reasons. A 40‑year‑old primipara with a history of concomitant mass protruding from both her vagina and anus following a spontaneous unsupervised delivery at home. Following pelvic examination, a diagnosis of uterovaginal and rectal prolapse was made. In view of her parity and desire to retain her reproductive function, she was offered abdominal sacrohysteropexy with synthetic mesh and rectopexy with satisfactory postoperative recovery. In resource‑limited settings with concomitant uterine and rectal prolapse, open abdominal sacrohysteropexy with synthetic mesh and rectopexy is an effective and safe alternative to Manchester operation in the absence of laparoscopic equipment and skills.
Keywords
Concomitant, Rectal prolapse, Utero-vaginal prolapse
Introduction
Concomitant existence of uterovaginal and rectal prolapse is a rare, but very distressing condition that poses a challenge to the gynecologist. [1] Isolated uterovaginal or rectal prolapse is more common and the treatment is not as challenging as in the existence of the two in the same patient.[1] The etiology of uterovaginal and/or rectal prolapse is multifactorial; pelvic floor disorders, connective tissue disorders, and genetic predispositions have been implicated. [1,2] The pelvic floor disorders often develop as a result of repeated pregnancies and childbirths causing stretching and tearing of the endopelvic fascia, levator ani muscles, and perineal body. [1,2] A connective tissue disorder, Ehlers–Danlos syndrome, characterized by skin hyper-extensibility, abnormal wound healing, and joint hypermobility, is commonly associated with uterovaginal and/ or rectal prolapse. [2]
The management of concurrent uterovaginal and rectal prolapse is determined by certain factors including patient’s age, desire for preservation of coital and/or reproductive functions, general medical status, severity of the condition, and previous attempts at surgical correction, symptomatology and physical examination findings. [1,2] In a 6 months follow-up of 33 cases of uterovaginal prolapse after abdominal sacrohysteropexy, Moiety et al., reported a success rate of 94%. [3] Successful outcome has also been recorded in other studies. [1,4-6] In resource-limited settings, where laparoscopic equipment and skills are lacking, sacrohysteropexy with synthetic mesh can be accomplished by laparotomy. [5]
Case Report
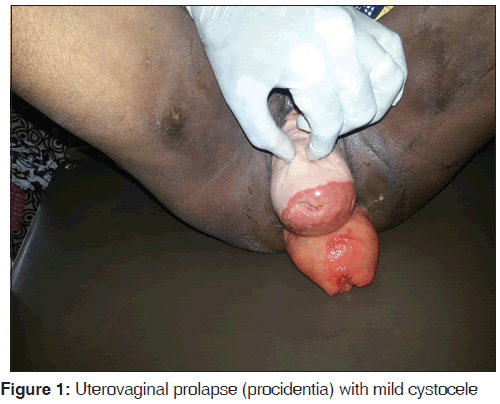
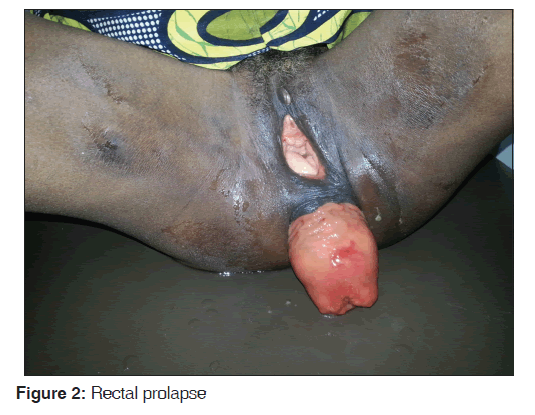
Mrs. B. O. is a 40-year-old petty trader. She is para 1+0 with one living male child. She achieved menarche at 14 years of age. She has a regular 28 days menstrual cycle with 4 days menstrual flow, and her last menstrual period was on January 15, 2014. She presented at the gynecology clinic of University of Nigeria Teaching Hospital on January 22, 2014 with complaints of masses protruding from her vagina and anus of 24 months duration. The protrusions started 5 months after a spontaneous unsupervised delivery at home of a live male baby. The concomitant protrusions occurred spontaneously. They were usually noticed while straining, sneezing, coughing or in standing position, but often receded spontaneously while in a recumbent position. There was associated low back pain, urinary frequency, and constipation. There was no chronic cough, weight lifting, dysuria, abdominal swelling, or similar family history. About 6 months prior to the presentation, the condition became associated with weight loss and difficulty in holding her stool. The vaginal protrusion no longer receded spontaneously in recumbent position and then required manual reduction. On examination, she appeared generally well. There were no abnormal findings on the examination of the chest, abdomen, central nervous system, and the musculoskeletal system. Pelvic examination showed a protrusion of the entire uterus from the vagina. The protrusion was reducible with associated mild cystocele [Figure 1]. There was no demonstrable stress incontinence. The cervix was healthy looking and the os was parous. The uterus was normal sized, retroverted, and mobile. The adnexa were free. Rectal examination showed a concomitant mass (rectum) protruding from the anus [Figure 2]. There was associated fecal incontinence, but the rectal mucosa was normal. A diagnosis of concomitant occurrence of uterovaginal prolapse (procidentia) and rectal prolapse was made. The hemoglobin concentration, white cell count, urinalysis, culture of her midstream urine, stool analysis and culture, and abdominopelvic ultrasound showed no abnormality. In view of her parity and desire to retain her reproductive function, she and her husband were counseled for open abdominal sacrohysteropexy with synthetic mesh and rectopexy, which they consented to. Following the above investigation results which were available within 2 weeks from her first clinic visit, she was admitted into the ward for the above surgery. While in the ward, she was reviewed by the general surgeons who commenced her on a 1-day mechanical bowel preparation alongside with antibiotics bowel preparation, using the oral neomycin and metronidazole for antibiotics bowel preparation. She had an overnight fasting prior to the day of surgery and was placed on intravenous fluid (normal saline) to ensure adequate rehydration. She received intravenous ceftriaxone and metronidazole as preoperative antibiotics medication. She subsequently had a successful surgery done by a combined team of gynecologists and general surgeons. The surgical procedure briefly involved a general anesthesia/endotracheal intubation; peritoneal cavity entered via a midline sub-umbilical incision; synthetic mesh sutured to the back of the cervix with the other end sutured to a prominent part of sacral promontory (sacrohysteropexy); rectum lifted and sutures taken to secure the sides to the sacrum with a synthetic mesh that provided added reinforcement (rectopexy).
The postoperative period was uneventful and she is being follow-up in the gynecologic clinic. Her last clinic visit, before this report was on June 30, 2014; she had no complaint and was happy with the procedure.
Discussion
Concomitant uterovaginal and rectal prolapse is an uncommon occurrence. Fewer than 100 cases of concomitant genital and rectal prolapse have been reported. [1] Uterine procidentia and rectal prolapse as diagnosed in this case implies the descent of the entire uterus outside the vulva and protrusion of a part or all of the rectum beyond the anus. [3] This case is unique because it occurred in a woman, who has not completed her desired family size.
Genital organ prolapse and rectal prolapse may co-exist, because each of them is a part of pelvic floor disorders. [7] The etiology of concomitant prolapse in this patient was probably multifactorial. Besides the possibility of genetic predisposition, her previous prolonged labor and unsupervised home delivery could be contributory. There might have been injury to the levator ani especially the puborectalis with associated alteration of the pelvic floor muscle integrity and the consistency of the endopelvic connective tissue, thereby precipitating prolapse of the uterus. Rectal prolapse is often associated with pelvic floor disorders including constipation and fecal incontinence, [7] as observed in the case reported. Uterine procidentia on the other hand is commonly associated with urinary tract infection, stress incontinence, or other forms of incontinence. [8] However, none was observed in the index case.
The options of treatment could be surgical or medical. The surgical option could be conservative or nonconservative with respect to preservation of reproductive function. The nonsurgical option available includes the use of ring pessary, but could not be offered to this patient because of the concurrent occurrence of uterovaginal and rectal prolapse. The selection of a surgical approach for uterine prolapse depends on the patient’s age, desire for pregnancy or preservation of vaginal function, the degree of prolapse, and the presence of other associated conditions such as cystocele, stress incontinence, enterocele, and rectocele. [8] The patient had an abdominal sacrohysteropexy and rectopexy because of her desire to retain their uterus for psychological or biological purposes. [1,5] The other conservative surgical option available in this environment, for the patient, includes the Manchester-fothergill operation. However, the popularity of this procedure is waning globally because of the associated complications including infertility, increased risk of cervical incompetence and mid trimester abortions, premature labor, and cervical dystocia. Vaginal hysterectomy and pelvic floor repair are a nonconservative surgical option for uterine procidentia. Though the procedure is curative, [9] it was not appropriate for the patient because she had the desire to preserve her reproductive function. [6] Laparoscopic uterine sling suspensions is a new and effective technique of uterine suspension in women desiring surgical management of uterine prolapse with the uterine conversation. [9,10] Unfortunately, such facilities and expertise are yet to develop in Nigeria.
Conclusion
In resource-limited settings with concomitant uterine and rectal prolapse, open abdominal sacrohysteropexy with synthetic mesh and rectopexy is an effective option in women who desire to preserve the uterus for future reproductive function.
References
- Karateke A, Batu P, Asoğlu MR, Selçuk S, Cam C. Approach to concomitant rectal and uterine prolapse: Case report. J Turk Ger Gynecol Assoc 2012;13:70-3.
- Sun C, Hull T, Ozuner G. Risk factors and clinical characteristics of rectal prolapse in young patients. J Visc Surg 2014;151:425-9.
- Moiety FM, Hegab HM, Ghanem A, Zedah WM, Salem HA. Abdominal Sacrohysteropexy for uterovaginal prolapse: A prospective study on 33 cases. Arch Gynecol Obstet 2010;281:631-6.
- Massey F, Umezurike CC, Eguzo KC. Sacrohysteropexy with synthetic mesh in Aba, South-Eastern Nigeria: A report of three cases and review of the literature. Niger J Clin Pract 2013;16:554-7.
- Demirci F, Ozdemir I, Somunkiran A, Doyran GD, Alhan A, Gul B. Abdominal sacrohysteropexy in young women with uterovaginal prolapse: Results of 20 cases. J Reprod Med 2006;51:539-43.
- Demirci F, Ozdemir I, Somunkiran A, Topuz S, Iyibozkurt C, Duras Doyran G, et al. Perioperative complications in abdominal sacrocolpopexy and vaginal sacrospinous ligament fixation procedures. Int Urogynecol J Pelvic Floor Dysfunct 2007;18:257-61.
- Peters WA 3rd, Smith MR, Drescher CW. Rectal prolapse in women with other defects of pelvic floor support. Am J Obstet Gynecol 2001;184:1488-94.
- Dim CC, Umeh UA, Ezegwui HU, Ikeme AC. Uterine procidentia in an African adolescent: An uncommon gynecological challenge. J Pediatr Adolesc Gynecol 2008;21:37-9.
- Detollenaere RJ, den Boon J, Stekelenburg J, Alhafidh AH, Hakvoort RA, Vierhout ME, et al. Treatment of uterine prolapse stage 2 or higher: A randomized multicenter trial comparing sacrospinous fixation with vaginal hysterectomy (SAVE U trial). BMC Womens Health 2011;11:4.
- Cutner A, Kearney R, Vashisht A. Laparoscopic uterine sling suspension: A new technique of uterine suspension in women desiring surgical management of uterine prolapse with uterine conservation. BJOG 2007;114:1159-62.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.