Conservative Management of Twisted Ischemic Adnexa in Early Pregnancy
Citation: Mathew M, Mubarak SA, Jesrani SK. Conservative management of twisted ischemic adnexa in early pregnancy. Ann Med Health Sci Res 2015;5:142-4.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Diagnosis of adnexal torsion can be difficult, especially during pregnancy. Delay in diagnosis can lead to necrosis and loss of the affected ovary compromising the reproductive capacity, especially in young women. A 22‑year‑old primigravida presented to the emergency room at 10 weeks of gestation with acute onset left iliac fossa pain. Ultrasound examination showed a live intra‑uterine gestation of 10 weeks, enlarged and edematous left ovary with a clear cyst of 76 mm × 63 mm with flow to the ovary. She underwent emergency surgery with a provisional diagnosis of torsion of left adnexa. Mini‑laparotomy, detorsion of the twisted adnexa and ovarian cystectomy with reconstruction was performed thus conserving the tube and ovary. The pregnancy progressed normally; follow‑up ultrasound scans showed normal functioning ovaries. Clinical appearance of torted adnexa does not correlate well with the residual function. Ovarian function can be preserved by untwisting, even if ovary appears necrotic.
Keywords
Adnexal torsion, Detorsion, Magnetic resonance imaging, Pregnancy, Ultrasound
Introduction
Adnexal torsion is the 5th most common gynecological emergency. [1] Diagnosis of torsion can be difficult as the clinical presentation varies. Delay in diagnosis can lead to necrosis and loss of the affected ovary compromising the reproductive capacity. Removal of the ovary containing the corpus luteum in early pregnancy may lead to miscarriage. Hence, conservation of adnexa should be the aim when managing twisted adnexa in young women especially in early pregnancy. We can safely preserve the ovarian function by untwisting and conserving the affected adnexa even when it appears dark purple or blackish. [2] Our case illustrates the successful outcome of pregnancy in a woman who underwent untwisting and conservation of necrotic-looking adnexa in the first trimester of pregnancy.
Case Report
A 22-year-old primigravida presented to the emergency room at 10 weeks gestation with acute onset left iliac fossa pain of 1 day duration. The Pain was colicky in nature and radiated to the left loin. It was associated with nausea. The patient was rolling in pain and there was tachycardia, but the temperature and blood pressure were normal. Abdominal examination revealed a vague mass in the left iliac fossa with marked tenderness. Her hemoglobin was 12.6 g/dL, white cell count 7.7 × 109/L and C-reactive protein (CRP) 26 mg/dL.
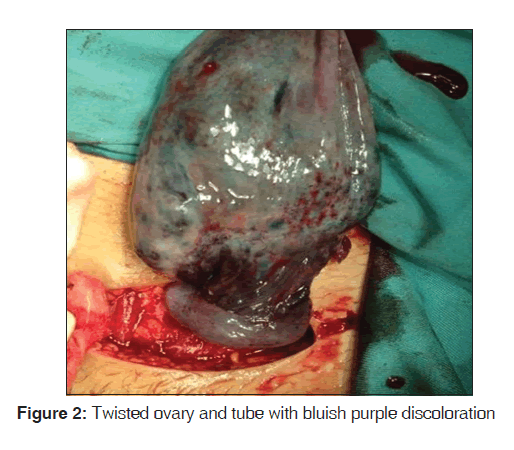
Ultrasound examination showed a single live intra-uterine fetus of 10 weeks gestation, an enlarged and edematous left ovary with a clear cyst of 76 mm × 63 mm with flow to the ovary [Figure 1]. The right ovary appeared normal.
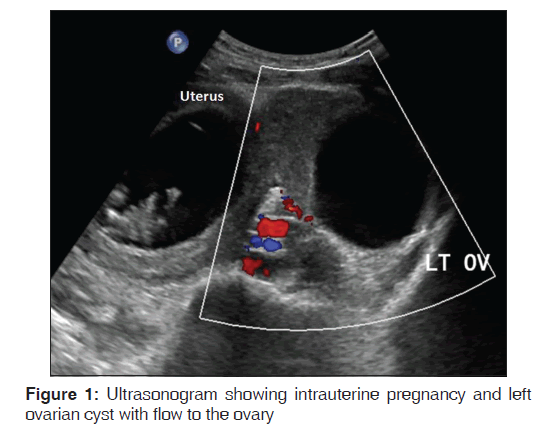
With a provisional diagnosis of left adnexal torsion in pregnancy, she was taken up for emergency surgery. Mini-laparotomy was performed through a suprapubic transverse incision; straw colored fluid was noticed in the peritoneal cavity, the left adnexa was delivered through the abdominal incision to improve the access and it was twisted twice on its pedicle, the left ovary and tube were blackish, edematous and congested [Figure 2]. The cyst had ruptured during manipulation, and it drained blood stained fluid. The uterus was 10 weeks in size, and the right adnexa was grossly normal.
On detorting the twisted adnexa, the tube regained its color and became pink, the ovary also began to regain its color slowly. Ovarian cystectomy with reconstruction and conservation of the left fallopian tube and ovary was performed. Postoperatively the patient received 17 alpha hydroxy progesterone caproate 250 mg intramuscularly weekly × 4 weeks (Proluton depot) as progestogen support for the pregnancy. The pregnancy progressed normally, and the patient had a spontaneous vaginal delivery at term of a live baby girl that weighed 2700 g. Follow-up ultrasound scans and Doppler studies showed flow to the ovary and developing follicles indicating normal functioning ovary.
Discussion
Adnexal torsion is defined as total or partial rotation of adnexa around its vascular pedicle resulting in ischemia. The incidence of simple or complex ovarian cyst in pregnancy is reported as 5–8% , of which 1–3% can undergo torsion. [1] Torsion is more common in prepubertal girls, during pregnancy and puerperium due to the laxity of tissues. The usual presentation is with acute onset pelvic pain, nausea, vomiting, tachycardia and low-grade fever. Atypical presentation can lead to mis-diagnosis or delay in diagnosis, resulting in the loss of ovarian function in many cases. [2]
The ultrasound appearance of adnexal torsion is highly variable. The usual appearance is a unilateral ovarian enlargement with edema and peripherally arranged follicles. The affected ovary may appear as a mixed echogenic mass. [3] Comparison with the normal ovary shows a clear difference in the appearance. As stated in Vijayaraghavan’s study “ the twisted pedicle may be seen as a “whirlpool” in grey scale and color Doppler and has been shown to increase the diagnostic sensitivity.” [4] Abnormal Doppler signals are noted in most of the cases of adnexal torsion. Absence of Doppler signals may be a late sign and presence of signals within the ovary does not exclude ovarian torsion. [5] In our case, the flow to the ovary was present, but there was no flow within the ovary itself.
Computed tomography and magnetic resonance imaging (MRI) are useful in the diagnosis of ovarian torsion in 2nd and 3rd trimesters of pregnancy where the ovaries are difficult to visualize by routine ultrasound. [6]
Various inflammatory markers have been reported to aid in the diagnosis of ovarian torsion but had low sensitivity and specificity. CRP is raised in the presence of inflammation, while the white cell count is raised in 50% of cases of torsion that is nonspecific. [5] Our patient was afebrile and had normal white cell count and mildly raised CRP.
In the past, adnexal torsion was treated by oophorectomy or salpingo-oophorectomy without prior detorsion, due to fear of embolus migration from the twisted pedicle causing infarction and sepsis and also a possible risk of repeat torsion. As there is no embolic incident reported in recent literature and clinical appearance of torted adnexa does not correlate well with the residual function, ovarian conservation is the current trend regardless of the color of the ovary at the time of surgery. [2,7]
There are many reports about conservative management of ovarian torsion with untwisting of the torted adnexa with minimal morbidity and recovery of ovarian function even if ovary appears dark purple or black. [8,9]
Although the role of oophoropexy after detorsion is not clear, it is mostly recommended in patients with recurrent torsion or children and adolescents with torsion of normal ovary. [10]
Laparoscopic route is the preferred method of detorsion with less postoperative pain, analgesia requirement and hospital stay, however, the route is determined by the availability of resources, skill of the operator and patient’s suitability.
Conclusion
The diagnosis of ovarian torsion requires a meticulous approach – adequate history, examination and investigation with a high index of suspicion. Ultrasound remains the first line of investigation; however MRI may be more useful in second and third trimester of pregnancy. Clinical appearance of the twisted adnexa does not correlate well with the residual function. Ovarian function can be safely preserved by untwisting and observing for the clinical reperfusion, even if it appears necrotic initially.
REFERENCES
- Oelsner G, Shashar D. Adnexal torsion. Clin Obstet Gynecol 2006;49:459-63.
- Damigos E, Johns J, Ross J. An update on the diagnosis and management of ovarian torsion. The Obstetrician and Gynecologist 2012;14:229-36.
- Smorgick N, Maymon R, Mendelovic S, Herman A, Pansky M. Torsion of normal adnexa in postmenarcheal women: Can ultrasound indicate an ischemic process? Ultrasound Obstet Gynecol 2008;31:338-41.
- Vijayaraghavan SB. Sonographic whirlpool sign in ovarian torsion. J Ultrasound Med 2004;23:1643-9.
- Shadinger LL, Andreotti RF, Kurian RL. Preoperative sonographic and clinical characteristics as predictors of ovarian torsion. J Ultrasound Med 2008;27:7-13.
- Eskandar O, Eckford S, Watkinson T. Safety of diagnostic imaging in pregnancy. Part 2: Magnetic resonance imaging, ultrasound scanning and doppler assessment. Obstet Gynecol 2010;12:171-7.
- Descargues G, Tinlot-Mauger F, Gravier A, Lemoine JP, Marpeau L. Adnexal torsion: A report on forty-five cases. Eur J Obstet Gynecol Reprod Biol 2001;98:91-6.
- Oelsner G, Cohen SB, Soriano D, Admon D, Mashiach S, Carp H. Minimal surgery for the twisted ischaemic adnexa can preserve ovarian function. Hum Reprod 2003;18:2599-602.
- Mathew M. Untwisting and fixation of ovarian torsion in early pregnancy. JABHS 2008;9:65-7.
- Fuchs N, Smorgick N, Tovbin Y, Ben Ami I, Maymon R, Halperin R, et al. Oophoropexy to prevent adnexal torsion: How, when, and for whom? J Minim Invasive Gynecol 2010;17:205-8.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.