Demographic Analysis of Benign Paroxysmal Positional Vertigo as a Common Public Health Problem
- *Corresponding Author:
- Prof. Sertac Yetiser
Department of ORL and HNS, Anadolu Medical Center, Kocaeli, Turkey.
E-mail: syetiser@yahoo.com
Abstract
Background: Benign paroxysmal positional vertigo (BPPV) is the most common peripheral vestibular problem. However, demographic analysis is few. Aim: The aim of this study was to document the demographic data of patients with BPPV regarding distribution of gender, age, associated problems, most common form, symptom duration, severity of nystagmus and cure rate. Subjects and Methods: A total of 263 patients with video‑nystagmography confirmed BPPV were enrolled in this retrospective study (2009‑2013). The data were collected in Anadolu Medical Center. Distribution of gender, age and affected side were reviewed. Associated problems were noted. Patients were analyzed according to the canal involvement, age, duration of symptoms, duration of nystagmus and recurrence. Mean values and standard deviations were calculated. One‑way ANOVA test was used for the analysis of the data (Statistical Package for the Social Sciences 17.0 version, IBM, Chicago, III, USA). Statistical significance was set at P < 0.05. Results: Women were affected more frequently than men (1:1.5). Comparative analysis of average age between the two gender groups was not statistically significant (P = 0.84). BPPV was common at middle age group. The incidence of affected side was not significant (P = 0.74). Posterior canal‑BPPV (PC‑BPPV) was the most leading one (129/263; 49%) followed by lateral canal (LC)‑canalolithiasis (60/263; 22.8%), LC‑cupulolithiasis (38/263; 14.5%) and superior canal‑BPPV (9/263; 3.4%). 55.1% of patients were defined as idiopathic (145/263). Associated problems were migraine (31/263; 11.8%), trauma (19/263; 7.2%), inner ear disorders (18/263; 6.8%) and other systemic problems (50/263; 19.1%). 72.6% of patients had symptoms <2 months (191/263). 23,6% of patients had intensive nystagmus lasting more than a minute regardless of canal involvement (62/263). 33% of patients required two or more maneuvers for the relief of symptoms (87/263). Conclusion: Symptoms are prone to recur in those of traumatic origin, associated inner ear problems and systemic disorders. As the prognostic factors are illuminated, preventive measures will be more effective and more patients will be cured properly.
Keywords
Benign paroxysmal positional vertigo, Nystagmus, Semicircular canal
Introduction
Benign paroxysmal positional vertigo (BPPV) is the most common peripheral vestibular problem seen at emergency units and outpatient clinics of neurology and otolaryngology. Pathophysiological mechanism that induces the sense of vertigo is well documented.[1] Freely floating otoconia inside the semicircular canals or those adhering to the cupula can provoke nystagmus and vestibular disturbance during sudden head motion.[2] The origin of these deposits is claimed to be the utricular neuroepithelium. Once, the cure was limited to only vestibular exercises and physical therapies. Treatment of patients with BPPV by way of maneuvers has been possible systematically since the clinical contribution of Epley and Semont.[3,4] However, the underlying cause for the detachment of the otoconia is still obscure. Associated problems and demographic aspects of this disturbance as a common public health problem have been less analyzed. The aim of this study is to document the demographic aspects of 263 patients with BPPV regarding distribution of gender, age, associated problems, most common type, symptom duration, severity of nystagmus and cure rate.
Subjects and Methods
A total of 263 patients with BPPV who have been evaluated between 2009- and 2013 during outpatient clinical visit were enrolled in this retrospective study. The data were collected in Anadolu Medical Center, Department of Otolaryngology. A verbal and a signed informed consent were obtained from each patient. The procedures were in accordance with the ethical standards of the declaration of Helsinki and of the institutional review board. Distribution of gender, age and affected side was reviewed. Associated problems were noted. Those who have no clear event-related problem were accepted as “idiopathic.” Patients were grouped as those with posterior canal BPPV (PC-BPPV), lateral canal BPPV (LC-BPPV), whether cupulolithiasis or canalolithiasis, and superior canal BPPV (SC-BPPV). Patients were also grouped as those younger than 30 years of age, those 31-50 years old and those over 51 to understand the distribution of age. Patients were also classified as those who had symptoms <2 months and those with symptoms over 2 months to see the time interval between the beginning of symptoms and the patient’s demand for cure. Patients were also grouped as those with nystagmus lasting more than a minute and those with less enduring nystagmus to understand how severe their disturbance at first admission and finally, as a whole to understand the cure rate for BPPV, patients were grouped as those with recurrent and non-recurrent symptoms. Patients with bilateral or multiple canal involvement were grouped as pluricanalar BPPV. All patients were tested with video-nystagmography (Micromedical Technologies, Inc, USA) for the accuracy of diagnosis.
Diagnosis of LC-BPPV was based on medical history and the presence of geotropic or apogeotropic nystagmus (bi-directional, horizontal) during head-roll maneuver. Affected side for LC-BPPV was determined according to the severity of nystagmus which was severe on the affected side in patients with geotropic nystagmus and was severe on the healthy side in patients with apogeotropic nystagmus. Patients with geotropic nystagmus during head-roll maneuver (McClure/Pagnini) were defined as “LC-canalolithiasis” and patients with apogeotropic nystagmus during head-roll maneuver were defined as “LC-cupulolithiasis” at initial diagnosis for the aim of classification although patients with debris very close to the cupula are also known to present apogeotropic nystagmus. Diagnosis of PC-BPPV was based on medical history and the presence of clockwise (for the left ear) or counter-clockwise (for the right ear) rotatory torsional and up-beating nystagmus during head-hanging maneuver (Dix/Hallpike) when the affected ear is down. Diagnosis of SC-BPPV was based on medical history and the presence of ipsilateral tortional down-beating rotatory nystagmus when the affected ear is down or counter lateral tortional down-beating rotatory nystagmus when the affected ear is up during the head-hanging maneuver with the prevalence of the vertical component. Therefore, inclusion criteria were based on diagnosis of BPPV only and the presence of latency, adaptation and habilitation of transient nystagmus associated with a brief and intense sense of vertigo were noted in all patients. Patients with PC-BPPV were treated with Epley maneuver. Patients with LC-BPPV were treated with Semont, Gufoni or barbeque maneuvers. Patients with SC-BPPV were treated with reverse Epley maneuver or vestibular exercises. Mean values and standard deviations were calculated. One-way ANOVA test was used for multiple variance analysis of the data (Statistical Package for the Social Sciences 17.0 version, IBM, Chicago, III, USA). Statistical significance was set at P < 0.05.
Results
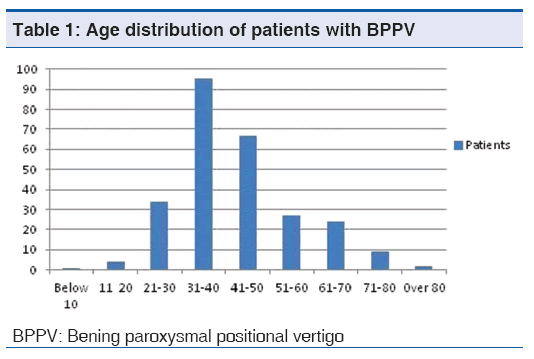
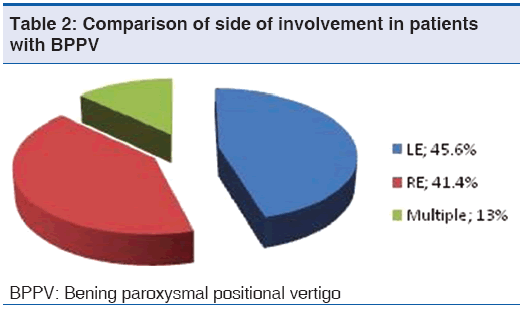
There were 104 men and 159 women (1:1.5). The number of women with BPPV was 1.5 fold more than that of men. Age was ranging between 10 years and 84 years, 42.76 (13.54). Comparative analysis of average age between the two gender groups was not statistically significant, male; 43.06 (13.02), female; 42.42 (13.89), (P = 0.84). The age of distribution is presented on Table 1. BPPV was quite rare under 20 years and it was the most common one at middle age group, 31-50 years. The incidence was lower in patients over 70 years [Table 1]. One hundred and eleven patients had right-sided (111/263; 41.4%), 120 patients had left-sided problem (120/263; 45.6%). The difference was not statistically significant (P = 0.74). It was not possible to identify the affected side due to multiple canal involvement or in some patients with LC-BPPV due to equal severity of nystagmus on both sides in 13% of patients (32/263) [Table 2].
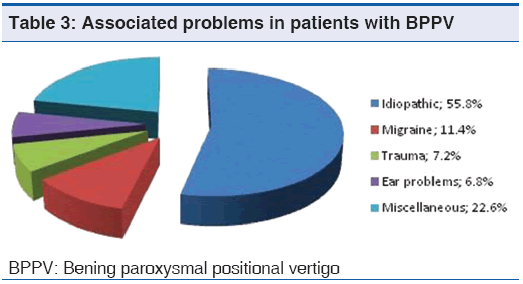
One hundred and twenty-nine patients had PC-BPPV (129/263; 49%), 60 patients had LC-canalolithiasis (60/263; 22.8%), 38 patients had LC-cupulolithiasis (38/263; 14.5%), 9 patients had SC-BPPV (9/263; 3.4%) and 11 patients had nystagmus in both Dix-Hallpike and head-roll maneuvers. Sixteen patients had nystagmus on both sides during Dix-Hallpike maneuver (27/263; 10.3%). PC-BPPV was apparently most leading one followed by LC-canalolithiasis. One hundred and forty-five patients were defined as “idiopathic” since they didn’t have any associated or event-related problem (145/263; 55.1%). Thirty-one patients had migraine (31/263; 11.8%). Nineteen patients had an evident story of trauma (19/263; 7.2%). Ten patients had vestibular neuritis prior to BPPV, 5 patients had Meniere’s disease and 3 patients had otosclerosis (18/263; 6.8%). Goiter, hypertension, high cholesterol, diabetes, gastric ulcer, osteoarthritis, cancer (lymphoma, thyroid and breast cancers etc), chronic coronary and lung diseases were the other miscellaneous problems (50/263; 19.1%) [Table 3]. One hundred and ninety-one patients had symptoms <2 months (191/263; 72,6%). Sixty-two patients (62/263; 23,6%) had intensive nystagmus lasting more than a minute regardless of canal involvement. Eighty-seven patients (87/263; 33%) required two or more maneuvers for the relief of symptoms.
Discussion
Causative factors that can be related with BPPV are still not quite clear. The role of aging as an etiological factor has been proposed. Ischemia and vascular damage, the incidence of which increases progressively with age, have been claimed although this disorder can affect eventually all age groups. Faralli et al. have investigated hypertension, hyperglycemia, and hyperlipidemia in 566 patients with BPPV and have found no difference between those under 50 and those over 50 years of age.[5] BPPV is known to be a disease of the elderly population. But more recently, it occurs across all age groups.[6] We have found an increased incidence of BPPV at middle age groups. This might be due to growing awareness of the problem and widespread use of diagnostic maneuvers. Associated problems were evident in 22.6% of patients and inner ear problems were found to be in 6.8% of patients in this series. Co-existence of Meniere’s disease and BPPV has been reported to be 5.5-10%.[6]. It is important to explore the problems associated with BPPV since it has been reported that especially those with inner ear disease have long treatment duration and higher recurrence when compared to those defined as idiopathic.[6-8]
Females were found to be affected more frequently. This is a common finding in several studies and females have more psychiatric disorders associated with BPPV like depression, demoralization, phobia and anxiety.[9] No predilection of side was observed in this series. On the other hand, Von Brevern et al. have found that BPPV affects predominantly the right labyrinth. They have reported that most patients had the habit of sleeping on their right side.[10] Most recently, a significant correlation has been found between head position during sleep and the side affected by BPPV.[11,12] Co-existence of BPPV with long-standing ipsilateral severe hearing loss might also be due to sleeping habit of the patients since most people desire to sleep on the side with hearing loss to keep the hearing side in the open environment. Trauma was evident in 7.2% of patients. Presence of trauma, as a factor, is probably under-estimated since most patients describe important events only. However, it has been reported that minor head trauma during daily life such as mountain biking; long journey by bus or airplane, roller-skating in amusement park, intense physical activity and dental treatment may provoke BPPV.[13-15] One of the interesting finding in our series is the co-existence of migraine and BPPV in 11.4% of patients which has to be investigated in detail in further studies.
Posterior canal-BPPV was the most common type, followed by other two versions of the LC-BPPV in which the crystalloid debris are in the anterior arm or in cupula in apogeotropic form and in the posterior arm in the geotropic form. The incidence of SC-BPPV was very low. Diagnosis of PC-BPPV is quite straightforward with ipsilateral head-hanging maneuver. However, the test could be positive on both sides, that may be due to pseudo effect on counter LC. Therefore, it is important to treat the more intensive side first, which will result in complete relief of symptoms. On the other hand, diagnosis of the affected side in patients with LC-BPPV could be difficult if the provoked nystagmus has equal intensity on both sides or is too weak to justify. The “head bow and lean test” is helpful to decide for the affected side.[16] Multiple canal involvement, which can be detected on both head-hanging and roll-on tests, is usually more common in those who had a history of trauma and presents a challenge for the treatment. Eighty-seven patients (33%) required two or more attempts of therapeutic maneuvers for the relief of symptoms in this series. This is an important finding in terms of public health since almost one-third of BPPV patients will have a recurrence of symptoms.
Diagnosis of patients with BPPV is easy and quick after head-roll and head-hanging diagnostic maneuvers. Intense, paroxysmal positional nystagmus is characteristic. Provoked vertigo is rarely distressing and long-lasting. Treatment is simple, safe and highly effective. However, it should be kept in mind that the symptoms are prone to recur in those with traumatic origin, in those with associated inner ear problems and in those with systemic disorders.[17-19] In conclusion, demographic and prognostic studies will enlighten all aspects of this common vestibular problem and will give new insights for proper cure and preventive measures like changing sleeping habit or searching of BPPV in every patient with balance problem following even mild trauma.
Acknowledgements
Authors declare that they do not have any fund for the preparation of the manuscript. They would like to thank to all personnel of the department for their support helping the patients.
References
- Balatsouras DG, Koukoutsis G, Ganelis P, Korres GS, Kaberos A. Diagnosis of single- or multiple-canal paroxysmal positional vertigo. Int J Otolaryngol 2011;2011:483965.
- Parnes LS, McClure JA. Free floating endolymph particles. A new operative finding during posterior semicircular canal occlusion. Laryngoscope 1992;102:989-92.
- Epley JM. The canalith repositioning maneuver for treatment of benign paroxysmal positional vertigo. Otolaryngol Head and Neck Surg 1995;112:688-90.
- Semont A, Freyss G, Vitte E. Curing the BPVV with a liberatory maneuver. Adv Otorhinolaryngol 1988;42:290-3.
- Faralli M, Ricci G, Molini T, Bressi T, Simoncelli C, Frenguelli A. Paroxysmal positional vertigo: The role of age as a prognostic factor. Acta Otorhinolaryngol Ital 2006;26:25-31.
- Gross EM, Ress BD, Virre ES, Nelson JR, Harris JF. Intractable benign paroxysmal positional vertigo in patients with Meniere’s disease. Laryngoscope 2000;110:655-9.
- Lee NH, Ban JH, Lee KC, Kim SM. Benign paroxysmal positional vertigo secondary to inner ear disease. Otolaryngol Head Neck Surg 2010;143:413-7.
- Tanimoto H, Doi K, Nishikawa T, Nibu K. Risk factors for recurrence of benign paroxysmal positional vertigo. J Otolaryngol Head Neck Surg 2008;37:832-5.
- Hagr A. Comorbid psychiatric conditions of benign paroxysmal positional vertigo. Int J Health Sci (Qassim) 2009;3:23-8.
- Von Brevern M, Seelig T, Neuhauser H, Lempert T. Benign paroxysmal positional vertigo predominantly affects the right labyrinth. J Neurol Neurosurg Psychiatry 2004;75:1487-8.
- Sato G, Sekine K, Matsuda K, Takeda N. Effects of sleep position on time course in remission of positional vertigo in patients with benign paroxysmal positional vertigo. Acta Otolaryngol 2012;132:614-7.
- Shim DB, Kim JH, Park KC, Song MH, Park HJ. Correlation between the head-lying side during sleep and the affected side by benign paroxysmal positional vertigo involving the posterior or horizontal semicircular canal. Laryngoscope 2012;122:873-6.
- Vibert D, Redfield RC, Hausler R. Benign paroxysmal positional vertigo in mountain bikers. Ann Otol Rhinol Laryngol 2007;116:887-90.
- Giacomini PG, Ferraro S, Di Girolamo S, Villanova I, Ottaviani F. Benign paroxysmal positional vertigo after intense physical activity: A report of nine cases. Eur Arch Otorhinolaryngol 2009;266:1831-5.
- Chiarella G, Leopardi G, De Fazio L, Chiarella R, Cassandro E. Benign paroxysmal positional vertigo after dental surgery. Eur Arch Otorhinolaryngol 2008;265:119-22.
- Califano L, Melillo MG, Mazzone S, Vassallo A. Secondary signs of lateralization in apogeotropic lateral canal canalolithiasis. Acta Otorhinolaryngol Ital 2010;30-78-86.
- Gordon CR, Levite R, Joffe V, Gadoth N. Is posttraumatic benign paroxysmal positional vertigo different from idiopathic form. Arch Neurol 2004;61:1590-3.
- Balatsouras DG, Ganelis P, Aspris A, Economou NC, Moukos A, Koukoutsis G. Benign paroxysmal positional vertigo associated with Meniere’s disease: Epidemiological, pathophysiologic, clinical and therapeutic aspects. Ann Otol Rhinol Laryngol 2012;121:682-8.
- De Stefano A, Dispenza F, Suarez H, Perez-Fernandez N, Manrique-Huarte R, Ban JH et al. A multicenter observational study on the role of co-morbidities in the recurrent episodes of benign paroxysmal positional vertigo. Auris Nasus Larynx 2014;41:31-6.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.