Dental Caries Experience in Children with Down Syndrome
2 Department of Pediatric and Preventive Dentistry, Saveetha dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences (SIMATS), Chennai, India, Email: mebingeorgem.sdc@saveetha.com
Received: 29-Jul-2021 Accepted Date: Aug 05, 2021 ; Published: 24-Dec-2021
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Oral health in Down Syndrome (DS) children has some peculiar aspects that must be considered in the follow-up of these patients. The objective of the present study was to assess the prevalence of dental caries and treatment needs among children with Down syndrome. Case records of patients who visited the department of pediatric and preventive dentistry at a private dental hospital from June 2019 to March 2020. 17 patients who fulfilled the inclusion and exclusion criteria were included in the study. The data was analysed through chi square. It was observed that all the children with Down syndrome had dental caries and mean dmft score was 4. Out of 17 children, all were reported to have dental caries with maximum prevalence in the age group 6-10 years and slightly more in males than females (p>0.05). Within the limitations of this study, it was concluded that prevalence of dental caries is high in children with Down syndrome.
Keywords
Caries experience; Down syndrome; Dental caries
Introduction
Introduction
Down syndrome (DS) is an autosomal chromosomal disorder caused by trisomy of all or a critical part of chromosome 21. [1–3] DS affects approximately 1 in 600-700 live births globally. [4–6] DS has also been referred to by the terms Trisomy 21, Trisomy G or Mongolism. [7–9] Clinically, it is characterized by generalized hypotonia, neurological changes, structural cardiomyopathy, respiratory problems and a greater risk of infection, dental anomalies and orofacial dysmorphology, which therefore requires special attention in the dental treatment of these patients. [10–13]
Caries is the most common chronic disease of childhood and can have a direct and devastating impact on the patients’ overall health, especially for those with certain systemic health problems. [14,15] Caries is a multifactorial infectious disease and there are a lot of different factors that affect its occurrence.
DS is one of the most common genetic abnormalities and has a highly variable prognosis. Individuals with DS have specific orofacial characteristics associated with the syndrome/the most common oral problems encountered included, periodontal disease, malocclusion, mouth breathing, macroglossia, delayed teeth eruption, multiple missing teeth and malformed teeth, microdontia, diastema and bruxism. [16,17] DS patients have specific characteristics in the head and neck area. The most noticeable characteristics include bracheocephaly, thin cranium with delayed closure of the fontanelles, fine and thin hair, frontal bossing, blocked tear ducts, small and wide nasal bridge, hypotonia of muscles with predisposition to retain the mouth open and tongue protruded, deficiency in the midface, short neck, abnormally sized or missing earlobes, loss of hearing ability that might be a resultant of fluid buildup in middle ear and atlantoaxial instability that might lead to dislocation. [18] Scientific evidence of susceptibility to dental caries in the population with down syndrome is limited and conflicting, making it difficult to establish firm conclusions. [19–21] The vast majority of published studies report a lower prevalence and experience of caries in this group of individuals than in groups not affected by DS and groups with other disabilities.
A smaller number of studies, however, have highlighted an equivalent or higher prevalence of caries in individuals with DS. [22,23] Previously our team has a rich experience in working on various research projects across multiple disciplines. [24–38] Now the growing trend in this area motivated us to pursue this project.
According to these authors, some local factors determinant of caries overrides protective factors. As no published literature is available on the prevalence of caries and treatment needs of Down syndrome children, this study aims to assess dental caries in children with down syndrome.
Materials and Methods
The study was undertaken after ethical approval was obtained from the institutional review boards. Data was retrospectively collected from the case records patients who visited the Department of Pediatric and Preventive Dentistry at a private dental hospital. Patients who had DS and were below 18 years were included in the study. Patients older than 18 years and those with any other disorder were excluded from the study. 17 patients who fulfilled the criteria were included in the study. Simple random sampling was done to minimise the sampling bias. Data verification was done based on the age, gender, dmft score, DMFT score, total caries experience. Data was entered in the excel sheet in a methodical manner and was imported to SPSS. Incomplete or uncensored data was excluded from the study. IBM SPSS 20.0 Software was used for data analysis. Independent variables include –age, gender and dependent variables include DMFT score, dmft score. Descriptive and inferential statistics was used. Inferential test includes the chi-square test.
Results and Discussion
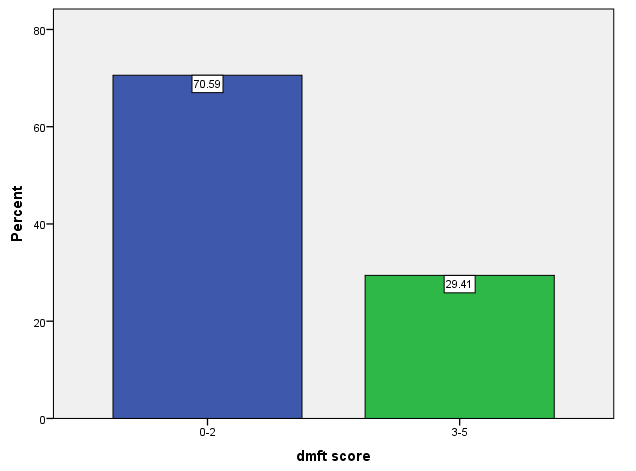
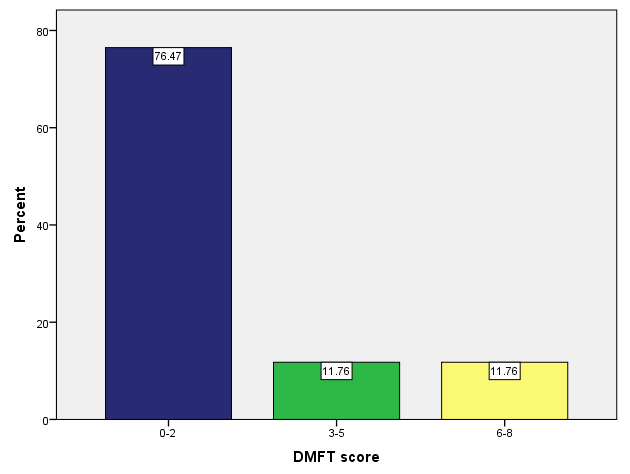
Out of 17 children, all were reported to have dental caries with maximum prevalence in the age group 6-10 years and slightly more in males than females. While observing frequency of dmft score in children with Down syndrome, it was seen that out of 17 patients, 70.59% of the children had a score of 0-2 and 29.41% reported with a score of 3-5 [Figure 1]. While observing frequency of DMFT score in children with Down syndrome, it was seen that out of 17 patients, 76.47% had a score of 0-2, 11.76% reported with a score between 3-5 and 11.76% reported with a score between 6-8 [Figure 2]. Hence, from Figures 1 and 2, it can be seen that permanent teeth are more affected with dental caries than the primary teeth.
Figure 1:The bar chart showing frequency of dmft score in children with Down syndrome. (Blue) bar depicts a dmft score of 0-2 and (green) bar depicts dmft score of 3-5. It shows that 70.59% of children with Down syndrome have dental caries of dmft score 0-2 and 29.41% reported with dmft score of 3-5.
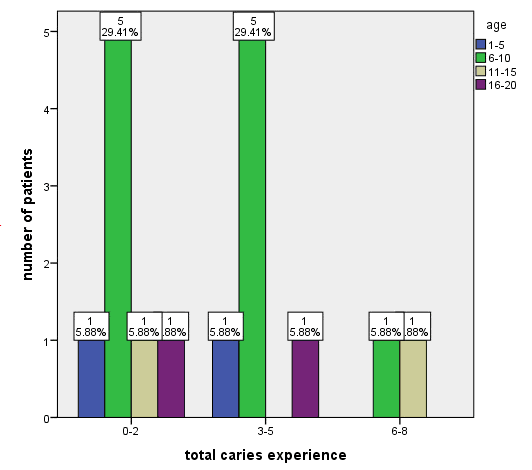
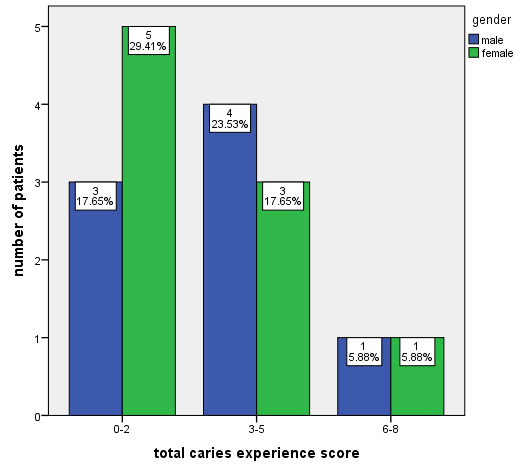
Coming to the age group, the maximum number of children with dental caries is 6-10 years (65%; n=11)) followed by all the other age groups distributed equally 1-5 years (12%; n=2), 11-15 years (12%; n=2) and 16-20 years (12%; n=2) [Figure 3]. Figure 4 shows the gender distribution of down syndromic patients with dental caries. Out of 17 patients, 58% were males and 42% were females where 50% of males had a total dmft score of 3-5 and 55% of females reported with a total dmft score of 0-2. Hence, when comparing both the genders, it was observed that males were slightly more prevalent to dental caries than females.
Figure 3:Bar chart represents the correlation between the age of children with Down syndrome and total dmft score. X-axis represents total caries score and Y-axis represents various age groups. Chi square test shows no significant association, Pearson chi square: 3.988, p=0.678>(0.05) which is statistically non-significant, however it showed that the maximum number dental caries in 6-10year old children when compared to other age groups.
Figure 4:Bar chart represents the correlation between the gender of children with Down syndrome and total caries score. X-axis represents total caries score and Y-axis represents gender where blue bar represents male and green bar represents female. Male represents (blue) and female represents (green). Chi square test shows no significant association, Pearson chi square: 0.586, p=0.746 >(0.05) which is statistically non-significant. It was observed that males were slightly more prevalent to dental caries than females.
The data for this retrospective study was based on residents of Indian origin seeking treatment at a private dental hospital.current scenario of prevalence of dental caries among children with Down syndrome.
In this study, it was observed that all the children with Down syndrome who were screened had dental caries with high prevalence in the age group 6-10 years and slightly more in males than females. Brown and Cunninghan (1961) examined 80 down syndrome children (1-39 years) and found that 44% of the sample was caries free. [39] Barnett et al. revealed that DS children have higher prevalence of periodontitis than dental caries. [40] Study conducted by Morinushi et al. in 1995 to evaluate the incidence of dental caries in 75 down syndrome children in age group 2-18 years. They found that 46.1% of these children with 61.4% of children at the age of 5 years to be caries free. [41]
The findings of our study however, differ from those of the above studies. Our results show that all children with DS have dental caries. The higher incidence of caries could be due to lack of dental visits, irregular diet, inadequate oral hygiene measures, high intake of sucrose containing food, parental negligence and lack of initiative towards prevention. Cornejo et al. studied the oral health conditions of children aged 3-19 years and compared them with control group. In every group, the DMFT and dmft score was higher in DS children than in control group. [23] Also the results of study conducted by Oredulgsa revealed that children with DS had a higher prevalence of dental caries than the controls. The results of the studies of Cornejo etal. were in accordance with the results of the present study. [42] Our institution is passionate about high quality evidence based research and has excelled in various fields. [43–49] We hope this study adds to this rich legacy.
Within the limitations of the current study it shows that children with Down syndrome have high prevalence of dental caries. This suggests the need to spread awareness among dentists in India on the severity of dental caries and new treatment modalities for down syndrome children.
Conclusion
Within the limitations of this study, it can be concluded from this study that children with Down syndrome have a high prevalence of caries and extensive unmet needs of dental treatment. This study also suggests that oral health promotion programs should be introduced to special care schools with parental education as an integral component of such programs.
Author's Contribution
Shanmugam performed the data collection by reviewing patient details, filtering required data, analysing and interpreting statistics and contributed to manuscript writing. Dr. Mebin George contributed to conception of study title, study design, analysed the collected data, statistics and interpretation and critically revised the manuscript. Dr. Suresh V also critically analysed the article. All the authors have discussed the results and contributed to the final manuscript.
Acknowledgement
This research was supported by Saveetha Dental College and Hospital. We thank the department of Pedodontics, Saveetha dental college for providing insight and expertise that greatly assisted this research.
Conflict of Interest
The authors have declared that there is no conflict of interests.
REFERENCES
- Jeevanandan G, Kedo S. Paediatricrotary files for root canal preparation in primary teeth-Case report. J Clin Diagn Res. 2017;11(3):ZR03–5.
- Finn SB, Akin J. Clinical pedodontics. Saunders. 1973;704.
- Govindaraju L, Jeevanandan G, Subramanian EMG. Knowledge and practice of rotary instrumentation in primary teeth among Indian dentists: A questionnaire survey. Int J Oral Health Dent. 2017;9(2):45-48.
- Somasundaram S. Fluoride content of bottled drinking water in Chennai, Tamil Nadu. J Clin Diagn Res. 2015;9(10):ZC32-ZC34.
- Jeevanandan G, Govindaraju L. Clinical comparison of Kedo-S paediatric rotary files vs. manual instrumentation for root canal preparation in primary molars: A double blinded randomised clinical trial. Eur Arch Paediatr Dent. 2018;19: 273–8.
- Govindaraju L, Jeevanandan G, Subramanian E. Clinical evaluation of quality of obturation and instrumentation time using two modified rotary file systems with manual instrumentation in primary teeth. J Clin Diagn Res. 2017;11(9):ZC55–8.
- Ravikumar D, Jeevanandan G, Subramanian EMG. Evaluation of knowledge among general dentists in treatment of traumatic injuries in primary teeth: A cross-sectional questionnaire study. Eur J Dent. 2017;11(2):232–7.
- Panchal V, Jeevanandan G, Subramanian EMG. Comparison of instrumentation time and obturation quality between hand K-file, H-files, and rotary Kedo-S in root canal treatment of primary teeth: A randomized controlled trial. J Indian Soc Pedod Prev Dent. 2019;37(1):75-79.
- Christabel SL, Linda Christabel S. Prevalence of type of frenal attachment and morphology of frenum in children, Chennai, Tamil Nadu. World J Dent. 2015;6(4):203-207.
- Packiri S, Gurunathan D, Selvarasu K. Management of paediatric oral ranula: A systematic review. J Clin Diagn Res. 2017 Sep;11(9):ZE06–9.
- Gurunathan D, Shanmugaavel AK. Dental neglect among children in Chennai. J Indian Soc Pedod Prev Dent. 2016;34(4):364–9.
- Govindaraju L, Gurunathan D. Effectiveness of Chewable Tooth Brush in Children-A Prospective Clinical Study. J Clin Diagn Res. 2017;11(3):ZC31–4.
- Subramanyam D, Gurunathan D, Gaayathri R, Vishnu Priya V. Comparative evaluation of salivary malondialdehyde levels as a marker of lipid peroxidation in early childhood caries. Eur J Dent. 2018;12(1):67–70.
- Ramakrishnan D. Fluoride, fluoridated toothpaste Efficacy andits Safety in Children-Review. Int J Curr Pharm Res.2018;10(4).
- Lakshmanan L, Mani G, Jeevanandan G, Ravindran V, Subramanian EMG. Assessing the quality of obturation and instrumentation time using Kedo-S files, Reciprocating files and Hand K-files. Braz Dent Sci. 2020;23(1).
- Smith DW, Jones KL. Smith’s recognizable patterns of human malformation. Saunders; 1988;778.
- Shrestha BK. Orthodontic treatment of anterior dental open bite with drawbridge effect: A Case Report. Orthod J Nepal. 2013;3:69–72.
- Hennequin M, Allison PJ, Veyrune JL. Prevalence of oral health problems in a group of individuals with Down syndrome in France. Dev Med Child Neurol. 2000;42:691–8.
- Dey S. Health problems in down syndrome. BoD–Books on Demand. 2015;134.
- Fung K, Lawrence H, Allison P. A paired analysis of correlates of dental restorative care in siblings with and without Down syndrome. Spec Care Dentist. 2008;28:85–91.
- Oliveira ACB, Paiva SM, Campos MR, Czeresnia D. Factors associated with malocclusions in children and adolescents with Down syndrome. Am J Orthod Dentofacial Orthop. 2008;133: 489.e1–489.e8.
- Dey S. Prenatal Diagnosis and Screening for Down Syndrome. Intech Open. 2011;246.
- Battellino LJ, Cornejo LS, de Cattoni STD, de Yankilevich ERLM, Calamari SE, Azcura AI, et al. Evaluación del estado de saludbucodental en preescolares: studio epidemiológico longitudinal (1993-1994), Córdoba, Argentina. Revista Saúde Pública. 1997;31:272–81.
- Ponnulakshmi R, Shyamaladevi B, Vijayalakshmi P, Selvaraj J. In silico and in vivo analysis to identify the antidiabetic activity of beta sitosterol in adipose tissue of high fat diet and sucrose induced type-2 diabetic experimental rats. Toxicol Mech Meth. 2019;29(4):276–90.
- Mathew MG, Samuel SR, Soni AJ, Roopa KB. Evaluation of adhesion of Streptococcus mutans, plaque accumulation on zirconia and stainless steel crowns, and surrounding gingival inflammation in primary molars: randomized controlled trial. Clin Oral Investig. 2020;24(9):3275–80.
- Subramaniam N, Muthukrishnan A. Oral mucositis and microbial colonization in oral cancer patients undergoing radiotherapy and chemotherapy: A prospective analysis in a tertiary care dental hospital. J Investig Clin Dent. 2019;10(4):e12454.
- Girija ASS, Shankar EM, Larsson M. Could SARS-CoV-2-Induced hyperinflammation magnify the severity of coronavirus disease (covid-19) leading to acute respiratory distress syndrome? Front Immunol. 2020;27(11):1206.
- Dinesh S, Kumaran P, Mohanamurugan S, Vijay R, Singaravelu DL, Vinod A, et al. Influence of wood dust fillers on the mechanical, thermal, water absorption and biodegradation characteristics of jute fiber epoxy composites. J Polym Res. 2020;27(1).
- Thanikodi S, Singaravelu D Kumar, Devarajan C, Venkatraman V, Rathinavelu V. Teaching learning optimization and neural network for the effective prediction of heat transfer rates in tube heat exchangers. Therm Sci. 2020;24(1B):575–81.
- Murugan MA, Jayaseelan V, Jayabalakrishnan D, Maridurai T, Kumar SS, Ramesh G, et al. Low velocity impact and mechanical behaviour of shot blasted SiC wire-mesh and silane-treated aloevera/hemp/flax-reinforced SiC whisker modified epoxy resin composites. Silicon Chem. 2020;12(8):1847–56.
- Vadivel JK, Govindarajan M, Somasundaram E, Muthukrishnan A. Mast cell expression in oral lichen planus: A systematic review. J Investig Clin Dent. 2019;10(4):e12457.
- Chen F, Tang Y, Sun Y, Veeraraghavan VP, Mohan SK, Cui C. 6-shogaol, an active constiuents of ginger prevents UVB radiation mediated inflammation and oxidative stress through modulating NrF2 signaling in human epidermal keratinocytes (HaCaT cells). J Photochem Photobiol B. 2019;197:111518.
- Manickam A, Devarasan E, Manogaran G, Priyan MK, Varatharajan R, Hsu C-H, et al. Score level based latent fingerprint enhancement and matching using SIFT feature. Multimed Tools Appl. 2019;78(3):3065–85.
- Wu F, Zhu J, Li G, Wang J, Veeraraghavan VP, Krishna Mohan S, et al. Biologically synthesized green gold nanoparticles from induce growth-inhibitory effect on melanoma cells (B16). Artif Cells Nanomed Biotechnol. 2019;47(1):3297–305
- Ma Y, Karunakaran T, Veeraraghavan VP, Mohan SK, Li S. Sesame inhibits cell proliferation and induces apoptosis through inhibition of STAT-3 translocation in thyroid cancer cell lines (FTC-133). Biotechnol Bioprocess Eng. 2019;24(4):646–52
- Ponnanikajamideen M, Rajeshkumar S, Vanaja M, Annadurai G. In vivo type 2 diabetes and wound-healing effects of antioxidant gold nanoparticles synthesized using the insulin plant Chamaecostus cuspidatus in albino rats. Can J Diabetes. 2019;43(2):82–9.e6
- Vairavel M, Devaraj E, Shanmugam R. An eco-friendly synthesis of Enterococcus sp.-mediated gold nanoparticle induces cytotoxicity in human colorectal cancer cells. Environ Sci Pollut Res Int. 2020;27(8):8166–75.
- Paramasivam A, VijayashreePriyadharsini J, Raghunandhakumar S. N6-adenosine methylation (m6A): a promising new molecular target in hypertension and cardiovascular diseases. Hypertens Res. 2020;43(2):153–4
- Brown RH, Cunningham WM. Some dental manifestations of mongolism. Oral Surg Oral Med Oral Pathol. 1961;14:664–76.
- Barnett ML, Kenneth P. Press, Friedman D, Sonnenberg EM. The prevalence of periodontitis and dental caries in a down’s syndrome population. J Periodontol. 1986;57:88–93.
- Morinushi T, Lopatin DE, Van Poperin N. The relationship between gingivitis and the serum antibodies to the microbiota associated with periodontal disease in children with down’s syndrome. J Periodontol.1997;68: 626–31.
- Oredugba F. Oral health condition and treatment needs of a group of Nigerian individuals with Down syndrome. Downs Syndr Res Pract. 2007;12(1), 72-76.
- Vijayashree PJ. In silico validation of the non-antibiotic drugs acetaminophen and ibuprofen as antibacterial agents against red complex pathogens. J Periodontol. 2019;90(12):1441–8.
- Ezhilarasan D, Apoorva VS, Ashok Vardhan N. Syzygium cumini extract induced reactive oxygen species-mediated apoptosis in human oral squamous carcinoma cells. J Oral Pathol Med. 2019;48(2):115–21.
- Ramesh A, Varghese S, Jayakumar ND, Malaiappan S. Comparative estimation of sulfiredoxin levels between chronic periodontitis and healthy patients-A case-control study. J Periodontol. 2018;89(10):1241–8.
- Mathew MG, Samuel SR, Soni AJ, Roopa KB. Evaluation of adhesion of Streptococcus mutans, plaque accumulation on zirconia and stainless steel crowns, and surrounding gingival inflammation in primary. Clin Oral Investig. 2020;24:3275–3280
- Sridharan G, Ramani P, Patankar S, Vijayaraghavan R. Evaluation of salivary metabolomics in oral leukoplakia and oral squamous cell carcinoma. J Oral Pathol Med. 2019;48(4):299–306
- Pc J, Marimuthu T, Devadoss P. Prevalence and measurement of anterior loop of the mandibular canal using CBCT: A cross sectional study. Clin Implant Dent Relat Res. 2018;20(4):531-534.
- Ramadurai N, Gurunathan D, Samuel AV, Subramanian E, Rodrigues SJL. Effectiveness of 2% Articaine as an anesthetic agent in children: randomized controlled trial. Clin Oral Investig. 2019;23(9):3543–50.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.