Depression, Anxiety, and Stress Symptoms in Menopausal Arab Women: Shedding More Light on a Complex Relationship
- *Corresponding Author:
- Prof. Bener A
Department of Biostatistics and Medical Informatics, Cerrahpaşa Faculty of Medicine, Istanbul University, 34098 Cerrahpasa, Istanbul, Turkey.
E-mail: abdulbari.bener@istanbul. edu.tr
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
CitationBener A, Saleh NM, Bakir A, Bhugra D. Depression, anxiety, and stress symptoms in menopausal arab women: Shedding more light on a complex relationship. Ann Med Health Sci Res 2016;6:224-31.
Abstract
Background: The association between depression, anxiety, and stress among Arab menopause and postmenopausal women have been explored in detailed. Aim: The objective of this study was to determine the correlation between depression, anxiety, and stress in menopausal and postmenopausal women and shedding more light on a complex relationship. Subjects and Methods: A cross‑sectional descriptive study was used to generate menopause symptoms experienced by Arabian women at the primary health care centers in Qatar. A representative sample of 1468 women aged 45–65 years were approached during July 2012 and May 2014 and 1101 women agreed to participate (75.0%) and responded to the study. Depression, anxiety, and stress were measured using the Depression Anxiety Stress Scales 21. Data on body mass index (BMI), clinical and other parameters were used. Univariate, multivariate, and matrix correlation analysis were performed for statistical analysis. Results: A total of 1101 women agreed to participate after informed consent was obtained. The mean age and standard deviation (SD) of the menopausal age were 49.55 (3.12), the mean and SD of postmenopausal age was 58.08 (3.26) (P < 0.001). There were statistically significant differences between menopausal stages with regards to age, ethnicity, educational status, occupation status, and place of living. Furthermore, there were statistically significant differences between menopausal stages with regards to BMI, systolic and diastolic blood pressure (BP), Vitamin D deficiency, and diseases. Depression and anxiety were more common among postmenopause women. Furthermore, there were no differences between the groups regarding the frequency of certain levels of stress among menopause and postmenopause. The multivariate regression analyses revealed that age in years, diastolic BP, consanguinity, regular exercise were a predictor for depression. Meanwhile, diastolic BP, occupation, and physical activity considered the main risk factors for anxiety. Furthermore, age in years, occupation, and sheesha smoking habits were considered as the main risk factors associated with stress. Conclusion: A large number of factors were associated with experiencing menopausal and psycho‑social problems and which had negative effects on the quality of life among Arabian women. Depression, anxiety, and stress should be considered as important risk factors for osteoporosis.Keywords
Anxiety, Complex relationship, Depression, Diseases, Menopause, Physical activity, Postmenopausal, Protective factors, Stress (Depression Anxiety Stress Scales 21)
Introduction
Menopause is the cessation of a woman’s reproductive ability, the opposite of menarche and it is usually a natural change; it typically occurs in women in midlife, during their late 40s or early 50s, signaling the end of the fertile phase of a woman’s life.[1-5] The transition from a potentially reproductive to a nonreproductive state is normally not sudden or abrupt, may occur over a number of years, and is a consequence of biological aging.[3-7] Age at natural menopause is an important research issue because of the suspected links between it and risk for certain diseases.[2,5]
Menopause is the cessation of a woman’s reproductive ability, the opposite of menarche and it is usually a natural change; it typically occurs in women in midlife, during their late 40s or early 50s, signaling the end of the fertile phase of a woman’s life.[1-5] The transition from a potentially reproductive to a nonreproductive state is normally not sudden or abrupt, may occur over a number of years, and is a consequence of biological aging.[3-7] Age at natural menopause is an important research issue because of the suspected links between it and risk for certain diseases.[2,5] In the last decade, researchers have begun studying the relationship between menopausal ages and depression, anxiety, and stress.[8-13] Most of these studies have focused on the psychological effects of coping with the disease, including pain, difficulties in ability to function and fractures, which may occasionally require surgery and prolonged rehabilitation.[2-4] Most recent meta-analyses supported a significant correlation of depression, anxiety, and stress with an increase in menopausal age.[5,14] This situation may explain a condition characterized by increase in an individual’s anxiety level.
The reported association between menopausal ages and depression, anxiety, and stress have been controversial.[5-17] The objective of the current study was to determine the correlation between depression, anxiety, and stress in menopausal and postmenopausal women and shedding more light on a complex relationship.
Subjects and Methods
This is a cross-sectional primary health care (PHC) centers based study conducted in the State of Qatar. The survey was conducted among Qatari national and Arab women aged 45–65-year-old. To support the PHC, 22 health centers were established covering all the districts of Qatar to provide health services. Every health center provides PHC services to the people in that surrounding catchment area.
PThe questionnaire had four parts. The first part included the sociodemographic details of the patients, the second part the medical and family history of the patients, the third part was obstetric variables, and the fourth was the diagnostic screening questionnaire. The Depression Anxiety Stress Scales (DASS-21) questionnaire is a quantitative measure of distress on the basis of three subscales of depression, anxiety, and stress.[10,11,18,19] The DASS 21 is a brief 21 item version of the full DASS, which originally consisted of 42 items. Each of the three DASS-21 scales contains seven items representing the dimensions of depression, anxiety, and stress. The DASS consists of three self-report scales that have been designed to measure the negative emotional scales of depression, anxiety and stress. Each question has 3 subscales ranging between 0 and 3 and the rating scale is as follows: 0 for “did not apply to me at all,” 1 for “applied to me to some degree, or some of the time,” 2 for “applied to me to a considerable degree, or a good part of the time,” and 3 for “applied to me very much, or most of the time.” Scores for the DASS-21 sub-scales of depression, anxiety and stress were derived by totaling the scores for each sub-scale and multiplying by two. We classified women according to the recommended scoring system using cut-off values to classify participants into the following categories: normal (0–9 for depression and 0–7 for anxiety), mild (10–13 for depression and 8–9 for anxiety), moderate (14–20 for depression and 10–14 for anxiety), severe (21–27 for depression and 15–19 for anxiety), and extremely severe (≥28 for depression and ≥20 for anxiety). We have referred to women within the “normal” range on the DASS-21 for depressive or anxiety symptoms as nondepressed or nonanxious, respectively. Women, who scored in the “mild” to “extremely severe” ranges, were referred to as depressed or anxious. Analysis is based on this dichotomy (i.e., “normal range” vs. “mild to extremely severe” symptoms). A score of DASS ≥10 was used to distinguish women suffering from depression, a score of DASS ≥8 for anxiety disorders and a score of DASS ≥15 for stress.
Data collection took place from July 2012 to March 2014. The sample size was determined on previous reported prevalence rate [2,3,5] and sample size of 1468 subjects would be required for this study. Of the 22 PHC centers available, we selected 12 health centers on a random sampling basis, of these, 10 were located in urban and 2 in semi-urban areas of Qatar. Each participant was provided with brief information about the study and was assured of strict confidentiality. Finally, subjects were selected by systematically sampling design 1-in-2 sampling procedure used and a representative sample of 1468 women aged 45–65 years were approached and 1101 women agreed to participate (75.0%) and responded to the study. The survey instrument was initially tested for validation on 100 patients through face to face interview who visited the health centers. Internal consistency in this study was explored for each scale of the DASS-21, and Cronbach’s alpha coefficients were adequate: Depression (0.81), anxiety (0.75) and stress (83) scales respectively, confirming a high level of consistency among the different Likert items in this scale.
To assess total number of medical conditions, participants were asked: “Has a doctor ever told you that you have any of the following conditions or have you had any of the following procedures?” Participants could mark as many as applied.
Statistical test
Data were analyzed using SPSS version 21 (Chicago IL,USA) statistical software. Student’s t-test was used to ascertain the significance of differences between mean values of two continuous variables and confirmed by nonparametric Mann–Whitney test. The Chi-square and Fisher’s exact tests (two-tailed) were performed to test for differences in proportions of categorical variables between two or more groups. Multivariate regression analysis using the forward inclusion and backward deletion method was used to assess the relationship between dependent and independent variables and to adjust for potential confounders and orders the importance of risk factors (determinants) for menopausal depression, anxiety, and stress. All statistical tests were two-sided and P < 0.05 was considered statistically significant.
Results
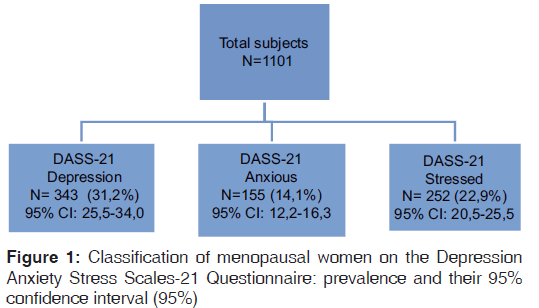
1101 women agreed to participate and were included in the study. The mean age and standard deviation of the menopausal and postmenopausal age were 49.55 (3.12) and 58.08 (3.26) (P < 0.001). Figure 1 shows the distribution and classification of menopausal women on the DASS-21 questionnaire: Prevalence and their 95% confidence interval (95%).
Table 1 shows the sociodemographic characteristics of studied subject by menopausal and postmenopausal status. There were statistically significant differences between menopausal stages with regards to age, ethnicity, educational status, occupation status, and place of living.
| Variable | Total (n=1101), n (%) | Menopause (n=521), n (%) | Postmenopausal (n=580), n (%) | P | |||
|---|---|---|---|---|---|---|---|
| Age | 54.17 (5.32) | 49.55 (3.12) | 58.08 (3.26) | <0.001 | |||
| Age of menarche | 12.61 (1.53) | 12.56 (1.55) | 12.66 (1.52) | 0.39 | |||
| Ethnicity | |||||||
| Qatari | 772 | (70.1) | 340 | (65.3) | 432 | (74.5) | 0.001 |
| Nonqatari | 329 | (29.9) | 181 | (34.7) | 148 | (25.5) | |
| Education level | |||||||
| Illiterate | 203 | (18.4) | 78 (15.0) | 125 | (21.6) | <0.01 | |
| Elementary | 221 | (20.1) | 104 | (20.0) | 117 | (20.2) | |
| Intermediate | 225 | (20.4) | 103 | (19.8) | 122 | (21.0) | |
| Secondary | 279 | (25.3) | 134 | (25.7) | 145 | (25.0) | |
| University | 173 | (15.7) | 102 | (19.6) | 71 (12.2) | ||
| Occupation | |||||||
| Housewife | 603 | (54.8) | 272 | (52.2) | 331 | (57.1) | <0.01 |
| Sedentary | 144 | (13.1) | 89 (17.1) | 55 | (9.5) | ||
| professional | |||||||
| Manual | 207 | (18.8) | 99 (19.0) | 108 | (18.6) | ||
| Businessman | 74 | (6.7) | 32 | (6.1) | 42 | (7.2) | |
| Arm/police | 73 | (6.6) | 29 | (5.6) | 44 | (7.6) | |
| Household Income | |||||||
| <$1500 US dollars | 83 | (7.5) | 39 | (7.5) | 44 | (7.6) | 0.09 |
| $1500-$3499 | 411 | (37.3) | 188 | (36.1) | 223 | (38.4) | |
| $3500-$5499 | 370 | (33.6) | 165 | (31.7) | 205 | (35.3) | |
| ≥$5500 | 237 | (21.5) | 129 | (24.8) | 108 | (18.6) | |
| Consanguinity | |||||||
| Yes | 332 | (30.2) | 159 | (30.5) | 173 | (29.8) | 0.80 |
| No | 769 | (69.8) | 362 | (69.5) | 407 | (70.2) | |
| Place of living | |||||||
| Urban | 920 | (83.6) | 422 | (81.0) | 498 | (85.9) | 0.03 |
| Semi-urban | 181 | (16.4) | 99 (19.0) | 82 (14.1) | |||
| House condition | |||||||
| Villa | 378 | (34.3) | 169 | (32.4) | 209 | (36.0) | 0.61 |
| Semi-villa | 546 | (49.6) | 263 | (50.5) | 283 | (48.8) | |
| Apartment-flat | 125 | (11.4) | 63 (12.1) | 62 (10.7) | |||
| Mud | 52 | (4.7) | 26 | (5.0) | 26 | (4.5) | |
Table 1: The sociodemographic of studied subject by menopause and postmenopausal according to depression (n=1101)
Table 2 shows the lifestyle characteristics of the participants by menopause and postmenopausal according to depression. There were statistically significant differences between menopausal stages with regards to body mass index, systolic and diastolic blood pressure (BP), Vitamin D deficiency, and diseases.
| Variable | Total (n=1101), n (%) | Menopause (n=521), n (%) | Postmenopausal (n=580), n (%) | P | |||
|---|---|---|---|---|---|---|---|
| BMI group (kg/m2) | |||||||
| <25 | 267 | (24.3) | 145 | (27.8) | 122 | (21.0) | 0.03 |
| 25-30 | 548 | (49.7) | 246 | (47.2) | 302 | (52.1) | |
| >30 | 286 | (26.0) | 130 | (25.0) | 156 | (26.9) | |
| Systolic BP | 130.27 (14.29) | 128.99 (12.92) | 131.41 (15.33) | <0.01 | |||
| Diastolic BP | 82.97 (8.35) | 82.24 (8.14) | 83.62 (8.48) | <0.01 | |||
| Regular exercise | |||||||
| Yes | 312 | (28.3) | 152 | (29.2) | 160 | (27.6) | 0.56 |
| No | 789 | (71.7) | 369 | (70.8) | 420 | (72.4) | |
| Physical activity | |||||||
| Yes | 295 | (26.8) | 143 | (27.4) | 152 | (26.2) | 0.64 |
| No | 806 | (73.2) | 378 | (72.6) | 428 | (73.8) | |
| Diseases | |||||||
| Without diseases | 765 | (69.5) | 392 | (75.2) | 373 | (64.3) | <0.001 |
| Diabetic | 122 | (11.1) | 51 | (9.8) | 72 (12.2) | ||
| Hypertension | 76 | (6.9) | 32 | (6.1) | 44 | (7.6) | |
| Asthma | 64 | (5.8) | 27 | (5.2) | 37 | (6.4) | |
| Arthritis | 24 | (2.2) | 12 | (2.3) | 12 | (2.1) | |
| Stroke | 22 | (2.0) | 4 (0.8) | 18 | (3.1) | ||
| CHD | 28 | (2.5) | 3 (0.6) | 25 | (4.3) | ||
| Cigarette smoking habit | |||||||
| Never | 1040 (94.5) | 494 | (94.8) | 546 | (94.1) | 0.68 | |
| Current smoker | 24 | (2.2) | 12 | (2.3) | 12 | (2.1) | |
| Past smoker | 37 | (3.4) | 15 | (2.9) | 22 | (3.8) | |
| Shisha smoking habit | |||||||
| Never | 106 (9.6) | 50 | (9.6) | 56 | (9.7) | 0.97 | |
| Current smoker | 995 | (90.4) | 471 | (90.4) | 524 | (90.3) | |
Table 2: The lifestyle characteristics of studied subjects by menopause and postmenopausal status (n=1101)
Table 3 reveals the association of depression, anxiety, and stress with sociodemographic characteristics in menopause and postmenopause women. Depression and anxiety were more common among postmenopause women. Furthermore, there were no differences between the groups regarding the frequency of certain levels of stress among menopause and postmenopause.
| Variable | Depression (yes) | Anxiety (yes) | Stress (yes) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DASS ≥14 (n=343) | DASS ≥10 (n=155) | DASS ≥19 (n=252) | ||||||||||||||
| Menopause | Postmenopausal | P | Menopause | Postmenopausal | P | Menopause | Postmenopausal | P | ||||||||
| (n=165) | (n=178) | (n=68) | (n=87) | (n=139) | (n=113) | |||||||||||
| Ethnicity | ||||||||||||||||
| Qatari | 108 (65.5) | 138 (77.5) | 0.013 | 41 | (60.3) | 69 | (79.3) | 0.010 | 91 | (65.5) | 84 | (74.3) | 0.13 | |||
| Nonqatari | 57 | (34.5) | 40 (22.5) | 27 | (39.7) | 18 | (20.7) | 48 | (34.5) | 29 | (25.7) | |||||
| Educationlevel | ||||||||||||||||
| Illiterate | 26 | (15.8) | 30 (16.9) | 0.260 | 10 | (14.7) | 14 | (16.1) | 0.355 | 21 | (15.1) | 25 | (22.1) | 0.46 | ||
| Elementary | 30 | (18.2) | 42 (23.6) | 15 | (22.1) | 16 | (18.4) | 25 | (18.0) | 22 | (19.5) | |||||
| Intermediate | 39 | (23.6) | 29 (16.3) | 10 | (14.7) | 18 | (20.7) | 28 | (20.1) | 20 | (17.7) | |||||
| Secondary | 41 | (24.8) | 53 (29.8) | 16 | (23.5) | 27 | (31.0) | 46 | (33.1) | 28 | (24.8) | |||||
| University | 29 | (17.6) | 24 (13.5) | 17 | (25.0) | 12 | (13.8) | 19 | (13.7) | 18 | (15.9) | |||||
| Occupation | ||||||||||||||||
| Housewife | 82 | (49.7) | 107 (60.1) | 0.122 | 27 | (39.7) | 50 | (57.5) | 0.175 | 73 | (52.5) | 71 | (62.8) | 0.39 | ||
| Sedentary | 30 | (18.2) | 16 (9.0) | 17 | (25.0) | 11 | (12.6) | 25 | (18.0) | 14 | (12.4) | |||||
| professional | ||||||||||||||||
| Manual | 34 | (20.6) | 34 (19.1) | 12 | (17.6) | 15 | (17.2) | 30 | (21.6) | 19 | (16.8) | |||||
| Businessman | 9 | (5.5) | 11 (6.2) | 6 | (8.8) | 5 | (5.7) | 6 ( 4.3) | 3 | (2.7) | ||||||
| Arm/police | 10 (6.1) | 10 (5.6) | 6 | (8.8) | 6 | (6.9) | 5 | (3.6) | 6 | (5.3) | ||||||
| Householdincome | ||||||||||||||||
| <$1500 US | 12 (7.3) | 14 (7.9) | 0.633 | 6 | (8.8) | 6 | (6.9) | 0.779 | 11 (7.9) | 8 | (7.1) | 0.56 | ||||
| dollars | ||||||||||||||||
Table 3: Association of depression, anxiety and stress with stressful life events in menopause and postmenopausal women
| Variable | Depression (yes) | Anxiety (yes) | Stress (yes) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| DASS ≥14 (n=343) | DASS ≥10 (n=155) | DASS ≥19 (n=252) | |||||||||
| Menopause | Postmenopausal | P | Menopause | Postmenopausal | P | Menopause | Postmenopausal | P | |||
| (n=165) | (n=178) | (n=68) | (n=87) | (n=139) | (n=113) | ||||||
| $1500-$3499 | 59 (35.8) | 74 (41.6) | 23 (33.8) | 24 (27.6) | 46 (33.1) | 45 (39.8) | |||||
| $3500-$5499 | 56 (33.9) | 57 (32.0) | 27 (39.7) | 39 (44.8) | 50 (36.0) | 41 (36.3) | |||||
| ≥$5500 | 38 (23.0) | 33 (18.5) | 12 (17.6) | 18 (20.7) | 32 (23.0) | 19 (16.8) | |||||
| Consanguinity | |||||||||||
| Yes | 41 (24.8) | 52 (29.2) | 0.364 | 25 (36.8) | 24 (27.6) | 0.223 | 43 (30.9) | 31 (27.4) | 0.54 | ||
| No | 124 (75.2) | 126 (70.8) | 43 (63.2) | 63 (72.4) | 96 (69.1) | 82 (72.6) | |||||
| Place of living | |||||||||||
| Urban | 136 (82.4) | 146 (82.0) | 0.923 | 54 (79.4) | 73 (83.9) | 0.609 | 115 (82.7) | 93 (82.3) | 0.93 | ||
| Semiurban | 29 (17.6) | 32 (18.0) | 14 (20.6) | 14 (16.1) | 24 (17.3) | 20 (17.7) | |||||
Table 3: Contd...
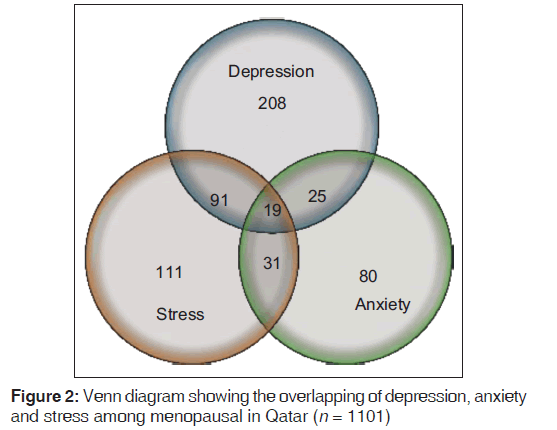
Table 4 presents the lifestyle characteristics of the participants by menopause and postmenopausal according to depression, anxiety, and stress. There were no any significant differences between menopause and postmenopause stage. Figure 2 presents Venn diagram showing the overlapping of depression, anxiety and stress among menopausal in Qatar.
| Variable | Depression (yes) | Anxiety (yes) | Stress (yes) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DASS ≥14 (n=343) | DASS ≥10 (n=155) | DASS ≥19 (n=252) | ||||||||||||||||
| Menopause Postmenopausal | P | Menopause Postmenopausal | P | Menopause Postmenopausal | P | |||||||||||||
| (n=165) | (n=178) | (n=68) | (n=87) | (n=139) | (n=113) | |||||||||||||
| Age | 50.1 (3.09) | 57.7 (3.21) | <0.001 | 49.5 (3.10) | 57.3 (3.36) | <0.001 | 50.20 (3.08) | 57.10 (3.70) | 0.001 | |||||||||
| Age of menarche | 12.67 (1.58) | 12.49 (1.53) | 0.265 | 12.59 (1.43) | 12.72 (1.57) | 12.65 (1.53) | 12.63 (1.51) | 0.80 | ||||||||||
| BMI (kg/m2) | 0.687 | |||||||||||||||||
| <25 | 46 | (27.9) | 44 | (24.7) | 0.796 | 23 | (33.8) | 15 | (17.2) | 40 | (28.8) | 27 | (23.9) | 0.54 | ||||
| 25-30 | 79 | (47.9) | 88 | (49.4) | 31 | (45.6) | 48 | (55.2) | 0.057 | 67 | (48.2) | 54 | (47.8) | |||||
| >30 | 40 | (24.2) | 46 | (25.8) | 14 | (20.6) | 24 | (27.6) | 32 | (23.0) | 32 | (28.3) | ||||||
| Systolic BP | 129.17 (12.84) | 130.10 (15.06) | 0.588 | 128.76 (10.47) | 130.08 (14.80) | 129.76 (13.27) | 132.50 (15.10) | 0.18 | ||||||||||
| Diastolic BP | 81.66 (7.93) | 83.49 (8.13) | 0.025 | 80.91 (6.81) | 83.46 (8.40) | 0.658 | 82.64 (8.32) | 85.15 (8.56) | 0.01 | |||||||||
| Regular exercise | 0.037 | |||||||||||||||||
| Yes | 54 | (32.7) | 43 | (24.2) | 0.078 | 18 | (26.5) | 21 | (24.1) | 48 | (34.5) | 25 | (22.1) | 0.03 | ||||
| No | 111 | (67.3) | 135 | (75.8) | 50 | (73.5) | 66 | (75.9) | 0.740 | 91 | (65.5) | 88 | (77.9) | |||||
| Diseases | ||||||||||||||||||
| Without diseases | 124 | (75.2) | 124 | (69.7) | 0.173 | 50 | (73.5) | 54 | (62.1) | 106 (76.3) | 73 | (64.6) | 0.09 | |||||
| Diabetic | 15 | (9.1) | 17 | (9.6) | 8 (11.8) | 13 | (14.9) | 0.559 | 13 (9.4) | 12 | (10.6) | |||||||
| Hypertension | 12 | (7.3) | 11 | (6.2) | 4 | (5.9) | 4 | (4.6) | 10 (7.2) | 7 | (6.2) | |||||||
| Asthma | 10 | (6.1) | 11 | (6.2) | 2 | (2.9) | 7 | (8.0) | 7 | (5.0) | 14 | (12.4) | ||||||
| Arthritis | 2 | (1.2) | 2 | (1.1) | 2 | (2.9) | 3 | (3.4) | 2 | (1.4) | 2 | (1.8) | ||||||
| Stroke | 1 | (0.6) | 4 | (2.2) | 2 | (2.9) | 5 | (5.7) | 1 | (0.7) | 2 | (1.8) | ||||||
| CHD | 1 | (0.6) | 9 | (5.1) | 0 | (0.0) | 1 | (1.1) | 0 | (0.0) | 3 | (2.7) | ||||||
| Cigarette smoking | ||||||||||||||||||
| Never | 156 | (94.5) | 170 | (95.5) | 0.696 | 66 | (97.1) | 83 | (95.4) | 133 (95.7) | 109 (96.5) | 0.91 | ||||||
| Current smoker | 5 | (3.0) | 3 | (1.7) | 0 | (0.0) | 1 | (1.1) | 0.550 | 2 | (1.4) | 1 | (0.9) | |||||
| Past smoker | 4 | (2.4) | 5 | (2.8) | 2 | (2.9) | 3 | (3.4) | 4 | (2.9) | 3 | (2.7) | ||||||
| Shisha smoking habit | ||||||||||||||||||
| Never | 23 | (13.9) | 18 | (10.1) | 0.275 | 8 (11.8) | 6 | (6.9) | 22 | (15.8) | 11 (9.7) | 0.21 | ||||||
| Current smoker | 142 | (86.1) | 160 | (89.9) | 60 | (88.2) | 81 | (93.1) | 0.443 | 117 (84.2) | 102 (90.3) | |||||||
Table 4: The lifestyle characteristics of studied subjects by menopause and postmenopausal status according to depression. anxiety, and stress
Table 5 gives multivariate regression analyses for depression, anxiety, and stress and associated covariates. As can be seen from this table that age in years, diastolic BP, consanguinity, regular exercise were predictor for depression. Meanwhile, diastolic BP, occupation, and physical activity considered the main risk factors for anxiety. Furthermore, age in years, occupation and sheesha smoking habits were considered as the main risk factors associated with stress.
| Regression | SE | t | P | |
|---|---|---|---|---|
| Depression | ||||
| Age in years | 0.371 | 0.137 | 2.708 | <0.01 |
| Diastolic BP | −0.579 | 0.218 | −2.643 | 0.01 |
| Consanguinity | 0.748 | 0.366 | 2.043 | 0.04 |
| Regular exercise | 0.046 | 0.021 | 2.238 | 0.03 |
| Anxiety | ||||
| Diastolic BP | −0.030 | 0.011 | −2.653 | <0.001 |
| Occupation | 0.177 | 0.073 | 2.417 | 0.02 |
| Physical activity | 0.423 | 0.209 | 2.018 | 0.04 |
| Stress | ||||
| Age in years | −0.006 | 0.002 | −2.532 | 0.01 |
| Occupation | −0.020 | 0.010 | −2.052 | 0.04 |
| Sheesha smoking | −0.086 | 0.043 | −2.003 | 0.04 |
Table 5: Correlates of menopause with depression, anxiety, and stress using multivariate regression analysis in (n=1101)
Discussion
Menopause produces very complex changes during this stage of life which include other changes such as psychological and social changes.[2,3] A recent study from Finland[1] and the United States[17] showed that due to postmenopause depression predicted increased bone loss. In Finland self-reported,[1] sleep problems observed more common in postmenopausal women than in premenopausal women, and the difference is more pronounced during workdays than during leisure days. These observations suggest that postmenopausal women have the capacity for a good sleep but are more vulnerable to sleep problems related to work-related stress. The negative impact of depressive symptoms on postmenopausal women was observed to be independent of body weight or other behavioral factors such as calcium compliance or exercise.[17] Unfortunately, the current study showed that only over one-third of women involved in physical exercise or regular activity.
More recently, study in Vietnam the results highlighted the importance of considering psychosocial factors, life style, and chronic disease management in providing health guidance for peri- and post-menopausal women to enhance their quality of life and reduce the risk of depressive symptoms.[1,20-22] This is consistent with this study outcome.
In contrast, there are protective factors that reduce the risk of depression. Interpersonal protective factors include adequate social support, which may protect against the onset of depression or may result in a more benign course of depression.[16,23] Another potential protective factor is physical activity. Individuals who engage in regular physical activity have less depression over time.[24] Preliminary evidence from randomized controlled trials suggests that regular aerobic exercise may be an effective intervention for adults with mild-moderate depression,[25] and that aerobic exercise may be as effective as sertraline or cognitive-behavioral therapy. Physical activity may also serve as a buffer for the effect of stress on depression.[16] Although it is well-established that certain stressors and protective factors are associated with changes in depression symptoms over time, less is known about effect moderation.
Most recently study in United States reported[16] that stressors at baseline, including verbal abuse, physical abuse, care giving, social strain, negative life events, financial stress, low income, acute pain, and a greater number of chronic medical conditions, were all associated with higher levels of depression symptoms at baseline and new onset elevated symptoms at 3 years follow-up among postmenopause women. In addition, social support and physical activity were associated with lower levels of depressive symptoms. Similarly, more social support at baseline increased the association between financial stress, income, and pain on new-onset depression 3 years later. Physical activity similarly moderated the effect of care giving, income, and pain on depression symptoms at baseline. Present results are consistent with other previous reported studies. [13 ,21-27]
McEwen and Sapolsky[26] have suggested that engagement in a more socially and emotionally supportive environment results in lower levels of physiologic arousal; this in turn protects against cognitive decline and depression secondary to direct positive stimulatory effects on the brain. Fortunately,the social environment is modifiable. For example, one can directly increase social support through participation in support groups or other organizations that promote social bonds such as religious or civic groups. Alternatively, behavioral health specialists can also indirectly help to increase an older individual’s social support through teaching of skills directed at gaining needed support.[27] Similarly, physical activity was associated with lower depression levels, both concurrently and prospectively, and therefore may still be useful in decreasing the likelihood of depression as women age. The present research highlighted the importance of considering psychosocial factors, life style, and chronic disease management in providing health guidance for peri-menopausal women and postmenopausal women to enhance their quality of life and reduce the risk of depressive and stress symptoms, this consistent with the previous reported studies. [6-9,13,28] Furthermore, the current data suggest that there is a strong association between depression, anxiety and stress symptoms high rates in menopause and postmenopausal women: These findings are confirmative with some previous reported studies. [6-9,13,21-28]
Limitations and strengths
One of the strengths of this study was the large sample size; this is particularly important in order to have sufficient power to examine interaction effects. This study based on a large representative’s sample. There are several limitations of this study. First, this is cross sectional study and thereby, subjects might be misclassified in this analysis. Second, the study sample was based on PHC clinics visits. Third, the majority of the study sample was Arab women and of relatively high socioeconomic and education status; hence, the results may not be generalizable to the population of all midlife women. This cohort is also diverse in terms of geographic region of the country and race/ethnicity. Results must also be interpreted in the context of study limitations.
Conclusion
A large number of factors were associated with experiencing menopausal and psycho-social problems and which had negative effects on the quality of life among Arabian women. Depression, anxiety and stress should be considered as an important risk factors for osteoporosis.
Acknowledgements
The authors would like to thank the Hamad Medical Corporation for their support and ethical approval (HMC RC#8222/08).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Lampio L, Polo-Kantola P, Polo O, Kauko T, Aittokallio J, Saaresranta T. Sleep in midlife women: Effects of menopause, vasomotor symptoms, and depressive symptoms. Menopause 2014;21:1217-24.
- Gerber LM, Bener A, Al-Ali HM, Hammoudeh M, Liu LQ, Verjee M. Bone mineral density in midlife women: The Study of Women’s Health in Qatar. Climacteric 2015;18:316-22.
- Bener A, Falah A. A measurement-specific quality-of-life satisfaction during premenopause, perimenopause and postmenopause in Arabian Qatari women. J Midlife Health 2014;5:126-34.
- Oppermann K, Fuchs SC, Donato G, Bastos CA, Spritzer PM. Physical, psychological, and menopause-related symptoms and minor psychiatric disorders in a community-based sample of Brazilian premenopausal, perimenopausal, and postmenopausal women. Menopause 2012;19:355-60.
- Bener A, Rizk DE, Shaheen H, Micallef R, Osman N, Dunn EV. Measurement-specific quality-of-life satisfaction during the menopause in an Arabian Gulf country. Climacteric 2000;3:43-9.
- Spangler L, Scholes D, Brunner RL, Robbins J, Reed SD, Newton KM, et al. Depressive symptoms, bone loss, and fractures in postmenopausal women. J Gen Intern Med 2008;23:567-74.
- Cizza G, Primma S, Coyle M, Gourgiotis L, Csako G. Depression and osteoporosis: A research synthesis with meta-analysis. Horm Metab Res 2010;42:467-82.
- Erez HB, Weller A, Vaisman N, Kreitler S. The relationship of depression, anxiety and stress with low bone mineral density in post-menopausal women. Arch Osteoporos 2012;7:247-55.
- Bistrovic IL, Roncevic-Grzeta I, Crncevic-Orlic Z, Franciskovic T, Ljubicic R, Orlic A, et al. Connection of depression and bone loss in perimenopausal and postmenopausal women. Coll Antropol 2012;36:1219-23.
- Bener A, Yousafzai MT. Comparison of reliability and validity of the postpartum Depression Anxiety Stress Scales (DASS-21) with the Beck Depression Inventory (BDI-II) and Edinburgh Postpartum Depression Scale (EPDS) in Arabian women. Int J Appl Sci Comput 2012;19:141-56.
- Bener A, Gerber LM, Sheikh J. Prevalence of psychiatric disorders and associated risk factors in women during their postpartum period: A major public health problem and global comparison. Int J Womens Health 2012;4:191-200.
- Bosworth HB, Bastian LA, Kuchibhatla MN, Steffens DC, McBride CM, Skinner CS, et al. Depressive symptoms, menopausal status, and climacteric symptoms in women at midlife. Psychosom Med 2001;63:603-8.
- Bener A, Saleh NM. Low Vitamin D, and bone mineral density with depressive symptoms burden in menopausal and postmenopausal women. J Midlife Health 2015;6:108-14.
- Wu Q, Magnus JH, Liu J, Bencaz AF, Hentz JG. Depression and low bone mineral density: A meta-analysis of epidemiologic studies. Osteoporos Int 2009;20:1309-20.
- Wassertheil-Smoller S, Shumaker S, Ockene J, Talavera GA, Greenland P, Cochrane B, et al. Depression and cardiovascular sequelae in postmenopausal women. The Women’s Health
- Uebelacker LA, Eaton CB, Weisberg R, Sands M, Williams C, Calhoun D, et al. Social support and physical activity as moderators of life stress in predicting baseline depression and change in depression over time in the Women’s Health Initiative. Soc Psychiatry Psychiatr Epidemiol 2013;48:1971-82.
- Milliken LA, Wilhelmy J, Martin CJ, Finkenthal N, Cussler E, Metcalfe L, et al. Depressive symptoms and changes in body weight exert independent and site-specific effects on bone in postmenopausal women exercising for 1 year. J Gerontol A Biol Sci Med Sci 2006;61:488-94.
- Crawford JR, Henry JD. The Depression Anxiety Stress Scales (DASS): Normative data and latent structure in a large non-clinical sample. Br J Clin Psychol 2003;42(Pt 2):111-31.
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney: Psychology Foundation; 1995.
- Bener A, Burgut FT, Ghuloum S, Sheikh J. A study of postpartum depression in a fast developing country: Prevalence and related factors. Int J Psychiatry Med 2012;43:325-37.
- Aguilar-Zavala H, Pérez-Luque EL, Luna-Martínez F, Bassol-Mayagoitia S, Canto-de-Cetina T, López-Conesa M, et al. Symptoms at postmenopause: Genetic and psychosocial factors. Menopause 2012;19:1140-5.
- Wang HL, Booth-LaForce C, Tang SM, Wu WR, Chen CH. Depressive symptoms in Taiwanese women during the peri- and post-menopause years: Associations with demographic, health, and psychosocial characteristics. Maturitas 2013;75:355-60.
- Gilchrist G, Gunn J. Observational studies of depression in primary care: What do we know? BMC Fam Pract 2007;8:28.
- Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO.Exercise treatment for depression: Efficacy and dose response. Am J Prev Med 2005;28:1-8.
- Blumenthal JA, Babyak MA, Moore KA, Craighead WE, Herman S, Khatri P, et al. Effects of exercise training on older patients with major depression. Arch Intern Med 1999;159:2349-56.
- McEwen BS, Sapolsky RM. Stress and cognitive function. Curr Opin Neurobiol 1995;5:205-16.
- Reblin M, Uchino BN. Social and emotional support and its implication for health. Curr Opin Psychiatry 2008;21:201-5.
- Low CA, Matthews KA, Kuller LH, Edmundowicz D. Psychosocial predictors of coronary artery calcification progression in postmenopausal women. Psychosom Med 2011;73:789-94.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.