Diagnosis of Atypical Teratoid/Rhabdoid Tumour-Sine Qua Non in Treatment Process: A Case Report
2 Department of Pediatrics, Kasturba Medical College, Mangalore, India
Received: 20-Jul-2021 Accepted Date: Aug 10, 2021 ; Published: 24-Sep-2021
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Childhood Atypical Teratoid/Rhabdoid Tumour (AT/RT) of CNS is a rare and new clinical event. We report a rare case of this case to highlight the rarity and importance of successful treatment, using AT/RT protocol, although prognosis is dismal among children younger than 3 years. 2½ years old male child on MRI reveals heterogeneously enhancing lobulated mass on left side of the cerebellum with marked fourth ventricle compression leading to proximal hydrocephalus. The excised tumour on histopathology and tumour marker analysis shows the presence of AT/RT Grade IV of cerebellum with no metastasis. Treatment strategy was chemotherapy and cranial radiation and upon follow-up at the age of 5 years the child was asymptomatic on brain MRI.
Keywords
Atypical teratoid/rhabdoid tumour; Children; Magnetic resonance imaging; Cranial radiation
Background
Atypical Rhabdoid/Teratoid Tumour (AT/RT) is a clinical event related to Central Nervous System (CNS) with a specific cytogenetic profile observed in early childhood. AT/RT is reported as a histological variant of Wilm’s tumour which is highly visualized in infants with very poor prognosis. CNS tumour encompassing rhabdoid cells is first highlighted in 1985, however, its clinic-pathological characteristics are less reported till 1996. [1]
ATRT is highly prevalent in children below years and also seen in children above 10 years and adults. [2] The severity of the disease is seen 20-30 % of the cases Severe forms occur in 20% to 30% of cases. Children affected with ATRT has a stressfull disease course and average period of mortality after diagnosis is only 1-2 months [3,4].
The radiological findings of AT/RT are non specific in most of the cases. [3] However, it share the radiological findings similar to other tumors such as medulloblastoma and choroid plexus papillomas. [5]
The ATRT histological features shows presence of rhabdoid cells sheets with highly evident eosinophilic cytoplasm, eccentric large, and a highly visible nucleolus with presence or absence of fibrillary globoid inclusions. Further, cytomorphological features are very specific which gives the accurate diagnosis during radiological evaluation.[6]
ATRT is a rampant disease and the recovery is observed only in the minor cases and no specific treatment protocol is available. Meanwhile, the treatment modalities such as radiation and chemotherapy, surgery orchestrate a vital role in ATRT management. [6] We report a ATRT case, to showcase the rarity and importance of effective treatment with the help of AT/RT protocol, albeit the prognosis is highly severe in children less than 3 years.
Case Report
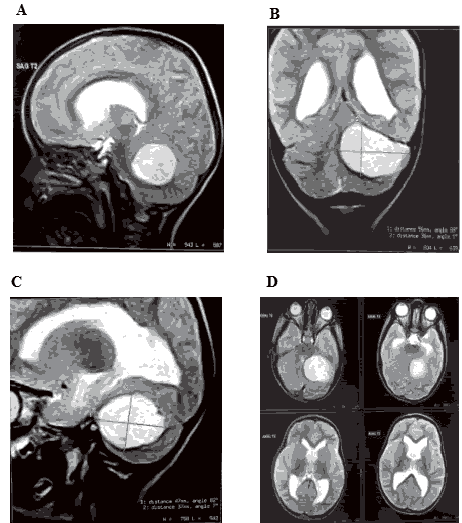
A previously normal 2½ years old male child presented to our pediatrics outpatient department with a 10 days history of headache and 3 days history vomiting. Physical examination showed only proximally enlarged head. Child was asymptomatic and there were no neurological and systemic complaints. There was no history of fever, altered sensorium, seizure, bleeding, and failure to gain weight or weight loss. Computerized Tomography (CT scan) showed intracranial space occupying lesions. Magnetic Resonance Imaging (MRI) of the brain revealed heterogeneously enhancing lobulated mass in left of cerebellum (5 × 4.4 × 3.6 cm), causing significant compression of fourth ventricle resulting in proximal hydrocephalus. The lesion was broad based to the duramater, but there was a partial rim of normal cerebellar tissue suggested intra-axial location (Figure 1A-1D).
Figure 1A and 1D Perioperative MRI brain revealed heterogeneously enhancing lobulated mass in left of cerebellum (5 x 4.4 x 3.6 cm), causing significant compression of fourth ventricle resulting in proximal hydrocephalus. The lesion was broad based to the duramater, but there was a partial rim of normal cerebellar tissue suggested intra-axial location
Posterior craniotomy and excision of tumour was done. Histopathological examination and tumour markers were done in the same centre and were also confirmed by NIMHANS, Bangalore and TATA Memorial Hospital, Mumbai. The report revealed sheets of small undifferentiated cells that exhibit brisk mitotic activity, minimal stroma and papillary arrangement with rhabdoid morphology.
The report also revealed premalignant tumour which has failed to mark with astrocytic markers (GFAP- repeated twice), neuronal marker (synaptophysin, S-100 and chromogranin) and epithelial markers (CK and EMA). Mib-1 was positive in 50%, Mic-2 was positive. INI1 was negative.
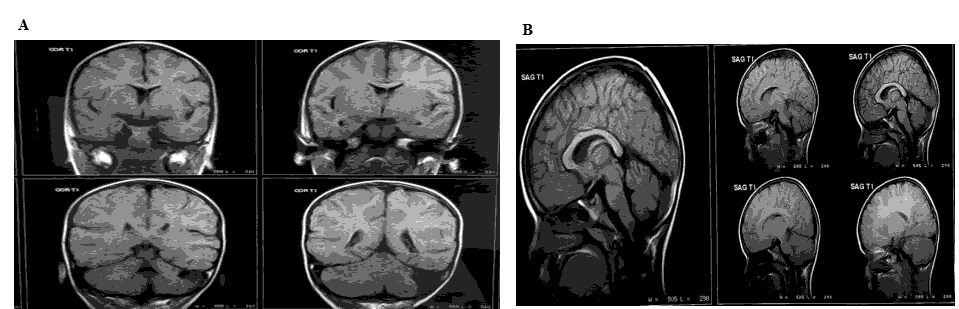
The report confirmed the diagnosis of AT/RT cerebellum (WHO Grading-IV). Metastatic workup was done and was negative. After surgery, child was on chemotherapy as per AT/RT protocol. After initial chemotherapy, cranial radiation was given. Today at the age of 6 years, child is undergoing follow-up. Child is asymptomatic. MRI brain was performed and it was normal (Figure 2A and 2B).
Figure 2A and 2B Posterior craniotomy was done for the tumour excision. Post operatively chemotherapy and cranial radiation was advised. After 6 years of follow up the children is asymptomatic and MRI was normal.
Discussion
AT/RT of cerebellum is a rare clinical event and majorly diagnosed in early childhood. It occupies 2-3 % of all childhood tumors below 18 years and male children are highly affected with the condition [7] The incidence is observed in children less than 3 years of age in majority of the cases. The tumor is affected at posterior fossa of cerebellum in about 2/3 of all reported cases. [7] Recently, mutations in the chromatic remodeling complex SMARCB1 (and, as a rare alternative, of SMARCA4) have been observed in large cases of Atypical Rhabdoid/Teratoid Tumour AT/RT. [8]
This is a case-report of Atypical Rhabdoid/Teratoid Tumour AT/RT which occurred in a 3 year old male child in the cerebellar region. Atypical Rhabdoid/Teratoid Tumour AT/RT tumour is a devastating disease with high malignant rate and thus complete excision of tumor is not possible. Meanwhile, children in this age group are prone to dissemination during diagnosis and displays higher rate of disease progression.[4] The hallmark feature of this diseases is the children are neurologically normal during diagnosis and at the time of presentation. The cardinal reason for performing MRI in Atypical Rhabdoid/Teratoid Tumour AT/RT is due to the visualization of proximally enlarged head. The radiological analysis reveals the presence of intracranial space on the cerebellum left portion with marked lesions and compression of fourth ventricle leading to hydrocephalus in proximal portion. There are marked variation in the appearance of Atypical Rhabdoid/Teratoid Tumour AT/RT histology studies, but the cardinal feature is the presence of rhabdoid cells. [9] Our patient’s tumour showed sheets of small undifferentiated cells with brisk mitotic activity, minimal stroma and papillary arrangement with rhabdoid morphology. Immunohistochemistry revealed premalignant tumour with negative astrocytic markers (GFAP- repeated twice), neuronal marker (synaptophysin, S-100 and chromogranin) and epithelial markers (CK and EMA). Mib-1 was positive in 50%, Mic-2 was positive. INI1 was negative.
The optimal treatment for ATRT remains unclear. Till date, surgical resection is the major treatment protocol for ATRT. In a study done by Lafay-Cousin et al. out of 50 children with less than 18 years with CNS ATRT, 15 patients are subjected to gross total resection and about 60% of the patients had 2 year overall survival as compared to 10 patients subjected to subtotal resection, only 21% of the patients displayed a 2 year overall survival (=0.03).[10] The radiation therapy along with the surgical resection has a significant impact in the prevention of Atypical Rhabdoid/ Teratoid Tumour AT/RT progression. In a retrospective study conducted by Buscariollo et al. displayed that 144 Atypical Rhabdoid/Teratoid Tumour AT/RT patients who underwent radiation therapy showed significant (p<0.001) overall survival upto 34 months as compared to patients who did not underwent radiation therapy has a survival rate of 6 months. [11] However, the main disadvantage of radiation therapy is that the young children may develop neurocognitive deficits. Previous studies shows that, patients subjected to radiation therapy at young age for the treatment of Atypical Rhabdoid/ Teratoid Tumour AT/RT, displayed chronic neurological, cognitive disorders with a marked reduction in intelligence quotient.[12]
Chemotherapy has been well documented for the treatment of Atypical Rhabdoid/Teratoid Tumour AT/RT. Most of the patients receive chemotherapy to postpone radiation therapy particularly in children less than 3 years age. The Canadian pediatric brain tumor consortium [10] published that 18 patients who underwent high dose chemotherapy displayed 2 year overall survival (47.9%) as compared to the patients (27.3%) who have received conventional chemotherapy reported on 18 patients who received High-Dose Chemotherapy (HDC) regimens and noted longer 2-year overall survival compared to those who received conventional chemotherapy (P=0.036). In our patient, the treatment modality is chemotherapy and cranial radiation and upon follow-up at the age of 5 years the child is asymptomatic on brain MRI.
Conclusion
We present the clinic-radiological features of atypical teratoid/rabdoid tumor in an infant. There is an urgent need to relook at the strategy of diagnosis and treatment of this tumor. In this case the tumor presented as an aggressive cerebellar hemispheric mass with significant compression of the fourth ventricle. Although the characteristics seen on CT or MR imaging was very similar to medulloblastoma and ependymoma, the cerebellar hemispheric location and the aggressive growth pattern could be considered as a gross morphologic characteristics of this tumor.
Acknowledgment
Nil
Conflict of Interest
None to declare.
Funding Sources
Nil
REFERENCES
- Chan KH, Mohammed Haspani MS, Tan YC, Kassim F. A case report of atypical teratoid/rhabdoid tumour in a 9-year-old girl. Malays J Med Sci MJMS 2011;18(3):82–66.
- Bouvier C, De Paula AM, Fernandez C, Quilichini B, Scavarda D, Gentet JC, et al. Atypical teratoid/rhabdoid tumour: 7-year event-free survival with gross total resection and radiotherapy in a 7-year-old boy. Childs nervsystchns off. J Int Soc Pediatr Neuro Surg. 2008 ;24(1):143–147.
- Lee IH, Yoo S-Y, Kim JH, Eo H, Kim OH, Kim I-O, et al. Atypical teratoid/rhabdoid tumors of the central nervous system: imaging and clinical findings in 16 children. Clin Radiol. 2009 ;64(3):256–264.
- Hilden JM, Meerbaum S, Burger P, Finlay J, Janss A, Scheithauer BW, et al. Central nervous system atypical teratoid/rhabdoid tumor: results of therapy in children enrolled in a registry. J Clin Oncol Off J Am Soc Clin Oncol. 2004 ;22(14):2877–2884.
- Parwani AV, Stelow EB, Pambuccian SE, Burger PC, Ali SZ. Atypical teratoid/rhabdoid tumor of the brain: Cytopathologic characteristics and differential diagnosis. Cancer. 2005 ;105(2):65–70.
- Tekautz TM, Fuller CE, Blaney S, Fouladi M, Broniscer A, Merchant TE, et al. Atypical Teratoid/Rhabdoid Tumors (ATRT): Improved survival in children 3 years of age and older with radiation therapy and high-dose alkylator-based chemotherapy. J Clin Oncol Off J Am Soc Clin Oncol. 2005 ;23(7):1491–9.
- Lee YK, Choi CG, Lee JH. Atypical teratoid/rhabdoid tumor of the cerebellum: report of two infantile cases. AJNR Am J Neuroradiol. 2004 ;25(3):481–483.
- Hasselblatt M, Isken S, Linge A, Eikmeier K, Jeibmann A, Oyen F, et al. High-resolution genomic analysis suggests the absence of recurrent genomic alterations other than SMARCB1 aberrations in atypical teratoid/rhabdoid tumors. Genes Chromosomes Cancer. 2013;52(2):185-190.
- Rorke LB, Packer RJ, Biegel JA. Central nervous system atypical teratoid/rhabdoid tumors of infancy and childhood: definition of an entity. J Neurosurg. 1996 ;85(1):56–65.
- Lafay-Cousin L, Hawkins C, Carret AS, Johnston D, Zelcer S, Wilson B, et al. Central nervous system atypical teratoidrhabdoid tumours: The Canadian Paediatric Brain Tumour Consortium experience. Eur J Cancer. 2012; 48:353–359
- Buscariollo DL, Park HS, Roberts KB, Yu JB. Survival outcomes in atypical teratoid/rhabdoid tumor for patients undergoing radiotherapy in a Surveillance, Epidemiology, and end results analysis. Cancer. 2012; 118(17):4212-4219.
- Squire SE, Chan MD, Marcus KJ. Atypical teratoid/rhabdoid tumor: the controversy behind radiation therapy. J Neurooncol. 2007;81:97–111.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.