Diagnostic Accuracy of different Methods of Palpation and Percussion of Spleen for Detection of Splenomegaly in Children
Published: 27-Aug-2021
Citation: Taksande A, Saqqaf SA, Damke S, Meshram R. Diagnostic Accuracy of Different Methods of Palpation and Percussion of Spleen for Detection of Splenomegaly in Children. Ann Med Health Sci Res. 2021;11:89-93
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Standard medical physical examination plays a major role in the decision-making regarding the diagnosis, investigations, and treatment of any illness or the teaching and examination of doctors-in-training. Unfortunately, standard medical examination still has yet to be thoroughly studied upon. The skill and ability to percuss and palpate the spleen to successfully detect and analyze the splenomegaly is a difficult task in infants and adolescents. Objective: Here in this study we would like to know the accuracy and reliability of clinical examination (by using three different methods of percussion and palpation) for detecting splenomegaly in children. Methodology: In this cross-sectional study, the eligible children will be examined by the three paediatric residents for splenomegaly by different methods. For palpation, supine palpation maneuver, Middleton’s hooking maneuver, and right lateral decubitus methods will be used whereas for percussion, traube's space percussion, castell's maneuver and Nixon’s maneuver will be used. Each patient will be subject to three methods of percussion and palpation each. After that, we will do the ultrasonography of the patient for detection of the splenomegaly. Results: After the completion of the study, we will come to know the accuracy and reliability of the clinical examination (palpation and percussion) of the spleen for the detection of splenomegaly. Conclusion: We will come to know the diagnostic accuracy of the different methods of palpation and percussion for detecting splenomegaly.
Keywords
Splenomegaly, Palpation, Percussion, Ultrasonography
Introduction
Clinical examination plays a significant part in the evaluation of patients and determining their plan of management, diagnosis, and prognosis.
Involves various signs of reproducibility and accuracy. There are still substantial inroads to be made on standard physical examination by evidence-based medicine.
To clinically diagnose and detect splenomegaly requires good skills and is very important in the course of an illness. The accuracy of clinical examination (palpation and percussion) for detecting splenomegaly has not been studied previously.
Standard techniques used by the bedside include palpation and percussion to document the spleen size. But it is very difficult to detect tiny changes in the spleen size. [1-4]
The spleen size varies widely according to age, which is further altered by the aetiology of the illness like infection, malignant conditions, etc. The best method to examine the spleen is with the patient in the supine position and palpating the abdomen from the right iliac fossa across to towards the left costal margin in the left hypochondriac quadrant when the patient is deeply inspiring.
A spleen increased in size might descend into the pelvis when the spleen is enlarged. Palpation for splenomegaly is only moderately sensitive but highly specific. Ultrasonography is a safe, quick, established, non-invasive and accurate method of spleen size measurement. Other methods of radiologic confirmation of splenic enlargement are CT or technetium-99 sulphur colloid scan. [4-9] Here in this study, we want to know the accuracy and reliability of clinical examination (by using three different methods of percussion and palpation) for detecting splenomegaly in children, since all the published data so far is mainly related to adolescents and adults.
Aim &Objectives
Aim
To know how accurate is the clinical examination (by using three different methods of palpation and percussion) for detecting splenomegaly as compared to ultrasonic graphically confirmed splenomegaly.
Objective
To determine reliability of the clinical examination for detecting splenomegaly across three paediatric residents.
Material&Methods
Study design: The design of the study will be a prospective, cross-sectional study. We plan to determine diagnostic accuracy of the index test {Clinical assessment of splenomegaly (percussion and palpation)} as compared to a reference standard (splenomegaly confirmed by ultrasonography) in an independent manner, over a 12 month period.
Setting: The Department of the Paediatrics, JNMC, DMIMS, Sawangi Meghe, Wardha.
Participants: Patients aged 2 months to 15 years admitted in Paediatric wards due to infectious, renal, hepatic and cardiac problems.
Selection Criteria
Inclusion criteria
Children, ages 2 months to 15 years who will be admitted to Paediatric wards due to infectious, renal, hepatic and cardiac problems.
Exclusion criteria
• Known cases of splenomegaly
• Left-sided pleural effusion
• Previous history of ascites
• If the child is receiving a blood transfusion at the time of enrolment
• Whose parent(s) do-not agree for inclusion in the study
Interventions
Three methods of Palpation (Supine Palpation Maneuver, Middleton's Hooking Maneuver, Right lateral decubitus and supine) and three methods of Percussion (Traube’s space percussion, Nixon's Maneuver, Castell's Maneuver) will be performed on each patient by three different paediatrics residents. A well-informed written consent will be taken from either of the child’s parent for inclusion in the study. They will be explained that investigation for splenomegaly will be done at no additional charge.
Study Procedures (Diagnostic Accuracy Study)
Performance of the Index Test
The paediatrics resident blind to the details of history, general examination, and laboratory investigation findings of the study subject will be examined independently, and we will use the palpation and percussion to detect study subjects for Splenomegaly (Index text). To access the reliability of Splenomegaly, the other two paediatrics residents will evaluate each child independently and blinded, and 60 minutes-90 minutes interval between the observer’s examinations. All the patients will be examined in a fasting state or at least two hours after food intake by the following methods.
Palpation
• Supine Palpation Maneuver: The patient will be made to lie in the supine position. The examiner's fingertips of the right hand will gently press the abdomen just beneath the left costal margin, and then he/she will be asked to take in deep and long inspiration, and then the descending spleen palpation will be sought.
• Middleton's Hooking Maneuver: The patient is made to lie in the supine position and is approached from the left side with their first under the left cost over tebral angle. Fingers are to be hooked under the left costal margin. Then the patient is asked to inspire while the examiner tries to feel for the tip of the spleen.
• Right lateral decubitus and supine: The patient is made to lie in the right lateral decubitus position. Then the left hand of the examiner's left hand is slipped over from anterior to posterior around the left lower thorax, with the lowermost rib cage of the left side being lifted gently anterior and medially. The examiner’s fingertips of the right hand are then gently pressed from beneath the left costal margin, the patient is then asked to inspire take a long and deep breath, while the spleen is palpated. The palpatory methods will be scored on a five-point scale of Hackett's semi-quantitative system. [10-12]
Percussion
• Traube's space percussion: The child will be made to lie in a supine position with the left arm slightly abducted so that the entire Traube's space can be assessed. When the patient is respiring normally, the medial to lateral margins of the triangle will be percussed from one or more levels. Usually, on percussion, a resonant or tympanitic note is heard. If on percussion a dull note is heard then splenomegaly is diagnosed.
• Castell's maneuver: The child is made to lie in the supine position; the lowest left intercostals space in the anterior axillary line (usually the 8th or 9th intercostals space) is then percussed. Normally, this space is resonant on percussion during full inspiration. If on percussion a dull note is heard then possible splenomegaly.
• Nixon's maneuver: The child is made to lie in the right lateral decubitus position. Percussion is then begun midway along the left costal margin. Proceed in a line perpendicular to the left costal margin. If the upper limit of dullness exceeds more than 8 cm above the left costal margin, it indicates a possibility of splenomegaly. [11-13]
Performance of the Reference Standard
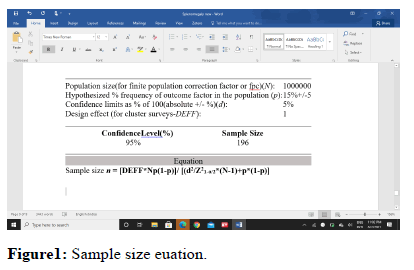
Abdominal Songraphy for Splenomegaly (Reference standard) will be carried out after the clinical examination of the children before starting treatment. All the patients included in the study will be made to undergo an assessment by ultrasonography for the size of the spleen on the same day by a radiologist, who is not aware of the clinical illness of the patient and also not aware of the observations made by the clinician, using a 3.5 to 5 MHz probe of the Philips Color Doppler system. The optically maximum distance at the hilum on the longitudinal coronal view (between the most superomedial and the most inferolateral locations) will be used to estimate spleen length, as this is the most reproducible linear measurement. [14,15] Younger children will have their measurements taken while breathing quietly, while older children will have their measurements taken while holding their breath. If the sonographic cephalocaudal diameter is 13 cms or greater, the spleen will be identified as enlarged [Figure 1].
Statistical methods
Data analysis is done with program STATA 10. Numerical information is summarized using standard deviations and means. The input and review of data are carried out using the program STATA. The proportions are evaluated using the chi-square test and the means are compared by student's ttest. The diagnostic accuracy of palpation and percussion for detecting ultrasonographically identified splenomegaly will be measured by computation of specificity, sensitivity, negative likelihood ratios (LR-), positive likelihood ratios (LR+), and negative and positive predictive values. 95% confidence intervals will be used to assess the precision of these estimations (95% CI).
Sensitivity and specificity measurements will be used to calculate likelihood ratios. A multilevel sensitivity and specificity estimate will be obtained, followed by the construction of a ROC curve to establish the ideal cut-off level for detecting a clinical sign. Between the pair of paediatric residents, ĸ statistic (a chance corrected measure of agreement) will be used to assess the reliability of physical findings.
Expected results
After completion of the study, we will come to know the diagnostic accuracy of the various clinical methods like palpatory methods (Supine Palpation Maneuver, Middleton's Hooking Maneuver, Right lateral decubitus and supine) and percussion methods (Traube's space percussion, Nixon's Maneuver, Castell's Maneuver) for detection of splenomegaly. We will able to know the specificity, sensitivity, LR-, LR+, PPV and NPV values of the each methods for the detection of the splenomegaly. We will also analyse the reliability of the methods of clinical assessment of the splenomegaly by three paediatrics resident.
Discussion
The clinical assessment of splenomegaly may be of immense importance in forming a diagnosis. Palpation and percussion both help in detecting the enlarged spleen. These methods appear to be complementary to each other. Yang JC et al in their study stated that an important aspect of physical examination is the evaluation of the patient for the presence of splenomegaly. [6] Even though there are various methods for percussion and palpation for the assessment of the spleen, they have not been validated by non-invasive imaging techniques such as ultrasonography, computed tomography, and radionuclide scanning. Godfried MH et al stated that physical examination low sensitivity and good specificity in detecting splenomegaly. [13] It also mentioned that, as compared to percussion, palpation is more sensitive and specific. Percussion findings often improve the accuracy of palpation. The specificity of the combination of both is around 90%. The prevalence of splenomegaly by ultrasonography (defined as a spleen > or = 13 cm on the longitudinal scan) was 33.3 percent, according to Tamayo SG et al. [16] The sensitivity and specificity of each palpation and percussion approach differed depending on the examiner. The sensitivity ranges for the 3palpatory and percussion methods were 0% -64.3 percent and 7.7% -75 percent, respectively, among examiners. The ranges of specificity across examiners were 50 percent -100 percent and 60 percent -100 percent, respectively for the 3 methods of palpation and percussion. Castell's approach showed the highest likelihood ratios for palpation, palpation from above, and percussion. The diagnostic accuracy was improved by a combination of tests of either palpation or percussion. Physical diagnostic approaches for the diagnosis of splenomegaly, although are insensitive but yet specific, according to Tamayo SG et al. [16] The accuracy of diagnosis is improved by combining tests.
Barkun AN et al in their study stated that by comparing the bedside examination maneuvers by their receiver operating characteristic curves, it was evident that percussion and palpation of Traube’s space were the significant discriminators of splenomegaly (p <0.001) with respective areas of 0.70 +/- 0.04 and 0.76 +/- 0.04. None of the methods of palpation were better than the other. [10] While it was also concluded upon that the palpation in the right decubitus position was not that useful when performed after palpation in the supine position. There wasn’t much difference in the sensitivity and specificity (79 percent and 46 percent respectively) of the splenic percussion sign as compared to Traube’s space percussion with sensitivity and specificity of 62 percent and 72 percent respectively in assessing the splenomegaly. On the contrary, the splenic palpation methods were more sensitive and specific than the percussion of the Traube’s space. In patients who exhibited dullness on percussion in the Traube’s space (area = 0.87 +/- 0.04, p less than 0.0001) demonstrated that the palpation was an important clinical discriminator. But, palpation had no or very less value when the percussion in the Traube’s space didn’t exhibit dullness (area = 0.55 +/- 0.08). The study then concluded that the ideal and adequate clinical evaluation of splenomegaly includes the Traube’s space percussion. Palpation of the spleen is required if percussion dullness is noted, with the accuracy best amongst the lean patients. Chongtham DS et al in their study of eighty subjects admitted to an education hospital noticed that the 2 methods of palpation, are namely, Supine palpation and Middleton's maneuver and 3 methods of percussion, namely Traube's space percussion, Castell's and Nixon's maneuvers were accurate in facilitating the diagnosis of splenic enlargement. [12] The gold standard for diagnosing splenic enlargement was considered to be the findings on Ultrasonography. Castell’s and Middleton's maneuvers had a similar percentage of sensitivity, that is 85.7 percentage, which was again more than that of the rest of the manoeuvers like Traube's space percussion, Nixon's maneuvers, and supine palpation. Amongst them, the least sensitive was Nixon's maneuver. Supine palpation had the highest specificity with a percentage of 92.1. While the least sensitive was Castell’s maneuver (31.6 percent). A maximum PPV was showed under the supine palpation with a percentage of 91.7. Chongtham DS et al stated that Supine palpation and Middleton’s maneuver are to be used for routine diagnosis of splenic enlargement. [12] Cessford T et al stated that the ultrasonography findings of Castell’s method and spleen tip technique have higher sensitivity and specificity than the traditional methods of clinical examination. [15] But they are more time-consuming and lower inter-rater reliability. When used along with physical examination techniques, radiological assistance can improve the accuracy of splenomegaly diagnosis. Splenomegaly is a common finding in children and can be caused by a large spectrum of diseases, including haematological diseases and infectious causes. Pelizzo G et al concluded that the recent concept of splenomegaly is not applicable in paediatric surgery. [17] It needs a separate splenomegaly classification for children and would improve the feasibility and safety of treatment. [18] Stewart KR et al concluded that the percussion and palpation techniques were not that sensitive and hence maybe not be adequate enough to rule out splenomegaly. But, at the same time also had high specificity in diagnosing splenomegaly. [19] Palpatory methods had higher positive likelihood ratios as compared to percussion methods, suggestive that palpation was better than percussion in diagnosing splenomegaly.
Conclusion
The study will probably give us adequate information about the accuracy of different methods of palpation and percussion for the detection of splenomegaly in children.
References
- Zhang B, Lewis SM. A study of the reliability of clinical palpation of the spleen. Clin Lab Haematol. 1989; 11: 7-10.
- Diagne I, Fall AL, Déme I, Sylla A, Coly JI, Camara B, et al.Epidemiology and course of splenomegaly in children and adolescents with sickle cell disease in Senegal. Arch Pediatr. 2010; 17:1017-1025.
- Abdullahi SU, Hassan-Hanga F, Ibrahim M. Ultrasonographic spleen size and haematological parameters in children with sickle cell anaemia in Kano, Nigeria. Niger Postgrad Med J. 2014; 21:165-170.
- Arshad K, Sheikh S, Naqvi SU, Sarwar I, Javaid S, Asghar M, et al. Frequency of splenomegaly in dengue fever in children. J Ayub Med Coll Abbottabad. 2015; 27:356-359.
- Megremis SD, Vlachonikolis LG, Tsilimigaki AM. Spleen length in childhood with US:Normal values based on age, sex and somatometric parameters. Radiology. 2004; 23:129-134.
- Yang JC, Rickman LS, Bosser SK. The clinical diagnosis of splenomegaly. West J Med. 1991; 155:47-52.
- Olatunji AA, Olatunji PO. Splenic size determination in sickle cell anaemia: an ultrasonographic study. East Afr Med J. 2001; 78:366-369.
- Ghosh K, Mukherjee MB, Surve RR, Shankarkumar U, Kate SL, Nagtilak SB, et al.Splenomegaly in school children in a remote tribal area of Dhole district, Maharashtra. Indian J Malariol. 2000; 37:68-73.
- Taksande A, Taksande B, Meshram R, Lohakare A, Jadhav. Study of Knowledge, Attitude and Practices regarding Malaria Prevention. Indian Journal of Communicable Diseases 2015; 1: 3-6.
- Barkun AN, Camus M, Green L, Meagher T, Coupal L, De Stempel J, et al. The bedside assessment of splenic enlargement. Am J Med. 1991; 91:512-518.
- Dubey S, Swaroop A, Jain R, Verma K, Garg P, Agarwal S. Percussion of Traube's space--a useful index of splenic enlargement. J Assoc Physicians India. 2000; 48:326-328.
- Chongtham DS, Singh MM, Kalantri SP, Pathak S. Accuracy of palpation and percussion manoeuvres in the diagnosis of splenomegaly. Indian J Med Sci. 1997; 51:409-416.
- Godfried MH, Briët E. Physical diagnosis--percussion and palpation of the spleen. Ned Tijdschr Geneeskd. 2000; 144:216-219.
- Rosenberg HK, Markowitz RI, Koelberg H, Park C, Hubbard A, Bellah RD. Normal splenic size in infants and children: sonographic measurements. AJR Am J Roentgenol. 1991; 157:119-121.
- Cessford T, Meneilly GS, Arishenkoff S, Eddy C, Chen LYC, et al. Comparing Physical Examination with Sonographic Versions of the Same Examination Techniques for Splenomegaly. J Ultrasound Med, 2018; 37:1621-1629.
- Tamayo SG, Rickman LS, Mathews WC, Fullerton SC, Bartok AE, et al. Examiner dependence on physical diagnostic tests for the detection of splenomegaly: a prospective study with multiple observers. J Gen Intern Med. 1993; 8:69-75.
- Pelizzo G, Guazzotti M, Klersy C, Nakib G, Costanzo F, Andreatta E, et al. Spleen size evaluation in children: Time to define splenomegaly for paediatric surgeons and pediatricians. PLoS One. 2018; 13:1-13.
- CurovicRotbain E, Hansen DL, Muckadell OSD, Wibrand F, Lund AM, Frederiksen H. Splenomegaly - Diagnostic validity, work-up, and underlying causes. PLoS One. 2017; 12:1-11.
- Stewart KR, Derck AM, Long KL, Learman K, Cook C. Diagnostic accuracy of clinical tests for the detection of splenomegaly. Physical Therapy Reviews. 2013; 18:173-184.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.