Drivers of Prenatal Care Quality and Uptake of Supervised Delivery Services in Ghana
- *Corresponding Author:
- Roger A. Atinga
Department of Public Administration and Health Services Management, University of Ghana Business School, P.O. Box LG 78, Legon, Accra, Ghana.
E-mail: ayimbillah@yahoo.com
Abstract
Background: In spite of the introduction of free maternal healthcare in Ghana, utilization of supervised delivery services continues to be low due partly to poor quality of antenatal care (ANC). Aim: The study sought to identify the determinants of perceived quality of ANC and uptake of skilled delivery services. Subjects and Methods: A total of 363 expectant mothers were randomly selected in urban health facilities for interview. Logistic regression models were computed to examine the relative odds of reporting quality of antenatal as good and the intention to receive skilled delivery care. Results: The odds of reporting ANC quality as good was high for women aged between 30 and 34 years. Perceived quality of ANC increases with increasing access to education but more likely to be higher for women attaining senior high education. Distance to the health facility influences quality perception, but the odds of reporting quality of care as good attenuated with proximity to the health facility. Finally, uptake of supervised delivery services was high for women aged between 35 and 39 years, women with at least junior high education; living close to the health facility and in their second and third trimester. Conclusion: Study’s findings demonstrate the need to improve the quality of maternal health services in public health facilities to encourage women to deliver under skilled care providers.
Keywords
Antenatal care, Expectant mothers, Ghana, Quality, Skilled care
Introduction
In response to the unacceptable maternal mortalities globally, particularly in developing countries, the United Nations in 2000 established an agreed universal framework of international development goals and targets known as the millennium development goals (MDGs) to be pursued by governments and civil society to meet the needs of people in the poorest parts of the world by 2015. Eight goals were adopted, but goal five, the focus of this study seeks to improve maternal health with two targets: To reduce by three-quarters maternal mortality rate (MMR) and secondly, to achieve universal access to reproductive health services.[1]
The MDGs deadline is almost due and progress toward improving maternal health has been at best staggering. Reports suggest that in 2008, there were approximately 358,000 maternal deaths or a MMR of 260 deaths/100,000 live births world-wide.[2] Out of this number, developing countries accounted for 99% (355,000), with the highest MMR of 290 in stark contrast to the developed nations which is 14.[2] Within the context of developing regions, Sub-Saharan Africa (SSA) has the highest MMR (640/100,000) suggesting that achieving goal five of the MDGs - halving maternal deaths by two-thirds is practically impossible.[3]
The slow pace of reducing maternal deaths despite the MDGs implementation raises pessimistic questions about the capacity of health systems in the developing regions to find sustainable means of improving maternal health. More often strategies to improve maternal health are constrained by inadequate skilled birth attendants and under funding of maternal and child health programs.[4,5] Other factors obstructing progress towards improving maternal health include barriers of access to healthcare, inadequate essential supplies, lack of emergency transport systems and poor referral services.[6]
The presence of user fees or nominal payment for maternal health services in some health systems also decreases women capacity to utilize maternal health services. This often results in increases in health risks especially among pregnant women. The tendency to suffer greater health risks arising out of under-utilization is particularly high for women within the poorest wealth quintile[7-9] who lack control over resources to cater for the cost of services, drugs, equipment and transportation.[10-12] On account of the far-reaching problems associated with out-of-pocket payment for obstetric services, the government of Ghana introduced a maternal care exemption fee policy in 2007 to eliminate the financial burden of access to maternal health services in order to reduce maternal and neonatal mortalities.[13] The exemption fee policy was later incorporated into the country’s health insurance scheme and the benefit package was expanded to incorporate antenatal, delivery and postpartum care.
In spite of the fee abolishing, many women continue to deliver at home instead of health facilities. Evidence suggests that about 95% of women in Ghana receive some antenatal care (ANC), yet only 57% have their deliveries in health facilities.[14] Similar findings have been reported in other countries that although most women seek ANC at least once during pregnancy, only a small proportion of them deliver in health facilities.[15,16] In Ghana, delivering at home without the assistance and supervision of a qualified midwife or doctor is considered to be the ideal situation and an easy way of delivery.[17]
Several studies have revealed that one of the factors responsible for non-utilization of supervised delivery services in Ghana is the provision of poor quality of care.[18-20] About 83% of delivery services in facilities especially at the primary level do not meet standard clinical practices[21] suggesting that trade-off between home and facility based delivery is to be expected. Quality is rarely matched with women expectations, resulting in negative correlation between ANC attendance and utilization of supervised delivery services. Among all the quality variables, attitude of health professionals cows potential users of institutional delivery services. As it has been documented women feel reluctant to seek future care in health facilities when their experience with health professionals is negative.[22,23]
Quality of prenatal or ANC is defined as the structures put in place to deliver care, the process within which care is delivered and the impact of services to expectant mothers.[24] Other supply side factors such as prompt diagnosis and treatment, skilled staff availability, convenient operating hours, adequate clinical equipment and drug availability determine quality of ANC.[25] The presence of these institutional variables can stimulate the use of ANC and consequently influence uptake of supervised delivery services.
To ensure improved facility-based deliveries, research directed at quality of ANC from expectant mothers’ perspective is necessary. This will enable decision-makers to have a clear understanding of the situation and hence commit more resources and advocate for appropriate changes to health service provision.[26] However, in Ghana developing a reliable quality monitoring system for maternal care has remained a challenge. This is further worsened by inadequate evidence base research to support strengthening of maternal health service delivery.[27]
Located in the West Africa Sub-Region, Ghana has made conscious efforts to increase ANC coverage and trains more health professionals to handle deliveries in primary health facilities. Total fertility rate has declined from 6.4 in 1988 to 3.92 in 2012.[28] However the maternal mortality ratio remains marginally high (350/100,000). ANC coverage for at least four visits is extrapolated to be 78.2%[28] suggesting that some women either do not visit antenatal health providers at all during pregnancy or fail to meet the recommended minimum number of four visits. Therefore improving the quality of obstetric care should form an integral part of efforts to encourage antenatal visits and subsequent delivery in health facilities.
In practice, all women who desire to have babies would like to do so safely with reassurance and care throughout their pregnancy, delivery and puerperal period.[29] Thus, improving access and strengthening the quality of antenatal services are significant strategies toward reducing maternal mortalities.[30] Against the background of high preference for home instead of institutional deliveries, this paper set out to examine factor associated with quality of ANC and uptake of skilled delivery services in Ghana.
Subjects and Methods
The study was conducted in public health facilities in the Accra Metropolitan Assembly (AMA) of the Greater Accra region. The selection of Accra Metropolis was necessitated by the fact that many studies about institutional deliveries, quality of maternity care and health seeking behavior among women have been directed at the rural settings.[17,19,20,31,32] Attention toward urban areas is rare though the causes of maternal mortalities in rural communities also manifest in urban settings.
AMA is the most populous area of the Greater Accra region, largely because it is home for the seat of government and center for major commercial activities. AMA is made up of 11 sub-metros each of which is treated as an administrative district. In spite of the growing population density in the metropolis, coverage of public health facilities remains low with people living in the slums and some indigenous communities being the worse served. There are fewer than 10 public referral hospitals unevenly distributed across the sub-metros. Some of the sub-metros are best served with at least two public hospitals while some have just one hospital. Quasi government hospitals also operate to augment the volume of services provided by public hospitals.[33] However, this is not enough to bridge the gap between demand and supply.
Six sub-metros were randomly selected for the study. Health facilities were selected using different sampling methods. Where a sub-metro had at least two public hospital, only one was randomly selected. On the other hand we purposively selected the main referral public hospitals in sub-metros with just one hospital. In all, a total of six public facilities representing two polyclinics and four hospitals were selected.
Ethical approval was sought from the Ghana Health Service. The study focused on expectant mothers reporting for ANC in the selected health facilities. At the time of conducting the study, average ANC utilization in the polyclinics and hospitals was 101 and 198 respectively. Therefore, we randomly selected 200 women (50 in each polyclinic) and 164 women (82 in each hospital) for interview. The aggregate sample size was 363. In the sampled health facilities, exit interviews (i.e., interviewing respondents after they have completed receiving care) were employed to collect data. Exit interviews were found to be suitable since the absence of providers enabled respondents freely articulate their opinions without fear of being judged. The purpose of the study was explained to secure the consent of each participant before interviews were conducted.
To empirically assess the factors associated with ANC quality and uptake of skilled delivery services, a structured questionnaire was used. The questionnaire contained information relating to the womens socio-demographic characteristics-age, education, religion, occupation, trimester and distance from the woman’s home to the health facility.
Two outcome variables were included in the questionnaire. The first outcome variable which sought to assess the quality of prenatal care was measured by the attitude of midwives; drug availability; duration of waiting hours; availability of essential medical equipment and comfort of the service environment. Considering the nature of their condition, expectant mothers would expect to be treated humanely in culturally sensitive and friendly manner during a visit to the health facility.[18] Therefore explicit concern from health providers expressed through good interaction with expectant mothers may increase their preference for continuous uptake of antenatal services and subsequent delivery in the health facility. Further when essential medical equipment and logistics are nominally available, it offers minimal confidence for women to access care much more birthing in the health facility. Responses to item measures of the outcome variable, quality of ANC were dichotomous (1 = good if woman perceived service delivery to meet her expectation; 0 = poor if otherwise). The second outcome variable, intention to deliver in the health facility was assessed by asking the respondents whether they would be willing to deliver in the health facility based on their experience on quality of ANC in the health facilities. This outcome variable was dichotomous (1 = Yes if woman expressed willingness to deliver in the health facility; 0 = No if otherwise).
A two-part binary logistic regression was computed to determine association between the women demographic characteristics and the outcome variables, quality of prenatal represented by model 1 and the intention to deliver in the health facility, model 2. Binary logistic regression is generally used to test the relationship between a binary dependent variable and a set of independent variables.[34]
Chi-square (?2) test of independence was further used to explore possible relationships between the various independent variables and the frequency of antenatal visits. The aim was to find out whether the independent variables and frequency of antenatal visits are independent. The World Health Organization recommends at least four visits for normal pregnancies, the first of which should occur within the first trimester.[35] In this study, the number of antenatal visits was at most nine.
Results
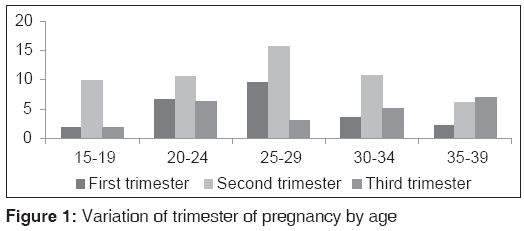
Descriptive statistics of the respondents are captured in Table 1. Many of the women (28.4%, 103/363) were aged between of 25 and 29. The majority, 87.9% (319/363) of the women had at least primary education. There were more Christians, 83.5% (303/363) than Muslims 16.5% (60/363). A greater number, 43.8% (159/363) of the women were self-employed. About 23% (82/363) and 18% (64/363) were respectively employed in the private and public sectors while 16.0% (58/363) were unemployed. A Large proportion, 52.9% (192/363) of the women were in their second trimester. The average distance to the nearest health facility from the woman’s home was 4.32 km. Many women across the different age sub-groups were in their second trimester [Figure 1]. Women perception about the quality of ANC was mixed. 54.4% (198/363) rated quality of ANC as good while 45.5% (165/363) indicated otherwise. An overwhelming number 71.9% (261/363) reported that they will seek skilled delivery care. Results in Table 2 show Chi-square analysis of the relationship between background characteristics of women and number of antenatal visits. Three variables, education, religion and occupation are significantly associated to antenatal visits.
| n (%) | |
|---|---|
| Age (years) | |
| 15-19 | 50 (13.8) |
| 20-24 | 85 (23.4) |
| 25-29 | 103 (28.4) |
| 30-34 | 70 (19.3) |
| 35-39 | 55 (15.2) |
| Education | |
| None | 44 (12.1) |
| Primary | 99 (29.3) |
| Junior/senior high | 176 (48.5) |
| Higher | 44 (12.1) |
| Religion | |
| Christian | 303 (83.5) |
| Muslim | 60 (16.5) |
| Occupation | |
| Public sector | 64 (17.6) |
| Private sector | 82 (22.6) |
| Self employed | 159 (43.8) |
| Unemployed | 58 (16.0) |
| Trimester | |
| First | 87 (24.0) |
| Second | 192 (52.9) |
| Third | 84 (23.1) |
| Distance to health facility (km) | |
| 1-3 | 93 (25.6) |
| 4-6 | 135 (37.2) |
| 7-9 | 60 (16.5) |
| 10+ | 76 (20.7) |
Table 1: Characteristics of respondents
| Number of antenatal visit N (%) | ?2 | P value | |||||
|---|---|---|---|---|---|---|---|
| 1-2 | 3-4 | 5-6 | 7-8 | 9+ | |||
| Age (years) | |||||||
| 15-19 | 24 (6.6) | 9 (2.5) | 4 (1.1) | 9 (2.5) | 4 (1.1) | 13.067 | <0.01 |
| 20-24 | 40 (11.0) | 16 (4.4) | 13 (3.6) | 10 (2.8) | 6 (1.7) | ||
| 25-29 | 38 (10.5) | 25 (6.9) | 21 (5.8) | 11 (3.0) | 8 (2.2) | ||
| 30-34 | 26 (7.2) | 14 (3.9) | 16 (4.4) | 6 (1.7) | 8 (2.2) | ||
| 35-39 | 24 (6.6) | 8 (2.2) | 11 (3.0) | 5 (1.4) | 7 (1.9) | ||
| Education | |||||||
| None | 24 (6.6) | 6 (1.7) | 8 (2.2) | 3 (0.8) | 3 (0.8) | 25.643 | <0.01 |
| Primary | 39 (10.7) | 22 (6.1) | 21 (5.8) | 10 (2.8) | 7 (1.9) | ||
| Junior/senior high | 72 (19.8) | 40 (11.0) | 32 (8.8) | 20 (5.5) | 12 (3.3) | ||
| Higher | 17 (4.7) | 4 (1.1) | 4 (1.1) | 8 (2.2) | 11 (3.0) | ||
| Religion | |||||||
| Christian | 118 (32.5) | 61 (16.8) | 55 (15.2) | 39 (10.7) | 30 (8.3) | 9.257 | <0.01 |
| Muslim | 34 (9.4) | 11 (3.0) | 10 (2.8) | 2 (0.6) | 3 (0.8) | ||
| Occupation | |||||||
| Public sector | 33 (9.1) | 7 (1.9) | 9 (2.5) | 3 (0.8) | 12 (3.3) | 22.867 | <0.01 |
| Private sector | 33 (9.1) | 16 (4.4) | 14 (3.9) | 12 (3.3) | 7 (1.9) | ||
| Self employed | 64 (17.6) | 35 (9.6) | 27 (7.4) | 23 (6.3) | 10 (2.8) | ||
| Unemployed | 22 (6.1) | 14 (3.9) | 15 (4.1) | 3 (0.8) | 4 (1.1) | ||
| Distance to health facility (km) | |||||||
| 1-3 | 35 (9.6) | 18 (5.0) | 22 (6.1) | 12 (3.3) | 6 (1.7) | 9.230 | 0.21 |
| 4-6 | 55 (15.2) | 28 (7.7) | 19 (5.2) | 18 (5.0) | 15 (4.1) | ||
| 7-9 | 31 (8.5) | 11 (3.0) | 8 (2.2) | 5 (1.4) | 5 (1.4) | ||
| 10+ | 31 (8.5) | 15 (4.1) | 16 (4.4) | 6 (1.7) | 7 (1.9) | ||
Table 2: Chi-square test of the relationship between the independent variables and number of antenatal visits
To investigate the association between women characteristics and quality of ANC a binary logistic regression was computed [Table 3]. The model contained 6 independent variables: Age, education, religion, occupation, pregnancy status and distance from woman’s home to the health facility. The results show significant association between quality of ANC and women aged between 30 and 34 years (P < 0.01). Perceived quality of antenatal services is higher among women attaining junior/senior high education (OR = 1.52; P < 0.01) compared to women with higher education (OR = 1.28; P = 0.04). The odds of reporting quality of ANC as good was high for private sector workers (OR = 3.4; P < 0.01) and the unemployed (OR = 2.47). Distance is associated with perceived quality of ANC, but this increases with increasing distance to the health facility. Women living far from the health facility were more likely to perceive quality of ANC as good in contrast with those who lived closed to the health facility (OR = 2.22).
| Explanatory variables | Model 1 (quality of ANC) | Model 2 (delivering in health facility) | ||||
|---|---|---|---|---|---|---|
| Coefficients | OR | CI (95%) | Coefficients | OR | CI (95%) | |
| Age (years) | ||||||
| 15-19† | ||||||
| 20-24 | -0.231 | 0.793 | 0.291-1.160 | -0.163 | 0.849 | 0.332-2.172 |
| 25-29 | -0.199 | 0.820 | 0.339-1.983 | -0.111 | 1.118 | 0.504-2.477 |
| 30-34 | 0.130** | 1.931 | 0.455-2.847 | -0.558 | 0.573 | 0.255-1.287 |
| 35-39 | -0.238 | 0.788 | 0.317-1.957 | 2.007** | 2.134 | 0.045-4.400 |
| Education | ||||||
| None† | ||||||
| Primary | -0.441 | 0.643 | 0.222-1.859 | 0.866 | 1.378 | 0.760-7.437 |
| Junior/senior high | 0.120** | 1.527 | 0.442-2.873 | 0.912* | 2.588 | 0.914-6.776 |
| Higher | 0.246* | 1.279 | 0.529-3.092 | 0.212** | 3.236 | 0.472-6.238 |
| Religion | ||||||
| Christian† | ||||||
| Muslim | 0.278 | 1.321 | 0.673-2.594 | -1.045** | 0.352 | 0.178-1.694 |
| Occupation | ||||||
| Public sector† | ||||||
| Private sector | 1.226** | 3.409 | 1.323-8.782 | -0.747 | 0.474 | 0.192-1.168 |
| Self employed | 0.520 | 1.682 | 0.782-3.619 | -0.467 | 0.627 | 0.280-1.404 |
| Unemployed | 0.905** | 2.472 | 1.217-5.021 | -0.473 | 0.623 | 0.302-1.285 |
| Trimester of pregnancy | ||||||
| First† | ||||||
| Second | 0.564 | 1.759 | 0.788-3.923 | 0.880* | 2.411 | 1.091-5.329 |
| Third | 0.420 | 1.522 | 0.811-2.855 | 0.498** | 3.645 | 0.828-6.268 |
| Distance to health facility (km) | ||||||
| 1-3† | ||||||
| 4-6 | 0.797** | 2.219 | 1.063-4.632 | 0.272* | 1.638 | 0.602-2.862 |
| 7-9 | 0.856** | 3.353 | 1.187-4.665 | 0.494 | 1.513 | 0.793-3.385 |
| 10+ | 1.470** | 4.351 | 1.723-10.990 | -1.014 | 0.363 | 0.135-1.973 |
| Constant | -0.804 | 0.448 | -0.332 | 0.718 | ||
| ?2(16) | 35.353 | 59.484 | ||||
| Probability >?2 | 0.000 | 0.000 | ||||
| Pseudo R 2 | 0.139 | 0.217 | ||||
| Log likelihood | -364.454 | -371.679 | ||||
Table 3: Logistic regression results of the relative odds of reporting quality of ANC as good and delivering in the health facility
Table 3 presents results of association between women characteristics and the intention to deliver in the health facility. The relative odds of delivering in the health facility is greater for women aged between 35 and 39 years (OR = 2.13). Access to higher education increases the probability of birthing in the health facility (OR = 3.24; P < 0.01) reflecting greater knowledge about the importance of skilled delivery care. In addition, women with junior/senior high education were more likely to deliver in the health facility (OR = 2.49) compared to those with primary level of education (OR = 1.38). The odds of delivering in the health facility is also high for women in their third trimester (OR = 3.65) than the second trimester (OR = 2.41). Distance to the health facility is not significantly associated with uptake of skilled delivery care. However, the relative odd of delivering in the health facility is higher for women living far from the health facilities studied.
Discussion
The study found that quality of ANC was perceived to be good among women aged between 30 and 34 years. A possible explanation is that as women advance in age they tend to perceive service delivery differently. Education has been shown to influence women health seeking behavior particularly, utilization of obstetric services.[34,36,37] Association between women education and perceived quality of ANC remains obscured in the literature however. This study discovered significant association between access to education and quality of care perception.
Women with low educational status have a negative perception about the quality of ANC. In our view, is not surprising given that reproductive health seeking behavior in Ghana is greatly impeded by low levels of women education and status.[38] The fact that highly educated women tended to hold a positive view about the quality of ANC imply that they are likely to better understand the dynamics of healthcare delivery and that enabled them coped with service providers even if they faced problems in the care seeking process. Women working in the private sector were about three times more likely to report quality as good in contrast to the unemployed who were twice more likely to report similar episode. A woman’s trimester of pregnancy does not affect perception about the quality of prenatal care. However, the odds of reporting quality of care as good was high for those in their second trimester. This may be attributed to the fact that the second trimester is normally less associated with complications and health risk comparable to the first and third. Relative stable health conditions may therefore influence service quality perception.[14] Healthcare managers should consider improving shortfalls of service delivery to create a balance of quality perceptions across all trimesters. In particular, attention should be paid to establishing structures that would enable women of all trimesters feel comfortable during the health seeking process.
The relative odds of reporting quality of ANC as good diminished with proximity to the health facility. For instance women living 10 km and beyond from the health facility highly reported ANC quality as good compared to those whose lived closed to the health facilities. Essentially, proximity of health facilities to users may be a key determinant of antennal visit,[39-44] but not quality perception. Perhaps excessive consumption of maternal services by women closer to the health facilities might have generated diminishing marginal utility of quality perception. More detail analysis using qualitative methods is needed to provide further understanding of this phenomenon. In the meantime service quality improvement is required to bridge the gap of quality perceptions between women closer and far from health facilities.
The provision of maternal health services with sufficient quality increases the chances of women delivering under the supervision of skilled providers. The reverse can however produce undesirable consequences, including for example, increases in the number of home deliveries and maternal mortalities. Maternal deaths can be prevented if women have access to quality health services so that complications can easily be managed.[45] Therefore understanding the factors shaping facility based deliveries is important to plan appropriately for policy interventions.
In line with one of the key objective of this study which is to identify factors associated with uptake of supervised delivery services, it was discovered that the likelihood of delivering in the health facilities studied was high for women aged between 35 and 39 years. Implying that as women advances in age, they become more conscious about the relevance of receiving supervised delivery services. Younger women were more likely to deliver at home[46] contrary to findings of an earlier study that young women have a preference for skilled delivery care.[47] In Ghana, many women have weak social status representing loss opportunity to make independent decisions about reproductive health issues.[48] More especially, young women who are pushed down the pecking order of many households are often constrained in terms of autonomy to take decisions concerning the choice of delivery place. Thus when decision regarding choice of facility delivery cannot be immediately agreed upon by the partner or family in the event of active labor, the only option is to deliver at home.
Consistent with previous studies, education has emerged as a significant determinant of supervised delivery.[9,39,47,49-51] This finding further provides support for previous studies that education plays an important role in accomplishing better reproductive health outcome.[52,53] In general, highly educated women have been demonstrated to have the power to override collective family decisions and therefore can opt for institutional delivery services even if they face opposition from within and outside the family.[54]
In the Ghanaian context where decision-making is mostly male dominated, education is seen as an empowerment tool against which women can contribute to decision making relating to their health and healthcare utilization. Therefore this finding reinforces the need to make girl child education paramount in national development policies. Pursuing enrolment and retention among girls in school could have both short and long-term benefits. Firstly, it increases the knowledge of women regarding reproductive health matters and secondly, it enables women overcome both family and societal factors constraining utilization of maternal health services. Occupation in its all forms is negatively associated with the intention to deliver under skilled care providers. The probability of perceiving quality of ANC as good was high for women engaged in the private sector and the unemployed. Such women expressed no strong intention to deliver in the health facility however. It is difficult to fully account for this phenomenon in this study. However private sector workers often better paid are well placed to appraise and select the optimal mix of supervised delivery services. This may not be the same for the unemployed without regular income source.
The intention to deliver in the health facility also reflects in the woman’s trimester, but this is more likely to be high for women in their second and third trimesters. Given the scope of the study, it is not possible to fully explore the normative reasons behind this phenomenon. Nonetheless, the fact that pregnant women in their second and third trimester are often more accustomed to information relating to reproductive health risk and the danger of delivering at home,[14] serve as an incentive for them to deliver in the health facility.
We found that uptake of supervised delivery services increases with decreasing distance to the health facility, corroborating findings of previous studies that physical distance influences utilization of skilled delivery services.[55-57] In effect, women living far from the health facilities held low opinions about future intention of receiving supervised delivery services. This could be partly linked to the opportunity cost of time, cost associated with transportation, drugs, equipment and services. This finding necessitates expanding facilities coverage to the under-served backed by well-resourced maternity units to facilitate access to reproductive health services. Alternatively, the government and policy makers should consider making social interventions such the metro mass transport system free for all expectant mothers not living close to health facilities in order to alleviate household catastrophic expenditure.
Conclusion
Findings of the study indicated that not all women of the different socio-demographic backgrounds perceived quality of ANC to be good neither did all of them express intention to deliver in the health facility. Policy implications of the study are specified supra, but it is important to stress that, the myth surrounding home deliveries may be broken when health providers offer sufficient quality of ANC and policy makers take steps to scale-up coverage of maternal care to encourage facility based deliveries.
A limitation of the study relate to the non-inclusion of income and parity which are seen as important in any analysis of maternal healthcare utilization. Future research should consider incorporating these variables to observe for possible changes. The sample size is also small considering the larger numbers of women utilizing antenatal services in the AMA. Future researchers interested in this subject matter should consider increasing the sample size.
Acknowledgment
This research was supported by funding from benevolent individuals to whom we are very much grateful. The views expressed in this paper are those of the authors and do not necessarily reflect that of the funding parties.
Source of Support
Nil.
Conflict of Interest
None declared.
References
- Hill K, Thomas K, AbouZahr C, Walker N, Say L, Inoue M, et al. Estimates of maternal mortality worldwide between1990 and 2005: An assessment of available data. Lancet 2007;370:1311-9.
- WHO, UNICEF, UNFPA, World Bank. Trends in Maternal Mortality 1990-2008. WHO, 2010. Available from: http://www. whqlibdoc.who.int/publications/2010/9789241500265_eng. pdf. [Last cited on 2013 Jan 23].
- De Allegri M, Ridde V, Louis VR, Sarker M, Tiendrebéogo J, Yé M, et al. Determinants of utilisation of maternal care services after the reduction of user fees: A case study from rural Burkina Faso. Health Policy 2011;99:210-8.
- Nyonator F, Kutzin J. Health for some? The effects of user fees in the Volta Region of Ghana. Health Policy Plan 1999;14:329-41.
- Garshong B, Ansah E, Dakpallah G, Huijts I, Adjei S. A study on factors affecting the implementation of the exemption policy in Ghana. Bulletin of Health Information 2002; 1:22–31.
- World Health Organization (WHO). World Health Report 2005: Make Every Mother and Child Count. Geneva: WHO; 2005.
- Graham WJ, Fitzmaurice AE, Bell JS, Cairns JA. The familial technique for linking maternal death with poverty. Lancet 2004;363:23-7.
- O’Donnell O. Access to health care in developing countries: Breaking down demand side barriers. Cad Saude Publica 2007;23:2820-34.
- Gill K, Pande R, Malhotra A. Women deliver for development. Lancet 2007;370:1347-57.
- Ensor T, Cooper S. Overcoming barriers to health service access: Influencing the demand side. Health Policy Plan 2004;19:69-79.
- Ensor T, Ronoh J. Effective financing of maternal health services: A review of the literature. Health Policy 2005;75:49-58.
- McNamee P, Ternent L, Hussein J. Barriers in accessing maternal healthcare: Evidence from low-and middle-income countries. Expert Rev Pharmacoecon Outcomes Res 2009;9:41-8.
- Witter S, Arhinful DK, Kusi A, Zakariah-Akoto S. The experience of Ghana in implementing a user fee exemption policy to provide free delivery care. Reprod Health Matters 2007;15:61-71.
- Akazili J, Doctor HV, Abokyi L, Hodgson A, Phillips FP. Is there any relationship between antenatal care and Place of delivery? Findings from rural northern Ghana. Afr J Health Sci 2011;18:62-73.
- Amooti-Kaguna B, Nuwaha F. Factors influencing choice of delivery sites in Rakai district of Uganda. Soc Sci Med 2000;50:203-13.
- Lugina H, Mlay R, Smith H. Mobility and maternal position during childbirth in Tanzania: An exploratory study at four government hospitals. BMC Pregnancy Childbirth 2004;4:3.
- Bazzano AN, Kirkwood B, Tawiah-Agyemang C, Owusu-Agyei S, Adongo P. Social costs of skilled attendance at birth in rural Ghana. Int J Gynaecol Obstet 2008;102:91-4.
- D’Ambruoso L, Abbey M, Hussein J. Please understand when I cry out in pain: Women’s accounts of maternity services during labour and delivery in Ghana. BMC Public Health 2005;5:140.
- Ansong-Tornui J, Armar-Klemesu M, Arhinful D, Penfold S, Hussein J. Hospital based maternity care in ghana-findings of a confidential enquiry into maternal deaths. Ghana Med J 2007;41:125-32.
- Bosu W, Bell JS, Armar-Klemesu M, Tornui JA. Effect of delivery care user fee exemption policy on institutional maternal deaths in the central and Volta regions of Ghana. Ghana Med J 2007;41:118-24.
- Hussein J, Bell J, Nazzar A, Abbey M, Adjei S, Graham W. The skilled attendance index: Proposal for a new measure of skilled attendance at delivery. Reprod Health Matters 2004;12:160-70.
- Kruk ME, Mbaruku G, McCord CW, Moran M, Rockers PC, Galea S. Bypassing primary care facilities for childbirth: A population-based study in rural Tanzania. Health Policy Plan 2009;24:279-88.
- Magoma M, Requejo J, Campbell OM, Cousens S, Filippi V. High ANC coverage and low skilled attendance in a rural Tanzanian district: A case for implementing a birth plan intervention. BMC Pregnancy Childbirth 2010;10:13.
- World Health Organization (WHO). Maternal Health and Safe Motherhood Programme, Division of Family Health: Mother Baby Package. Geneva: WHO; 1996.
- Sharan M, Ahmed S, Ghebrehiwet M, Rogo K. The quality of the maternal health system in Eritrea. Int J Gynaecol Obstet 2011;115:244-50.
- Kerber KJ, de Graft-Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: From slogan to service delivery. Lancet 2007;370:1358-69.
- Atinga RA, Baku AA. Determinants of antenatal care quality in Ghana. Int J Soc Econ 2013;40:852-65.
- WHO. Country profile of Ghana, 2013. Available from: http://www.apps.who.int/gho/data/node.country. country-GHA. [Last accessed on 2013 Nov 18].
- Koblinsky M, Matthews Z, Hussein J, Mavalankar D, Mridha MK, Anwar I, et al. Going to scale with professional skilled care. Lancet 2006;368:1377-86.
- Bennet V, Brown LM. Text Book for Midwives. 13th ed. London: Churchill-Livingstone; 1997.
- Jansen I. Decision making in childbirth: The influence of traditional structures in a Ghanaian village. Int Nurs Rev 2006;53:41-6.
- Guerts KL. Well-Being and Birth in Rural Ghana: Local Realities and Global Mandates. Paper Presented at the Fifth Annual Penn African Studies Workshop; October 17, 1997. Available from: http://www.africa.upenn.edu/Workshop/ geurts.html. [Last cited on 2012 Nov 10].
- Ghana Health Service: 2008 Review of Sector Performance in the Greater Accra region. Accra, Ghana: Ghana Health Service; 2008.
- Huq MN, Tasnim T. Maternal education and child healthcare in Bangladesh. Matern Child Health J 2008;12:43-51.
- Villar J, Ba’aqeel H, Piaggio G, Lumbiganon P, Miguel Belizán J, Farnot U, et al. WHO antenatal care randomised trial for the evaluation of a new model of routine antenatal care. Lancet 2001;357:1551-64.
- Addai I. Determinants of use of maternal-child health services in rural Ghana. J Biosoc Sci 2000;32:1-15.
- Paruzzolo S, Mehra R, Kes A, Ashbaugh C. Targeting poverty and gender inequality to improve maternal health. International Centre for Research on Women; 2010. Available from: http://www.womendeliver.org. [Last cited on 2011 Apr 04].
- Ngom P, Debpuur C, Akweongo P, Adongo P, Binka FN. Gate-keeping and women’s health seeking behaviour in Navrongo, northern Ghana. Afr J Reprod Health 2003;7:17-26.
- Hall MF, Press I. Keys to patient satisfaction in the emergency department: Results of a multiple facility study. Hosp Health Serv Adm 1996;41:515-32.
- McKinley RK, Manku-Scott T, Hastings AM, French DP, Baker R. Reliability and validity of a new measure of patient satisfaction with out of hours primary medical care in the United Kingdom: Development of a patient questionnaire. BMJ 1997;314:193-8.
- Gabrysch S, Campbell OM. Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy Childbirth 2009;9:34.
- Johnson FA, Padmadas SS, Brown JJ. On the spatial inequalities of institutional versus home births in Ghana: A multilevel analysis. J Community Health 2009;34:64-72.
- Hounton S, Chapman G, Menten J, De Brouwere V, Ensor T, Sombié I, et al. Accessibility and utilisation of delivery care within a Skilled Care Initiative in rural Burkina Faso. Trop Med Int Health 2008;13 Suppl 1:44-52.
- Gage AJ. Barriers to the utilization of maternal health care in rural Mali. Soc Sci Med 2007;65:1666-82.
- Thaddeus S, Maine D. Too far to walk: Maternal mortality in context. Soc Sci Med 1994;38:1091-110.
- Ochako R, Fotso JC, Ikamari L, Khasakhala A. Utilization of maternal health services among young women in Kenya: Insights from the Kenya Demographic and Health Survey, 2003. BMC Pregnancy Childbirth 2011;11:1.
- Mrisho M, Schellenberg JA, Mushi AK, Obrist B, Mshinda H, Tanner M, et al. Factors affecting home delivery in rural Tanzania. Trop Med Int Health 2007;12:862-72.
- Smith ME, Tawiah EO, Badasu DM. Why some women deliver in health institutions and others do not: A cross sectional study of married women in Ghana, 2008. Afr J Reprod Health 2012;16:36-47.
- Fotso JC, Ezeh AC, Essendi H. Maternal health in resource-poor urban settings: How does women’s autonomy influence the utilization of obstetric care services? Reprod Health 2009;6:9.
- Beegle K, Frankenberg E, Thomas D. Bargaining power within couples and use of prenatal and delivery care in Indonesia. Stud Fam Plann 2001;32:130-46.
- Sharma SK, Sawangdee Y, Sirirassamee B. Access to health: Women’s status and utilization of maternal health services in Nepal. J Biosoc Sci 2007;39:671-92.
- Munsur AM, Atia A, Kazuo K. Relationship between educational attainment and maternal health care utilization in Bangladesh: Evidence from the 2005 Bangladesh household income and expenditure survey. Res J Med Sci 2010;4:33-7.
- Basu AA. Why does education lead to lower fertility? A critical review of some of the possibilities. World Dev 2002;30:1779-90.
- Tchibindat F, Martin-Prevel Y, Kolsteren P, Maire B, Delpeuch F. Bringing together viewpoints of mothers and health workers to enhance monitoring and promotion of growth and development of children: A case study from the Republic of Congo. J Health Popul Nutr 2004;22:59-67.
- Hodgkin D. Household characteristics affecting where mothers deliver in rural Kenya. Health Econ 1996;5:333-40.
- Bolam A, Manandhar DS, Shrestha P, Ellis M, Malla K, Costello AM. Factors affecting home delivery in the Kathmandu Valley, Nepal. Health Policy Plan 1998;13:152-8.
- Yanagisawa S, Oum S, Wakai S. Determinants of skilled birth attendance in rural Cambodia. Trop Med Int Health 2006;11:238-51.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.