Early Discontinuation of Long Acting Reversible Contraceptives among Married and in Union Women: A Systematic Review and Meta-analysis
Citation: Tadele Girum Adal. Early Discontinuation of Long Acting Reversible Contraceptives among Married and in Union Women: A Systematic Review and Meta-analysis. Ann Med Health Sci Res. 2017; 7: 113-118
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Despite the improvement in availability and utilization of long acting reversible contraception early discontinuation is becoming a public health concern. Significant proportion of women discontinues the service before its due date which poses a concern in the health system and its consequence may leads to failure of a program. Therefore Estimating the rate of discontinuation from the available reports and identifying the associating factors are important for designing a strategy to overcome the problem. Methods: The review was conducted through a systematic literature search of articles published between 1997 and 2017. Five Most known bibliographic databases and libraries: PubMed/Medline, Global Health Database, Embase, the Cochrane Library, and African Index Medicus were used. After cleaning and sorting, analysis was performed using STATA version 11. The pooled rate of early discontinuation was estimated with a random-effects model. Heterogeneity was assessed by the I2 and publication bias through funnel plot. Results: The 22 studies that were retained for final analysis enrolled a total of 19,805 Married or in union women. Accordingly, 20% (95% CI=17-23%) of women discontinue long acting reversible contraceptives within one year of insertion. There is no significant difference in the rate of discontinuation between IUD and implant users (20.6% (SD=12.7) and 20.2% (SD=7.9)). Side effects and health concerns were main determinants for early discontinuation. Conclusion and recommendation: Contraceptive discontinuation rate in this meta-analysis was found to be much higher than previous studies and world health organization’s report associated with adverse outcomes and inconveniences. There for appropriate counseling, follow up care and management of side effects and clients inconveniences are very important
Keywords
Family planning service; Intrauterine device; Etonogestrel; Implanon
Introduction
In the past four decades organized international and national effort has made great progress in expanding the availability and use of family planning services, reducing unmet need and addressing special needs. [1] In 2015, 64 percent of married or in-union women of reproductive age women worldwide were using some form of contraception. Of these 57 percent used a modern method of family planning, constituting 90 percent of contraceptive users and a larger share of them are reversible long acting contraceptive users. Intra uterine device (IUD) is one of the most commonly used methods by married or in-union women worldwide, used by among 14 percent of women. [2-4]
Advances in contraceptive technologies over the last few decades have resulted in the availability of most effective and safe long acting reversible modern contraceptives; like copper bearing and levonorgestrel-releasing IUDs and implants which are easier to insert and remove and convenient for users and effectively prevent pregnancy; they are cost-effective for programs over time, can result in substantial cost savings for governments, and contribute directly to reaching national and international health goals. [5,6]
For many women, long-term reversible contraception is an excellent choice. [7,8] It is also the strategy and preferred program for world health organization and many member countries. These methods can enhance FP programs in meaningful ways if the challenges to their availability, access, and acceptability can be overcome. [9] In countries with high fertility rate and unmet need of contraceptives, shifting towards long acting reversible contraception (LARC) is an important strategy to ensure continuity of services. It also helps to meet the need for spacing and limiting births which has the potential to prevent thousands of cases of maternal mortality further by preventing annually occurring 80 million unintended pregnancies among women who are not using contraception. [10,11]
Despite the improvement in availability and utilization of long acting reversible contraception early discontinuation is becoming a major problem. Significant proportion of women discontinues the service within one year even without any side effect. [12] According to a report based on developing countries, 13.1% of IUD users discontinue its use during the first 12 months, 26.3% within 24 months, and 36.7% by the third year of its use. The discontinuation of IUD within the first 12 months ranges from 13% to 47% and Implanon discontinuation within the first year ranges from 2% in Nigeria to 23% in UK. [13,14]
From the available limited research it was indicated that sideeffects and health concerns like irregular bleeding, lower abdominal pain, and vaginal discharge play an important role in discontinuation. while Secio-demographic variables (Level of parity or need for more children, preferred family size, sex preference, reason for use, religious concern) along with health care related variables (appointed for follow, quality of care, satisfaction, counseling) were also contributed for early discontinuation. [15-17]
Higher discontinuation rate of long acting contraception is a public health concern; it is also failure of a program. Long acting contraceptives which designed to use for 3-12 year are coast effective only when they serve for the intended period of time. Along with their health impact the economic impact of Early discount of long acting contraceptives are very high. Therefore measuring the rate of discontinuation and identifying the associating factors are important for programme planning and designing a strategy to overcome the problem.
Materials and Methods
Literature search strategy
In accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses: guidance for reporting of systematic reviews and meta analyses) [18] guide line this systematic review was conducted through a systematic literature search of articles published between 1997 and 2017 containing information on early termination of long acting modern contraception and their associated factors among married and in union women. Five Most known bibliographic databases and libraries: PubMed/Medline, Global Health Database, Embase, the Cochrane Library, and African Index Medicus were used. Key words from Medical Subject Headings (MeSHs): long acting contraceptives, reversible contraception, Intra uterine device, implant, early termination, discontinuation were used with (AND, OR, NOT) Boolean (Search) Operators. In addition the references of each primary researches and reviews were screened and citations were uploaded into an EndNote XI library (EndNote, Carlsbad, CA, USA) and checked for duplications.
Selection /eligibility criteria
The studies included in this review were limited to publications in English language that reported long acting contraception; intrauterine device, and any type of implants and/or both for cohorts of at least 100 women who are married or in union without geographic demarcation. Also Studies were eligible regardless of design and setting provided that they fulfill the inclusion criteria. However studies reporting the overall contraceptive termination or discontinuation were excluded to avoid over reporting which is common in short acting contraceptives. The outcome of interest was early discontinuation of long acting reversible contraception with in the period of one year of use. Studies conducted in the same location during the same time period were considered as potential duplicates and therefore excluded from the analysis.
Data extraction and abstraction
The data included in this review were derived through the electronic search of published papers, titles and abstracts after filtered for potential eligibility. If needed, and wherever possible, the authors were contacted for clarifications. From each eligible research, the following information was extracted based on the preformed database (Excel, Microsoft, 2010) format: about author, study participants, studies (study design, cohort size, setting), Type of contraception, length of use, year of publication, year of study start and end, eligibility criteria, etc. All data were extracted independently and in duplicate using a standardized extraction form. Returned abstracts were reviewed and full texts retrieved if they contained relevant information. Mean way, each selected research was assessed for methodological quality and possibility of bias.
Data analysis
After cleaning and sorting the final database was exported into Stata 11.0 for analysis (Stata, College Station, TX, USA). An outcome of interest was rate of early termination before or at 12th month of use. Estimates of early discontinuation were assessed for each study and standardized mean with 95% confidence interval was used. These were calculated with a random-effects model according to the DerSimonian and Laird method. [19] Heterogeneity was assessed by the I2 and values greater than 50% considered representing significant heterogeneity. When heterogeneity between studies was found to be significant, pooled estimates were based on random-effect models and the Hedges method of pooling. Results were displayed visually in forest plots. Bias was investigated by construction of funnel plots and Analysis was performed using the ‘metan’ and related functions in STATA version 11 (College Station, TX).
Results
Studies included
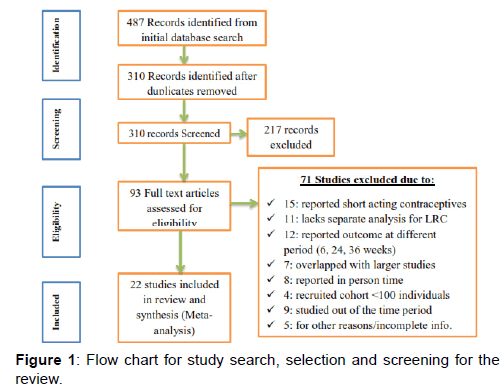
The search initially identiï¬Âed 487 citations from electronic database in the form of abstract, bibliography and citation; all citations were transferred to endnote and cleaned for duplications and 93 articles were identified for full text review. Of the 93 articles reviewed in full text, 22 articles were analyzed based on the inclusion-exclusion criteria and quality assessment and 71 studies were removed prior to analysis for different reasons: 15 studies reported the finding of short acting contraceptives, 11 removed for lack of separate analysis for short acting and long acting contraception, 12 removed for reporting out come at different period (6, 24 and 36 months only), 7 overlapped with larger studies, 8 reported outcome in terms of person year of follow up, 4 studies had recruited cohorts less than 100 individuals, 9 studies were out of time period and 5 were removed for other reasons; either not specified settings [Figure 1].
Description of Findings
The 22 studies that were retained for final analysis reported the rate of early discontinuation of long acting reversible contraception for a total of 19,805 Married or in union women, with a range of 106-6153 women in each study. These women were followed for at least a year prior to the study and the studies were published during the period 2005–2017. Of these studies 9 were cross-sectional, 1 was case study and 12 were cohort. Eleven studies assed IUD discontinuation alone, 9 studied Implant discontinuation and 2 assessed both IUD and implant discontinuation. Ten studies were conducted in Asia, five in Africa, four in Europe, two in North America and one in Australia. Survey characteristics are described in Table 1.
| Study | Year | Country | Design | Type | ES | SS |
|---|---|---|---|---|---|---|
| Sebash Tagash [20] | 2012 | Nepal | Retrosp/Cohort | IUD | 21.3 | 230 |
| Azmat et al. [21] | 2012 | Pakistan | Cross-sectional | IUD | 18 | 2789 |
| Theai et al. [22] | 2010 | Philippines | Cross-sectional | IUD | 11.2 | 1347 |
| Ali Navidian et al. [23] | 2016 | Iran | Cross-sectional | IUD | 23.85 | 260 |
| O'Nail-callahan et al. [24] | 2013 | USA | Cohort | Both | 13 | 6153 |
| Carolineharvey et al. [25] | 2009 | Australia | Retrosp/Cohort | Implant | 26 | 976 |
| ACQUIRE project [26] | 2007 | Bangladesh | Retrosp/Cohort | IUD | 47.3 | 300 |
| Melese Seyoum [27] | 2017 | Ethiopia | Cross-sectional | Implant | 23.9 | 348 |
| Teunissen et al. [28] | 2013 | Netherlands | Retrosp/Cohort | Implant | 28 | 214 |
| Anjali Agrawal [29] | 2005 | UK | Case study | Implant | 30.2 | 106 |
| Kalayu Birhane [30] | 2015 | Ethiopia | Cross-sectional | Implant | 16 | 244 |
| Nyguyen TH [31] | 2011 | Vietnam | Retrosp/Cohort | IUD | 12.2 | 1316 |
| Sharma et al. [32] | 2014 | India | Retrosp/Cohort | IUD | 16.8 | 387 |
| Janine Barden [33] | 2011 | Honduras | Cross-sectional | IUD | 41 | 671 |
| Subha et al. [34] | 2015 | India | Retrosp/Cohort | IUD | 5.97 | 251 |
| Bhatia et al. [35] | 2011 | India | Cross-sectional | Implant | 18.5 | 200 |
| N.H.Madugu et al. | 2015 | Nigeria | Cross-sectional | Both | 25.6 | 625 |
| C.Moreau et al. [36] | 2009 | France | Prosp/Cohort | IUD | 15 | 702 |
| Ezagwui et al. [38] | 2011 | Nigeria | Retrosp/Cohort | Implant | 8.1 | 295 |
| Adegbela et al. [38] | 2008 | Nigeria | Retrosp/Cohort | IUD | 13.9 | 1602 |
| Arribas-Mir et al. [40] | 2009 | Spain | Cross-sectional | Implant | 9 | 372 |
| Otero Flores et al. [41] | 2005 | Mexico | Prosp/Cohort | Implant | 21.8 | 417 |
ES = Effect Size [Percentage of Discontinuation], SS = Sample Size, IUD = Intrauterine Contraceptive Device
Table 1: Characteristics of studies included in the review.
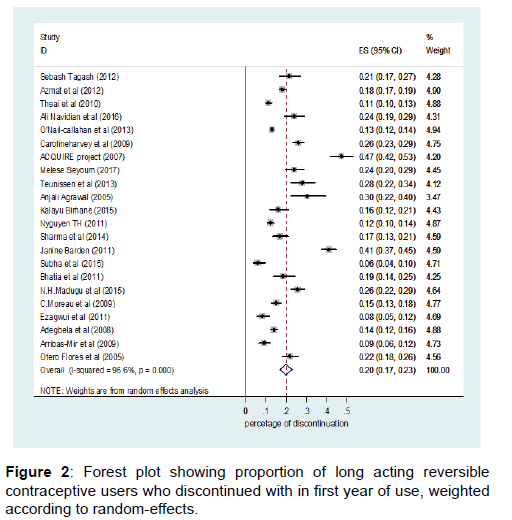
For all populations, percentage of early discontinuation (with in the first year) ranged from 6% to 47.3%, with a mean of 20.3% (SD=10.2). IUD discontinuation ranged from 6% in India to 47.3% in Bangladesh with a mean of 20.6% (SD=12.7) and Implant discontinuation ranged from 8.1% in Nigeria to 30.2% in United Kingdom with a mean of 20.2% (SD=7.9). There is no significant difference in the rate of discontinuation between IUD and implant users. Only three studies reported discontinuation rate of below 10%; in India IUD discontinuation rate of 6% (95% CI=4-10%), in Nigeria implant discontinuation rate of 8% (95% CI=5-12%) and in Spain implant discontinuation rate of 9% (95% CI=6-12%). Similarly three studies reported discontinuation rate of above 30% [Figure 2].
Pooled estimates and tests
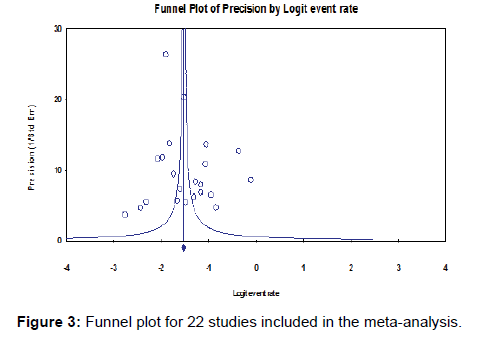
Heterogeneity tests showed significant variations between studies (Q=617.8, P=0.000), where Q-value, the weighed sum of squares on a standardized scale was significantly different compared with expected weighed sum of squares and I-squared showed that 96.6% of the observed dispersions are attributed to real rather than spurious variations. Also the funnel plot showed evidence of bias with some of the studies missing at the bottom rather than around the main effect [Figure 3]. Accordingly, the Duval and Tweedie’s trim and fill test was applied to adjust for the publication bias.
The presence of heterogeneity and publication bias therefore resulted in adjustment of the point estimate of the percentage of discontinuation under a random effect model from 15% to 20%. In a fixed effect model the pooled estimate of discontinuation rate was 15% (95% CI=15-16%) and in a random effect model the pooled estimate of discontinuation rate became 20% (95% CI=17-23%), while estimates of each study are unchanged. In all cases pooled estimate from random effect model was used for report and discussion.
Discussion
Contraceptives are used by the majority of married or in-union women in almost all regions of the world. Modern contraceptive methods constitute most contraceptive use in the current statistics. These High levels of contraceptive prevalence reflect availability of different mixtures of methods, but long-acting reversible methods play a prominent role. Significant proportion of married or in union women prefers to use reversible long acting contraceptives. [2-4]
All available types of contraception have both strengths and weaknesses, and no method is medically suitable, appropriate and acceptable for all couples in all circumstances. However, long acting reversible contraceptives are best preferences for most women for delaying or spacing births. Current advancements in contraceptive technology and health care system made this contraceptives to have less side effects, less failure and technically easy for insertion and removal. In order to avoid financial barriers for use many countries provide the service free of coast, which created additional opportunity. [4,13,14]
However, since Individuals are vary in their experience of and tolerance for side effects of highly effective modern methods as well as in their willingness to tolerate the inconveniences, and ability of health professionals to provide quality service, counseling clients and appointing follow up, early discontinuation of long acting reversible contraceptives created another threat for the service. Unless the contraceptives are retained in place until their service year, all advantages of long acting reversible contraceptives: coast effectiveness and efficacy remains under question. [8,11,13]
From previous studies it was reported that significant proportion of mothers discontinue long acting contraception use within a short period of time. The discontinuation rate varies from country to country; however there is no estimate made based on reviewing available researches throughout the world which could estimate the overall rate of discontinuation. Therefore this study evaluated 22 researches [20-41] and estimated the pooled discontinuation rate of long acting reversible contraception.
According to this study, 20% (95% CI=17-23%) of women discontinue long acting reversible contraceptives within one year of insertion. The rate of discontinuation in the first year in the study was higher as compared with a survey conducted among women of 14 developing countries which was 13.2%. [13] Also in line to Mohamed Ali’s report [14] huge inter-country variations in the probability of stopping contraception use were observed, which may have contributed to the difference observed between our estimate and the survey report in developing countries.
After 12 months more than 30% of women had discontinued their contraception in the three studies. Forty seven percent (95%CI=42-47) of women in Bangladesh, 41% (95%CI=37-45) of women in Honduras and 30% (95%CI=22-40) of women in United Kingdom [26,29,33] had discontinued their contraception with in the first year of insertion. On the other hand three studies had reported a discontinuation rate of less than 10%. Six percent (95% CI=4-10%) of women from Subha et al. [34] report, 8% (95% CI=5-12%) of women from Ezagwui et al. [38] report and 9% (95% CI=6-12%) of women from Arribas-Mir et al. [40] report had discontinued their contraception within one year of insertion. This difference may be ascribed to difference in design, setting and difference in the health care system.
However, in contrast to pronounced inter-country differences, discontinuation does not vary appreciably between the two types of long acting contraception users. In the study 20.6% (SD=12.7) IUD users and 20.2% (SD=7.9) of implant users had discontinued with in the first year of insertion. Thus the methods are equally suitable and proportionally posed a side effect among women all around the world. When a method supposed to be serving for 10-12 years and implant expected to serve for 3-5 year are removed early within one year of insertion, the loss to health care system is very high. [4,8] The other impact is when women discontinue early they may not have another alternatives for spacing which may causes unwanted pregnancy. [13,14]
Along with socio-economic determinants planned pregnancy was reported as one of the most common reason for discontinuation of all methods of contraception. This review found that side effect ascribed to IUD and Implants like vaginal bleeding, infection, and menstrual abnormalities was the major reason for discontinuation and desire to have child, expulsion, failure and method switch contributed a lot. This finding is in line to many of previous studies conducted abroad. [26,29,34,40]
Conclusions and Recommendation
Contraceptive discontinuation rate in this meta-analysis was found to be much higher than previous studies and world health organization’s report from survey reports. This higher level of discontinuation may substantially contribute to high fertility rate, unwanted pregnancies, and induced abortions. Also early termination of long acting contraception makes the method less coast effective. Side effects associated with the method itself and the procedure, expulsion, failure and other similar inconveniences contributed for discontinuation. There for appropriate counseling, follow up care and management of side effects along with information on contraceptive effectiveness, insertion and removal procedures are very important.
Conflict of Interest
All authors disclose that there was no conflict of interest.
REFERENCES
- Jacobstein R. Long Acting and Permanent Contraception: An International Development, Service Delivery Perspective. J Midwifery Womens Health. 2007; 52: 361-367.
- United Nations, Department of Economic and Social Affairs, Population Division (2015). Trends in Contraceptive Use Worldwide 2015 (ST/ESA/SER.A/349).
- Scoggins & Bremner (2016). FP2020 momentum at the midpoint 2015-2016. http://progress.familyplanning2020.org/.
- UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP). Annual Technical Report 2015.
- Family Health International. Addressing Unmet Need for Family Planning in Africa. 2007. Accessed on 29/12/2016];Available from: http://www.k4health.org/ system/files/ unmetneed for FP_Africa. pdf
- Kulier R, O’Brien PA, Helmerhorst FM, Usher-Patel M, D’Arcangues C. Copper containing, framed intra-uterine devices for contraception. Cochrane Database Syst Rev 2007(4): CD005347.
- Speizer IS, Nanda P, Achyut P, Pillai G, Guilkey DK. Family planning use among urban poor women from six cities of uttar pradesh, India. J Urban Health. 2012; 89: 639-658.
- WHO. WHO joins call for renewed focus on Family Planning, Geneva, Switzerland, 11 July 2012. Brown. Available: http://www.who.int. Global health Europe, WHO joins call for renewed focus on Family Planning, Geneva, Switzerland.
- Takele A, Degu G, Yitayal M. Demand for long acting and permanent methods of contraceptives and factors for non-use among married women of Goba Town, Bale Zone, South East Ethiopia. Reprod Health 2012; 9:26.
- Peterson HB, Curtis KM. Long-Acting Methods of Contraception. New England journal of medicine 2005; 353: 2169-2175.
- Zlidar VM. 3. New survey findings: the reproductiverevolution continues. Baltimore: Johns Hopkins Bloomberg School of Public Health, 2003.
- Blane A, Curtis S, Croft T. Does contraceptive discontinuation matter? Quality of care and fertility consequences. MEASURE Evaluation Technical Report No. 3.: University of North Carolina at Chapel Hill: Carolina Population Center, 1999.
- Ali, Mohamed M, Sadler Rachael K, Cleland John, Ngo Thoai D, Shah Iqbal H. Long term contraceptive protection, discontinuation and switching behaviour: intrauterine device (IUD) use dynamics in 14 developing countries. London: World Health Organization and Marie Stopes International, 2011.
- Mohamed Ali, John C, Iqba Shah. Couse and consequence of contraceptive discontinuation: evidence from 60 demographic and health surveys. World health organization, 2012.
- Asari VG. Determinants of contraceptive use in Kerala: the case of son/daughter preference. J Fam Welf. 1994; 40: 19-25.
- Youssef RM. Contraception use and probability of continuation: community-based survey of women in southern Jordan. East Mediterr Health J. 2005; 11: 545-558.
- Bhat PN, Halli SS. Factors influencing continuation of IUD use in South India: evidence from a multivariate analysis. J Biosoc Sci. 1998; 30: 297-319.
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group, 2009. Preferred reporting items for Systematic reviews and metaanalyses: the PRISMA statement. PLoS Med 6: e1000097.
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986; 7: 177-188
- Sebash Tagash. Early discontinuation of intrauterine device in Nepal – a retrospective study. WHO South-East Asia Journal of Public Health 2012; 1: 309-319.
- Azmat et al. Rates of IUCD discontinuation and its associated factors among the clients of a social franchising network in Pakistan. BMC Women’s Health 2012 12:8.
- Ngo TD, Pernito VL: Discontinuation of IUCDs among women receiving mobile outreach services in the Philippines, 2006-2008. Marie Stopes International, London; 2009.
- Hassan R, Azizollah A, Ali N, Hossein G. Analysis of the Continuation Rates of Intrauterine Device (IUD) and Three Month Injectable Depot Medroxy-progesterone Acetate (DMPA)Uses and Reasons for Their Discontinuation in Women Referred to Health Centers. Der Pharmacia Lettre, 2016; 8: 233-238.
- O’Neil-Callahan, Jeffrey F, Qiuhong Z, Tessa M, Gina S. Twenty-Four–Month Continuation of Reversible Contraception. Obstet Gynecol 2013; 122: 1083-1091.
- Harvey C, Seib C, Lucke J. Continuation rates and reasons for removal among Implanon users accessing two family planning clinics in Queensland, Australia. Contraception. 2009; 80: 527-532.
- Mahboob El-Alam, Searing H, Bradley J, Shabnam F. IUD use and discontinuation in Bangladesh. New York; The Acquire Project, 2007.
- Melese S, Zerfu M, Mulunesh A, Habtamu K. Implanon Discontinuation Rate and Associated Factors among Women who ever Used Implanon in the Last Three Years in Debre Markos Town, Northwest Ethiopia, 2016, Cross Sectional Study. ARC Journal of Public Health and Community Medicine; 2017.
- Teunissen A, Bernd G, Frans J, Roumen M. Continuation rates of the sub dermal contraceptive Implanon and associated influencing factors. Eur J. of Contracept Reprod Health Care; 2013
- Anjali A, Christine R. An assessment of the first 3 years' use of Implanonin Luton. J Fam Plann Reprod Health Care 2005; 31: 310-312.
- Kalayu B. Seifu H, Mesganaw F. Early Discontinuation Rate of Implanon and its Associated Factors among Women who ever Used Implanon In Ofla district, Tigray, Northern Ethiopia. Int Journal of Pharma Sciences and Research. 2015; 6.
- Park MH, Nguyen TH, Ngo TD. Dynamics of IUD use in Vietnam: Implications for family planning services at primary health care level. Int J Womens Health 2011; 3: 429-434.
- Sharma M, Joshi S, Nagar O, Sharma A. Determinants of Intrauterine Contraceptive Device Discontinuation Among Indian Women. J Obstet Gynaecol India. 2014; 64: 208-211.
- Janine B, Ilene S. What Differentiates Method Stoppers from Switchers? Contraceptive Discontinuation and Switching Among Honduran Women. Int Perspect Sex Reprod Health, 2011; 37: 16-23.
- Aruna Subha Shree Rao Yellayi, Aruna S, Sarada Bai K. A Study on acceptance and discontinuation of intrauterine contraceptive device and its determinants in a tertiary care centre”. Int J Evid Based Healthc, 2015; 2: 3804-3811.
- Bhatia P, Nangia S, Aggarwal S, Tewari C. Implanon: Subdermal Single Rod Contraceptive Implant. J Obstet Gynaecol India. 2011; 61: 422-425.
- Madugu NH, Abdul MA, Bawa U, Kolawole B. Uptake of Hormonal Implants Contraceptive in Zaria, Northern Nigeria. Gynecol Obstet Res. 2015; 5: 268-273.
- Moreau C, Bouyer J, Bajos N, Rodríguez G, Trussell J. Frequency of discontinuation of contraceptive use: Results from a French population-based cohort. Hum Reprod. 2009; 24: 1387-1392.
- Ezegwui H, Ikeako L, Ishiekwene C, Oguanua T. The discontinuation rate and reasons for discontinuation of implanon at the family planning clinic of University of Nigeria Teaching Hospital (UNTH) Enugu, Nigeria. Niger J Med. 2011; 20: 448-450.
- Adegbola O, Ogedengbe O. The acceptance rate of intrauterine contraceptive device (IUCD) amongst family planning clinic users in Lagos University Teaching Hospital (LUTH). Nig Q J Hosp Med. 2008;18: 175-180.
- Arribas-Mir L, Rueda-Lozano D, Agrela-Cardona M. Insertion and 3-year follow-up experience of 372 etonogestrel subdermal contraceptive implants by family physicians in Granada, Spain. Contraception. 2009; 80: 457-462.
- Otero Flores JB, Lozano BM, Cortes BM. Clinical experience and acceptability of the etonogestrel subdermal contraceptive implant. Int J of Gynecology and Obstetrics. 2005; 90: 228-233.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.