Educational Interventions in Type 2 Diabetes Mellitus Patients in Primary Health Care: Systematic Review and Meta-analysis
2 Imam University, Riyadh City, Saudi Arabia
3 King Faisal University, Alahsa City, Saudi Arabia
4 Alfarabi Colleges, Riyadh City, Saudi Arabia
5 Prince Sultan Cardiac Center Al Hassa, Hofuf City, Saudi Arabia
6 Prince Sattam Bin Abdulaziz University, Riyadh city, Saudi Arabia
7 Umm Al qura University, Makkkah City, Saudi Arabia
8 King Faisal General Hospital, Alahsa, Alahsa City, Saudi Arabia
Citation: Alluhaymid YM, et al. Educational Interventions in Type 2 Diabetes Mellitus Patients in Primary Health Care: A Systematic Review and Meta-analysis. Ann Med Health Sci Res. 2021;11: 1217-1221.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Diabetes self-management education (DSME) is a critical part of diabetes care. Guidelines for the treatment of diabetes recommend that all diabetes patients must take part in DSME to enhance clinical outcomes and quality of life. Aim: This work aims to assess the impact of educational interventions in type 2 Diabetes Mellitus (DM) patients in primary health care. Materials and Methods: A systematic search was performed over different medical databases to identify Family Medicine studies, which studied the outcome of the Interventional group versus the Control group of primary health care DM patients. Using the meta-analysis process, either with fixed or random-effects models, we conducted a meta-analysis on HbA1C difference as the main outcome measure. Results: Ten studies were identified involving 3335 patients, with 1635 patients in the Interventional group, and 1700 patients in the Control group. The meta-analysis process revealed a highly significant decrease in mean HbA1C in the Interventional group compared to the Control group (p = 0.001). Conclusion: To conclude, educational interventions in primary care addressing T2DM could be effective for metabolic control, but the low quality of the evidence and the lack of measurement of critical results generate uncertainty and highlight the need for high-quality trials.
Keywords
Educational Interventions; Diabetes Mellitus; Primary Health Care
Introduction
Diabetes mellitus has a high prevalence worldwide, leading to problems such as increased mortality and health costs. There were 387 million cases of diabetes in 2014 and 415 million in 2015. [1] Type 2 diabetes mellitus especially a consequence of the presently experienced sedentary lifestyle and the marked boom in weight problems all over the globe. Type 2 diabetes mellitus is associated with excessive morbidity and mortality, as it’s far the main reason for kidney insufficiency, blindness, and non-traumatic amputations. Also, it represents a fundamental risk factor for cardiovascular sickness, the main purpose of mortality in diabetic patients. [2]
Diabetes self-management education (DSME) is a critical part of diabetes care. Guidelines for the treatment of diabetes recommend that all diabetes patients must take part in DSME to enhance clinical outcomes and quality of life. DSME can help type 2 diabetes sufferers improve the knowledge, skills, and capability of self-control cost-effectively. Numerous systematic evaluations have advised that DSME can improve patients’ self-management and blood glucose manipulate, and it needs to seem like a crucial element within the treatment of diabetes. DSME could lead to more than 0.4% reduction in hemoglobin A1C (HbA1c) of type 2 diabetes patients, extra than 5 mg/ dl reduction in general cholesterol, and more than 1 mmol/L reduction in fasting blood glucose. However, these systematic evaluations targeted brief-time period outcomes, but the effect of DSME on long-time period consequences, such as all-cause mortality, had not been sufficiently assessed. [3]
The importance of self-management of T2DM has gained increasing attention among researchers and clinicians. Good self-management can lessen the complication rate and enhance the best of life of patients. There were some systematic reviews to summarize the results of self-control education on T2DM patients, whilst studies focused on the consequences of theory-based self-management interventions. Theory-based interventions in diabetes self-control had been gaining interest from researchers. Increasing proof indicates that public fitness and health-promotion interventions that are based totally on social and behavioral science theories are more powerful. To support this practice with robust evidence, a systematic evaluation of randomized controlled trials (RCTs) examining the effectiveness of theory-based self-control educational interventions on T2DM sufferers was undertaken. [4]
This work aims to assess the impact of educational interventions in type 2 Diabetes Mellitus (DM) patients in primary health care.
Literature Review
Our review came following the (PRISMA) statement guidelines. [5]
Study eligibility
The included studies should be in English, a journal published article, and a human study describing primary health care DM patients. The excluded studies were non-English or animal studies.
Study identification
Basic searching was done over the PubMed, Cochrane library, and Google scholar using the following keywords: Educational Interventions, Diabetes Mellitus, Primary Health Care.
Data extraction and synthesis
RCTs, clinical trials, and comparative studies, which studied the outcome of the Interventional group versus Control group of primary health care DM patients, will be reviewed. Outcome measures included the HbA1C difference as the main outcome measure.
Study selection
We found 250 records, 185 excluded based on title and abstract review; 65 articles are searched for eligibility by full-text review; 25 articles cannot be accessed; 13 studies were reviews and case reports; the desired protocol not used in 17 studies leaving 10 studies that met all inclusion criteria.
Statistical analysis
After the pooling of data, Standard Mean Differences (SMDs), with 95% confidence intervals (CI) were calculated, using MedCalc statistical software (Belgium). After the Q test of heterogeneity, the I2-statistics (either the fixed-effects model or the random-effects model) were done within the meta-analysis process.
Results
The included studies were published between 2012 and 2020 [Table 1]. [6-15]
| N | Author | Number of patients | Age (average years) |
Follow-up time (average months) |
||
|---|---|---|---|---|---|---|
| Total | Interventional group | Control group | ||||
| 1 | Khunti et al. [6] | 604 | 332 | 272 | 57.6 | 36 |
| 2 | Adachi et al. [7] | 193 | 100 | 93 | 61 | 6 |
| 3 | DePue et al. [8] | 268 | 104 | 164 | 55 | 12 |
| 4 | Thom et al. [9] | 236 | 122 | 114 | 57 | 6 |
| 5 | Mash et al. [10] | 866 | 391 | 475 | 55 | -- |
| 6 | Grillo et al. [11] | 137 | 69 | 68 | 62 | 12 |
| 7 | Jutterström et al. [12] | 182 | 97 | 85 | 64.5 | 12 |
| 8 | Islam et al. [13] | 279 | 145 | 134 | 55 | 6 |
| 9 | Moreno et al. [14] | 518 | 249 | 269 | 64 | 24 |
| 10 | Dehghan Nayeri et al. [15] | 52 | 26 | 26 | 62 | -- |
| #Studies arranged via publication year | ||||||
Table 1: Patients and study characteristics.
Regarding patients’ characteristics, the total number of patients in all the included studies was 3335 patients, with 1635 patients in the Interventional group, and 1700 patients in the Control group, while their average follow-up time was (14 months) [Table 1]. The mean age of all patients was (59.3 years) [Table 1].
A meta-analysis study was done on 10 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=3335) [Table 2]. [6-15]
| N | Author | Main outcome | |||
|---|---|---|---|---|---|
| HbA1C difference | |||||
| Interventional group | SD | Control group | SD | ||
| 1 | Adachi et al. [7] | 7 | 2.2 | 7.7 | 1.9 |
| 2 | DePue et al. [8] | 6.7 | 1.2 | 7 | 1 |
| 3 | Thom et al. [9] | 9.6 | 2.1 | 10 | 2.3 |
| 4 | Mash et al. [10] | 8.98 | 2 | 9.55 | 2.3 |
| 5 | Grillo et al. [11] | 8.4 | 2 | 8.8 | 2.2 |
| 6 | Jutterström et al. [12] | 8.8 | 1.9 | 9.1 | 2 |
| 7 | Islam et al. [13] | 7.99 | 0.9 | 9.98 | 0.8 |
| 8 | Moreno et al. [14] | 7.6 | 1.2 | 8 | 1.6 |
| 9 | Dehghan Nayeri et al. [15] | 7.1 | 1.2 | 7 | 1.2 |
| 10 | Adachi et al. [7] | 8.7 | 0.63 | 9.8 | 0.83 |
Table 2: Summary of outcome measures in all studies.
Each outcome was measured by:
Standard Mean Difference (SMD)
• For HbA1C difference.
Concerning the main outcome measure, we found 10 studies reported HbA1C difference with a total number of patients (N=3335).
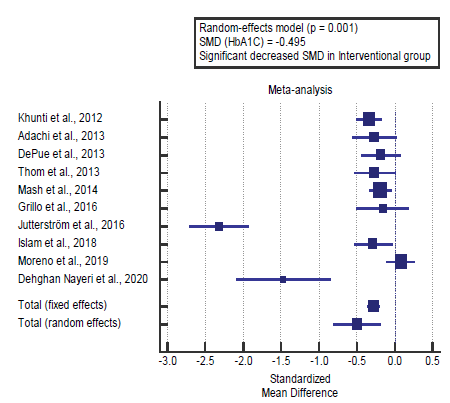
I2 (inconsistency) was 93.9% with a highly significant Q test for heterogeneity (p<0.001), so random-effects model was carried out; with overall SMD= -0.495 (95% CI =-0.791 to -0.198) [Figure 1].
Using the random-effects model, the meta-analysis process revealed a highly significant decrease in mean HbA1C in the Interventional group compared to the Control group (p=0.001) [Figure 2].
Discussion
This work aims to assess the impact of educational interventions in type 2 Diabetes Mellitus (DM) patients in primary health care. The included studies were published between 2012 and 2020.
Regarding patients’ characteristics, the total number of patients in all the included studies was 3335 patients, with 1635 patients in the Interventional group, and 1700 patients in the Control group, while their average follow-up time was (14 months).
The mean age of all patients was (59.3 years). A meta-analysis study was done on 10 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=3335).
Concerning the main outcome measure, we found 10 studies reported HbA1C difference with a total number of patients (N=3335).
Using the random-effects model, the meta-analysis process revealed a highly significant decrease in mean HbA1C in the Interventional group compared to the Control group (p=0.001). Which came in agreement with Garcia-Molina et al., [2] Ali & Al-Saadi, [16] Cortez et al., [1] Trief et al., [17] Gonzalez-Zacarias et al., [18] He et al., [3] Zhao et al., [4] Caro-Bautista et al. [19] and Saleh et al. [20]
Garcia-Molina et al. reported that a total of 28 researches were included. They demonstrated that life-style interventions significantly reduced glycosylated hemoglobin (HbA1c) levels in comparison to the usual care for patients with type 2 diabetes mellitus, normal weighted mean difference, WMD=− 0.51 (− 0.67, − 0.35). Strategies combining individualized and groupbased activities were the most effective, WMD=− 0.95 (− 1.24, − 0.66). Maximum of stratified analyses did not resolve heterogeneity, but improvement in HbA1c levels has been consistently observed. [2]
Ali & Al Saadi reported that all of 70 sufferers completed the observation (35 patients inside the intervention group and 35 patients inside the control group). At baseline, the intervention and control group had been comparable and there was no sizable difference (p>0.05) among values of the 2 groups concerning age, gender, education status, family records with DM, duration of DM, complications, and type of therapy, body mass index. For the manage group concerning FBG, HbA1C, TG, and cholesterol at baseline and the end of examination results found out the non-big distinction in each of FBG (P=0.497), HbA1C (P= 0.11), TG (p= 0.177) and LDL cholesterol (p=0.36). While in response to the pharmaceutical care intervention, results on the end of the examination for the intervention group, compared with the baseline, revealed a statistically significant reduction (P<0.05) in all FBG, HbA1C, TG, and cholesterol. [16]
Cortez et al. reported that there were 238 participants: 127 and 111 in the intervention and control group, respectively. For glycated hemoglobin, the mean effect in the control and intervention groups was 3.93 and −5.13, respectively (p<0.001). Levels of glycated hemoglobin and other metabolic indicators, as well as most of the secondary outcomes, showed a significant difference in the experimental group compared to the control group. [1]
Trief et al. reported that the primary intervention goal was progressed glycemic control of the character with diabetes. Persons with diabetes participated alone; in the control couple (CC), the person with diabetes and his/her partner participated collectively. All arms received calls protecting comprehensive diabetes education. Control couple (CC) and intervention couple (IC) arms had 10 additional calls, the content was based totally on social learning idea, which had been comparable with maximum behavioral interventions (provision of expertise, selfmonitoring, goal-setting and behavioral contracting to promote lifestyle changes in activity, diet, blood glucose monitoring, and medicinal drug adherence), targeted on the effect of behavior on glycemic control. [17]
Gonzalez-Zacarias et al. reported that, the educational differences in glycemic degrees, and the factors contributing to the survival differences in older adults with diabetes. High school or more education was associated with better glycemic control and higher survival fees at observe-up whilst in comparison to those with lower schooling. The independent results of socioeconomic and psychosocial determinants of fitness on diabetes knowledge, self-care, and satisfaction of life. They confirmed that diabetes knowledge was related to college education and earnings of>$20,000. Also, higher diabetes results were substantially associated with higher SES, selfefficacy, and excellent life. [18]
He et al. reported that 42 randomized managed trials containing 13,017 participants have been included. The mean time of observe-up changed into 1.5 years. There was no heterogeneity amongst those included research. Mortality happened in 159 individuals (2.3%) within the diabetes self-control education group and 187 (3.1%) in the usual care group and diabetes selfmanagement education appreciably reduced the hazard of allmotive mortality in type 2 diabetes patients (pooled RR: 0.74, P=0.003; absolute RD: −0.8% to −0.3). each multidisciplinary team education and nurse-led education may want to notably reduce mortality risk in type 2 diabetes sufferers, and the pooled risk ratios have been 0.66 (P=0.02) and 0.64 (P=0.1), respectively. Subgroup analyses of studies with a longer length of follow-up (≥1.5 years) or large pattern size (≥300) also found a significant effect of diabetes self-control education in lowering mortality hazard amongst type, 2 diabetes. [3]
Zhao et al. reported that twenty studies with 5,802 participants met the inclusion criteria. The interventions in the studies were based on one or more theories which mostly belong to mid-range theories. The pooled main outcomes by random-effects model showed significant improvements in HbA1c, self-efficacy, and diabetes knowledge, but not in BMI. As for the quality of life, no conclusions can be drawn as the pooled outcome became the opposite with reduced heterogeneity after one study was excluded. [4]
Caro-Bautista et al. reported that, in total, 20 studies had been analyzed, representing a population of 12,018 persons with T2DM. For the primary outcome, HbA1c, the overall reduction acquired was −0.29%, reducing the effect in a long-time period follow-up. The quality of the evidence was low/very low because of the very severe risk of bias, inconsistency, and indirectness of results. Better consequences had been obtained for individually randomized trials versus cluster designs and in the ones, programmers wherein nurses led the interventions. The findings for other cardiovascular chance factors were inconsistent. [19]
Saleh et al. reported that, after the intervention, the mean score of knowledge (8.5 vs. 5.5) and attitudes (85.7 vs. 79.9) of the patients improved significantly (P=0.0001). About 67.7%, 85.2%, 82.8%, and 92.1% of the patients were monitored for blood glucose, doing exercises, taking foot care and smoking withdrawal whereas the rates were 8.3%, 69.2%, 25.8%, and 86.7%, respectively before the intervention; a significant difference was observed between the measures. [20] Our result came in disagreement with Abdulah et al. [21]
Abdulah et al. reported that the study showed that walking, taking vegetables, fruit, and bread were higher, and taking fullfat cheese and full-fat spread was lower among the experimental group significantly compared to the control arm. Besides, the experimental group had substantially higher albumin and lower urea, ALP-Phosphatase, and glucose levels in comparison with control patients. No substantial change was seen in HbA1C and no change in milk and fish products. [21]
Conclusion
To conclude, educational interventions in primary care addressing T2DM could be effective for metabolic control, but the low quality of the evidence and the lack of measurement of critical results generate uncertainty and highlight the need for high-quality trials.
Competing Interests
The authors declare that they have no competing interests. All the listed authors contributed significantly to the conception and design of study, acquisition, analysis, and interpretation of data and drafting of the manuscript, to justify authorship
REFERENCES
- Cortez DN, Macedo MML, Souza DAS, dos Santos JC, Afonso GS, Reis IA, et al. Evaluating the effectiveness of an empowerment program for self-care in type 2 diabetes: a cluster-randomized trial. BMC Public Health. 2017;17:41.
- Garcia-Molina L, Lewis-Mikhael AM, Riquelme-Gallego B, Cano-Ibanez N, Oliveras-Lopez MJ, Bueno-Cavanillas A. Improving type 2 diabetes mellitus glycaemic control through lifestyle modification implementing diet intervention: a systematic review and meta-analysis. Eur J Nutr. 2020;59:1313-1328.
- He X, Li J, Wang B, Yao Q, Li L, Song R, et al. Diabetes self-management education reduces risk of all-cause mortality in type 2 diabetes patients: a systematic review and meta-analysis. Springer; 2017.
- Zhao FF, Suhonen R, Koskinen S, Leino-Kilpi H. Theory-based self-management educational interventions on patients with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. J Adv Nurs. 2017;73:812-833.
- Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions. Bmj 2009;339.
- Khunti K, Gray LJ, Skinner T, Carey ME, Realf K, Dallosso H, et al. Effectiveness of a diabetes education and self-management programme (DESMOND) for people with newly diagnosed type 2 diabetes mellitus: three-year follow-up of a cluster randomized controlled trial in primary care. Bmj 2012;344:e2333.
- Adachi M, Yamaoka K, Watanabe M, Nishikawa M, Kobayashi I, Hida E, et al. Effects of lifestyle education program for type 2 diabetes patients in clinics: a cluster randomized controlled trial. BMC Public Health 2013;13:467.
- DePue JD, Dunsiger S, Seiden AD, Blume J, Rosen RK, Goldstein MG, et al. Nurse–community health worker team improves diabetes care in American Samoa: results of a randomized controlled trial. Diabetes Care. 2013;36:1947-1953.
- Thom DH, Ghorob A, Hessler D, De Vore D, Chen E, Bodenheimer TA. Impact of peer health coaching on glycemic control in low-income patients with diabetes: a randomized controlled trial. Ann Fam Med. 2013;11:137-144.
- Mash RJ, Rhode H, Zwarenstein M, Rollnick S, Lombard C, Steyn K, et al. Effectiveness of a group diabetes education program in under-served communities in South Africa: a pragmatic cluster randomized controlled trial. Diabetic Med. 2014;31:987-993.
- Grillo M de FF, Neumann CR, Scain SF, Rozeno RF, Beloli L, Perinetto T, et al. Diabetes education in primary care: a randomized clinical trial. Cadernos de Saude Publica 2016;32:e00097115.
- Jutterström L, Hörnsten \AAsa, Sandström H, Stenlund H, Isaksson U. Nurse-led patient-centered self-management support improves HbA1c in patients with type 2 diabetes—a randomized study. Patient Educ Couns. 2016;99:1821-1829.
- Islam NS, Wyatt LC, Taher MD, Riley L, Tandon SD, Tanner M, et al. A culturally tailored community health worker intervention leads to improvement in patient-centered outcomes for immigrant patients with type 2 diabetes. Clin Diabetes. 2018;36:100-111.
- Moreno EG, Mateo-Abad M, de Retana García LO, Vrotsou K, del Campo Pena E, Perez ÁS, et al. Efficacy of a self-management education programme on patients with type 2 diabetes in primary care: A randomised controlled trial. Prim Care Diabetes. 2019;13:122-133.
- Dehghan Nayeri N, Samadi N, Larijani B, Sayadi L. Effect of nurse-led care on quality of care and level of HbA1C in patients with diabetic foot ulcer: A randomized clinical trial. Wound Repair Regen. 2020;28:338-346.
- Ali ZT, Al Saadi MT, Al Saadi NT. Incidence of stroke with uncontrolled DM: effect of pharmaceutical care intervention to DM type-2 patients in Iraqi hospitals. Ann Trop Med Public Health. 2019;22:221-231.
- Trief PM, Fisher L, Sandberg J, Hessler DM, Cibula DA, Weinstock RS. Two for one? Effects of a couples intervention on partners of persons with type 2 diabetes: a randomized controlled trial. Diabetic Med. 2019;36:473-481.
- Gonzalez-Zacarias AA, Mavarez-Martinez A, Arias-Morales CE, Stoicea N, Rogers B. Impact of demographic, socioeconomic, and psychological factors on glycemic self-management in adults with type 2 diabetes mellitus. Front Public Health. 2016;4:195.
- Caro-Bautista J, Kaknani-Uttumchandani S, García-Mayor S, Villa-Estrada F, Morilla-Herrera JC, León-Campos Á, et al. Impact of self-care programmes in type 2 diabetes mellitus population in primary health care: Systematic review and meta-analysis. J Clin Nurs. 2020;29:1457-1476.
- Saleh F, Afnan F, Ara F, Mumu SJ, Khan AK. Diabetes education, knowledge improvement, attitudes and self-care activities among patients with Type 2 Diabetes in Bangladesh. Jundishapur J Health Sci. 2017;9.
- Abdulah DM, Hassan AB, Saadi FS, Mohammed AH. Impacts of self-management education on glycaemic control in patients with type 2 diabetes mellitus. Diabetes Metab Syndr. 2018;12:969-975.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.