Effect of Non‑Surgical Periodontal Therapy on the Concentration of Volatile Sulfur Compound in Mouth Air of a Group of Nigerian Young Adults
- *Corresponding Author:
- Dr. Adebola O Ehizele
Department of Periodontics, University of Benin Teaching Hospital, P.M.B. 1111 Ugbowo, Benin City, Edo State, Nigeria.
E-mail: deblosco@yahoo.co.uk
Citation: Ehizele AO, Akhionbare O. Effect of non-surgical periodontal therapy on the concentration of volatile sulfur compound in mouth air of a group of Nigerian young adults. Ann Med Health Sci Res 2013;3:433-7.
Abstract
Background: The major goal of non‑surgical periodontal therapy is to reduce or eliminate the subgingival pathogenic microbial flora that is known to be associated with volatile sulfur compounds (VSC). Aim: The aim of this study was, therefore, to determine the effect of non‑surgical periodontal therapy on the concentration of VSC in mouth air of young adults. Subjects and Methods: Four hundred subjects, grouped into two based on the absence or presence of periodontal diseases, were involved in this study. Basic periodontal examination was used for the grouping. The measurement of the concentration of the VSC in the mouth air of the subjects was done objectively, using the Halimeter, before and after the therapy, and at recall visits 2 weeks and 6 weeks after therapy. Chi‑square and Paired t‑test were used to find statistical significance. Results: The results revealed that at baseline, 78.7% (48/61) of the subjects who had VSC concentration more than 250 parts per billion (ppb) were from the group with periodontal disease. Immediately after non‑surgical periodontal therapy, only 8.5% (17/200) of the subjects with periodontal disease had VSC concentration of more than 250 ppb while all the subjects with no periodontal disease had VSC concentration less than 181 ppb. The same pattern of reduction in the concentration of the VSC and improvement in oral hygiene was also obtained 2 weeks and 6 weeks after therapy. Conclusion: It can be concluded that non‑surgical periodontal therapy brought about reduction in the concentration of volatile sulfur compounds in mouth air of young adults.
Keywords
Africa, Concentration, Mouth, Non-surgical periodontal therapy, Volatile sulfur compound
Introduction
Non-surgical periodontal therapy refers to the conventional and conservative way of removing supra and subgingival bacterial plaque and calculus. The goal of this therapy is to establish and maintain healthy periodontal tissues by removing irritants from the surface and root of the tooth that promote plaque retention, through mechanical means.[1] Dental health education and instruction on plaque control is an integral part of this therapy.[2]
It remains an essential component of any successful periodontal treatment,[2,3] and it is considered the “gold standard” for the non-surgical management of periodontitis in most quarters.[4] Evaluation for post-scaling and root planing healing is usually done at 4 to 6 weeks following treatment when most of the healing would have taken place.[5] Repair and collagen maturation may continue for an additional 9 months.[1,6] Reduction of pockets depth and improvement in the level of clinical attachment are noticeable after scaling and root planing.[7]
Since the major goal of non-surgical periodontal therapy is to reduce or eliminate, to the extent possible, the subgingival pathogenic microbial flora that is known to be associated with volatile sulfur compounds (VSC), the therapy, therefore, may result in a significant reduction of the concentration of VSC released during the activities of these microbes.
Previous studies have shown that non-surgical periodontal therapy can reduce the sulfide level in the gingival sulcus[8,9] and that a thorough oral hygiene training program can reduce the oral level of VSC.[10] There is, however, a paucity in this area of research in our environment. If the relationship between the non-surgical periodontal therapy and concentration of VSC is established, measurement of the concentration of VSC may then be a useful parameter in the estimation of patients’ response to non-surgical periodontal therapies and determination of improvement or progression of periodontal diseases. Therefore, the aim of this study was to determine the relationship between non-surgical periodontal therapy and the concentration of VSC in mouth air of young adults.
Subjects and Methods
Four hundred subjects between the ages of 20 and 40 were selected from the Periodontology Clinic at the University of Benin Teaching Hospital, Benin City. An informed consent was duly obtained, and the study was approved by the Ethics and Research Committee of the University of Benin Teaching Hospital.
The subjects were grouped into two using the basic periodontal examination (BPE).[11,12] Two hundred subjects made up the group with no periodontal disease (BPE score 0), and the other 200 subjects made up the group with periodontal disease (BPE score 1-4). Smokers, subjects with any underlying systemic diseases, and subjects using any orthodontic or prosthetic appliance, that may worsen oral hygiene, were excluded.
The measurement of the concentration of the VSC in the mouth air of the subjects was done objectively using the Halimeter [Figure 1].[13] Subjects abstained from eating strongly spiced foods at least 48 hours before the assessment, avoided using scented cosmetics for 24 hours before the assessment, abstained from ingesting any food or drink 12 hours before assessment, omitted their usual oral hygiene practices 12 hours before assessment, and abstained from using oral rinse and breath fresheners. The examiner also refrained from drinking coffee, tea or juice, smoking, and using scented cosmetics 12 hours before the assessment.[13-15]
The Halimeter reading, based on the method used in similar studies,[14,15] was categorized into 3 as follows: Normal = 0-180 parts per billion (ppb), Weak = 181-250 ppb, Strong = > 250 ppb. Baseline measurements were taken in the morning before tooth brushing.
The subjects were then treated based on their BPE scores. Subjects who had a BPE score of 0 did not have any periodontal treatment. Tooth brushing was done, and oral hygiene instruction given. Subjects who scored 1-4 were given oral hygiene, and non-surgical periodontal therapy was done as applicable (i.e., scaling and polishing with or without subgingival curettage). A second measurement of VSC concentration was done after tooth brushing or non-surgical periodontal therapy. The level of oral hygiene and the concentration of the VSC of subjects were repeated 2 weeks and 6 weeks after the initial measurements.
The data was analyzed using the Statistical Package for Social Sciences version 15.0 for frequency distributions and cross-tabulation. Chi-square test was done to test statistical significance. Paired t-test was used to find statistical significance in the difference between the concentration of the volatile sulfur compounds in the two groups before and after non-surgical periodontal therapy. P values less than 0.05 was considered statistically significant.
Results
At baseline, the mean concentration of VSC in the group with no periodontal disease was 91.5 (5.9) ppb while it was 228.5 (16.7) ppb in the group with periodontal disease [Table 1]. Two hundred and fifty subjects had a concentration of VSC less than 181 ppb, 63.2% (158/250) of which had no periodontal disease, and 36.8% (92/250) had varying degree of periodontal disease. Eighty-nine subjects had a concentration of VSC between 181 and 250 ppb, 32.6% (29/89) of which had no periodontal disease, and 67.4% (60/89) had varying degree of periodontal disease. Sixty one subjects had a concentration of VSC greater than 250 ppb, 21.3% (13/61) of which had no periodontal disease, and 78.7% (48/61) had varying degree of periodontal disease (P = 0.01) [Table 2].
| Stages | Disease present | Disease absent | ||
|---|---|---|---|---|
| Mean VSC(SEM) (ppb) | P value | Mean VSC(SEM) (ppb) | P value | |
| 1a | 228.5 (16.7) | 0.001 | 91.5 (5.9) | 0.001 |
| 1b | 106.2 (9.5) | 46.6 (3.2) | ||
| 2 | 6.8 (1.0) | 4.7 (0.4) | ||
| 3 | 3.4 (0.5) | 3.1 (0.3) | ||
Table 1: Comparison of means of the VSC concentration of the subjects at the stages of the study
| Disease present n (%) | Disease absent n (%) | Total n (%) | χ² | P value | |
|---|---|---|---|---|---|
| VS Cconcentration (ppb) | |||||
| <181 | 92 (36.8) | 158 (63.2) | 250 (100.0) | 48.30 | 0.001 |
| 181-250 | 60 (67.4) | 29 (32.6) | 89 (100.0) | ||
| >250 | 48 (78.7) | 13 (21.3) | 61 (100.0) | ||
| Total | 200 (50.0) | 200 (50.0) | 400 (100.0) | ||
Table 2: Baseline VSC concentration in mouth air of subjects
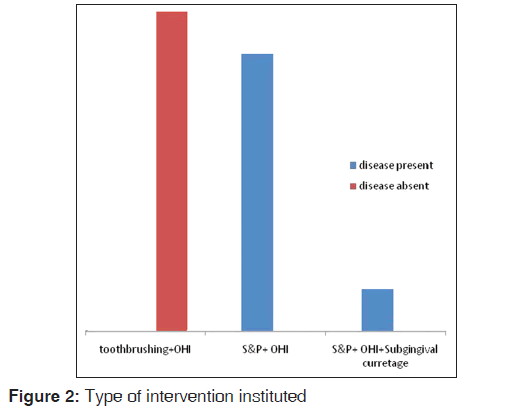
Immediately after instituting the treatment applicable [Figure 2], most of the subjects (364/400) had a concentration of VSC less than 181 ppb. Nineteen subjects with periodontal disease had concentration of VSC between 181 and 250 ppb, and 17 subjects with periodontal disease had concentration of VSC greater than 250 ppb (P = 0.01) [Table 3]. The mean concentration of VSC concentration was reduced to 46.6 (3.2) ppb and 106.2 (9.5) ppb in the group with no periodontal disease and the group with periodontal disease, respectively [Table 1].
| VS Cconcentration(ppb) | Disease present disease absent total | ||||
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | χ² | P value | |
| <181 | 164(82.0) | 200(100.0) | 364(91.0) | 39.56 | 0.001 |
| 181-250 | 19(9.5) | 0(0.0) | 19(4.8) | ||
| >250 | 17(8.5) | 0(0.0) | 17(4.2) | ||
| Total | 200 (100.0) | 200(100.0) | 400(100.0) | ||
Table 3: VSC concentration in mouth air of subjects measured immediately after intervention
Two weeks after the therapy, the mean concentration of VSC concentration was reduced to 4.7 (0.4) ppb and 6.8 (1.0) ppb in the group with no periodontal disease and the group with periodontal disease, respectively. Six weeks after the therapy, the mean concentration of VSC concentration was reduced to 3.1 (0.3) ppb and 3.4 (0.5) ppb in the group with no periodontal disease and the group with periodontal disease, respectively [Table 1]. The same pattern of Halimeter readings was recorded at 2 weeks and 6 weeks recall visits. All the subjects in the two groups had concentration of VSC less than 181 ppb [Figure 3].
Discussion
In this study, the non-surgical periodontal therapy required by majority of the subject with periodontal disease was scaling and polishing and oral hygiene instruction. Only a few required more complex non-surgical periodontal treatment. This result is similar to what was previously reported.[16-18] This may be because scaling and polishing effectively removes plaque, the primary etiological factor of periodontal diseases as well as calculus and stains, which are the commonly seen plaque-retentive factors.
Generally, the subjects with periodontal disease in this study had the tendency of having a higher concentration of VSC. The attempt to control plaque by an individual with periodontal disease may be impaired by pain, mobility, or drifting of the affected teeth. This worsens the oral hygiene and ultimately worsens the periodontal condition. The putrefaction of desquamated epithelial cells and leukocytes occasioned by periodontal destruction may also lead to increase in the concentration of VSC.[19]
Non-surgical periodontal therapy had an effect on the concentration of volatile sulfur compounds in mouth air of the subjects in this study. A paired sample t-test was conducted to compare the mean of the concentration of VSC before non-surgical periodontal treatment and after non-surgical periodontal treatment. The result specifically suggests that after non-surgical periodontal therapy is done, the concentration of VSC decreases (P = 0.001). This may be due to the fact the debridement as a result of tooth brushing and non-surgical periodontal therapy reduces plaque accumulation and maintains a better intra-oral bacterial environment.[3] Some sources of VSC such as bacteria plaque, proteinaceous food debris, and calculus are removed by non-surgical periodontal therapy.[20] This supports a previous study that reported that the level of oral malodor significantly reduced after treating gingival inflammation with scaling and oral hygiene instruction.[21]
It was also observed at the recall visits 2 weeks and 6 weeks after treatment that subjects had lower mean of concentration of VSC. This may imply that once the possible oral causes are removed, the concentration of VSC will decrease. It may also imply that subjects were compliant with the oral hygiene instructions emphasized after the treatment. The result of this study supports previous studies that showed statistically significant improvement in VSC levels after non-surgical periodontal therapy.[10,22] Although it was reported that the expected improvement in oral hygiene after oral hygiene instruction may be overestimated,[23] another study reported highly significant improvements in oral health after dental education and oral hygiene instruction.[24]
Most of the subjects in this study had mild forms of periodontal diseases. Future similar studies should be done in the elderly as more severe forms of periodontal diseases are seen among the elderly.[25] It will be interesting to see if the level of VSC increases with the severity of periodontal disease and if non-surgical periodontal therapy will still lower the level of VSC in severe cases of periodontal disease.
Conclusion
In this study, non-surgical periodontal therapy brought about reduction in the concentration of volatile sulfur compounds in mouth air of young adults, and this reduction in the level of volatile sulfur compound was maintained up to 6 weeks after the non-surgical therapy. It can, therefore, be concluded that a relationship exists between non-surgical periodontal therapy and the concentration of VSC in mouth air.
References
- Greenstein G. Nonsurgical periodontal therapy in 2000: A literature review. J Am Dent Assoc 2000;13:1580-92.
- Drisko CH. Nonsurgical periodontal therapy. Periodontol 2000 2001;25:77-88.
- Cobb CM. Clinical significant of non-surgical periodontal therapy: An evidence based perspective of scaling and root planing. J Clin Periodontol 2002;29:6-16.
- Ryan ME. Nonsurgical approaches for treatment of periodontal diseases. Dent Clin North Am 2005;49:611-36.
- American Academy of Periodontology. Non-surgical periodontal treatment: Consensus statement. In: Proceedings of the world workshop in clinical periodontics. Chicago. American Academy of Periodontology; 1989. p. II-13–II-7.
- Badersten A, Nilveus R, Egelberg J. Effect of nonsurgical periodontal therapy. I. Moderately advanced periodontitis. J Clin Periodontol 1981;8:57-72.
- Hung HC, Douglass CW. Meta-analysis of the effect of scaling and root planing, surgical treatment and antibiotic therapies on periodontal probing depth and attachment loss. J Clin Periodontol 2002;29;975-86.
- Morita M, Wang HL. Effect of initial periodontal therapy on sulcular/tongue sulfide level. A pilot study. J Clin Periodontol 2002;29:844-7.
- Nogueira-Filho GR, Peruzzo D, Sallum AW. Relationship between the formation of VSC and the severity of the periodontal disease: A pilot study. J Breath Res 2008;2:017005-10.
- Seemann R, Passek G, Bizhang M, Zimmer S. Reduction of oral levels of volatile sulfur compounds (VSC) by professional toothcleaning and oral hygiene instruction in non-halitosis patients. Oral Health Prev Dent 2004;2:397-401.
- Tugnait A, Clerehugh V, Hirschmann PN. Use of the basic periodontal examination and radiographs in the assessment of periodontal diseases in general dental practice. J Dent 2004;32:17-25.
- Council of the British Society of Periodontology. Guidance on interpretation of BPE scores. Available from: http://www. bsperio.org. [Last accessed on 2011 Dec 12].
- Interscan Corporation Halimeter Instruction Manual. Available from: http://www.halimeter.com. [Last accessed on 2009 Jul 24].
- Satoh S, Ohmori M, Murayama K, Nakamura T, Saitoh M, Imai R, et al. A study of measurement of oral malodour with a portable sulfide monitor Halimeter®. J Jpn Soc Periodontol 1999;41:195-200.
- Baharvand M, Maleki Z, Mohammadi S, Alavi K, Moghaddam EJ. Assessment of oral malodour: A comparison of the organoleptic method with sulfide monitoring. J Contemp Dent Pract 2008;9:76-83.
- Ogunbodede EO, Adamolekun B, Akintomide AO. Oral health and dental treatment needs in Nigerian patients with epilepsy. Epilepsia 1998;39:590-4.
- Akhionbare O, Ojehanon PI, Ufomata DO, Jeboda SO. Periodontal treatment needs of urban and rural populations in Edo State, Nigeria. Niger Dent J 2007;15:13-7.
- Azodo CC, Ehizele AO, Umoh A, Ojehanon PI, Akhionbare O, Okechukwu R, et al. Perceived oral health status and treatment needs of dental auxiliaries. Libyan J Med 2010;5.
- Ratcliff PA, Johnson PW. The relationship between oral malodor, gingivitis and periodontitis. A review. J Periodontol 1999;70:485-9.
- Yaegaki K, Suetaka T. Periodontal disease and precursors of oral malodourous components. J Dent Health 1989;39:733-41.
- Kara C, Tezel A, Orbak R. Effect of oral hygiene instruction and scaling on oral malodour in a population of Turkish children with gingival inflammation. Int J Paediatr Dent 2006;16:399-404.
- Roldán S, Herrera D, O’Connor A, González I, Sanz M. A combined therapeutic approach to manage oral halitosis: A 3-month prospective case series. J Periodontol 2005;76:1025-33.
- Weinstein P, Milgrom P, Melnick S, Beach B, Spadafora A. How effective is oral hygiene instruction? Results after 6 and 24 weeks. J Public Health Dent 1989;49:32-8.
- Shenoy RP, Sequeira PS. Effectiveness of a school dental education program in improving oral health knowledge and oral hygiene practices and status of 12- to 13-year-old school children. Indian J Dent Res 2010;21:253-9.
- Savage KO. A preliminary study of the periodontal status and treatment needs of elderly Nigerian subjects. Afr Dent J 1992;6:23-9.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.