Effect of Phacoemulsification Surgery on Central Maclar Thickness
2 Department of Opthalmology, Custom Eyecare, Islamabad, Pakistan
Department of Optometry, Women University, Multan, Pakistan
3 University of Lahore, Lahore, Pakistan
, DOI: 10.54608.annalsmedical.2021.6
Citation: Ali Qasim MS, et al. Effect of Phacoemulsification Surgery on Central Maclar Thickness. Ann Med Health Sci Res. 2021;11:1536- 1539.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objective: The objective of this study is to demonstrate the sustainability of changes in Central Macular thickness associated with Phacoemulsification surgery. Materials & Methods: Cohort study with 120 patient’s eyes was conducted from March 2020 to August 2020 at Riphah International University Lahore. Sampling technique was non probability convenient sampling technique. Inclusion criteria include all patients willing to undergone phacoemulsification with intraocular lens implant (phaco) surgery and having cataract with controlled diabetes and hypertension. Exclusion criteria include all patients who didn’t agree to undergone phaco surgery. Patients with any other ocular pathology were excluded from the study. Refractive status objectively assessed by Canon Autorefractor and Heine retinoscope. Vision was assessed at six (06) meters of distance using Snellen chart and recorded using Snellen notation. Average reading of both methods was taken. The phacoemulsification was done using “OertliCataRhex 3” and foldable lens was implanted during the surgery. For the measurement of the macular thickness Zeiss Cirrus HD-OCT 500 model was used. All data entered and analyzed by SPSS 20 (Statistical Package for Social Sciences). Normality of quantitative data was checked by Shapiro Wilk test. Wilcoxon sign test was used for non-parametric data. P value <0.05 was taken as significant. Results: This study include 120 patient’s eyes that undergone successful phacoemulsification surgery. Macular thickness before the surgery was assessed and recorded on proforma. Mean macular thickness before surgery was 210 μm. After the surgery the macular thickness was recorded after 01 week and 04 weeks and the mean values were 243 μm and 207 μm respectively. The best corrected visual acuity after the surgery was 6/6 in 21%, 6/9 in 47% and 6/12 in 31% patients. There is significant difference between the macular thickness of before and after the phacosurgery (p=0.00). The macular thickness was decreases with the time and settled after 04 weeks of surgery. Conclusion: There is significant difference between the macular thickness before and after phaco surgery (p=0.000). The macular thickness is slightly raised after the surgery and observed to lower down after 04 week of surgery.
Keywords
Phaco; Phacoemulsification; Cataract; OCT; Zeiss; Macula; Macular thickness
Introduction
The objective of this study is to demonstrate the sustainability of changes in Central Macular thickness associated with Phacoemulsification surgery. This study gave the comparison of macular thickness before and after phacoemulsification. [1]
Phacoemulsification (phaco) has become the preferred form of cataract removal. Advantages of phacoemulsification are that only a small incision into the cornea or sclera of an eye is needed to remove the opaque lens. Moreover, the breakdown of the cataractous lens can be done very swiftly. After the cataract is removed, an IOL is inserted to replace the original lens. The phaco technique uses a hand-held microsurgical tool which is known as phacoemulsifier. [2] This phacoemulsifier consist of a handpiece and a minor width needle with a tip to be incorporated into the tiny incision of the eye. The needle and hence the tip are pulsated by an ultrasonic supplier. It breaks the cataract into small fragments which are sucked out through the same tip in a controlled manner. The tip is henceconstructed for emulsifying, fragmenting and also comprises a central hollow bore or lumen for the suction or aspiration of the fragments. [3]
It was seen that during phaco surgery small amount of section/ emulsifier effect is seen on retina especially Macula. Eventually unsuccessful cataract surgical procedure causes minimal intraoperative trauma, which results in the thickening of macula. [4]
Cataract is defined as the clouding in the eyes or loss of transparency of the lensresulting in the breakdown of tissue and protein plodding. The causes of cataract development in the eyes are numerous including hypertension, diabetes, systematic medication like cortisone, trauma and other pathologies. [5]
For posterior segment evaluation, Optical Coherence Tomography (OCT) is used to analyze the thickening of retina especially macula. OCT is a method used for macular thickness measurement and quantitative assessment of the retina. [6] OCT is a reproducible, non-invasive and non-contact system of imaging providing higher resolution cross sectional pictures of the posterior section. Imaging of the anterior segment has also been increasingly adopted. OCT utilizes near infrared light rays for interferometry for the formation of image of retina layer by using Michelson interferometry principle. The basic principle of OCT (Michelson Interferometry) is to measure the time-offlight of light echoes from tissue, which is done by creating an interference pattern between light transmitting in one arm and light transmitting in the reference arm of a Michelson interferometer. [7]
In recent years it has become increasingly common to use OCT) to study the macular region. There are a lot of techniques to assess macula and measure macular thickness. But OCT is one of the best techniques, which is easy to use, non-invasive, give qualitative & quantitative data and easily reproducible. [8-10] This technique has the advantage of being simple to perform, non-invasive, and extremely sensitive, as it can provide measurements of the macular region with a resolution of 8 μm- 10 μm (micron meter). Moreover, OCT has been used to study the macular region after uncomplicated cataract surgery. [11]
The Macula is a rounded area of retina at the posterior pole of eye, lying within the temporal vascular arcades. It measures between 5 mm and 6 mm in diameter, and sub serves the central 15°-20° of the visual field. Histologically, it shows more than 1 layer of ganglionic cells, in contrast to the single ganglion cell layer of the peripheral retina. Lutein, xanthin and zeaxanthin which are yellow xanthophyll carotenoid pigments found in the inner layers of macula in much higher concentration than the peripheral retina. Hence the full name Macula Lutea. [12]
Macular thickness and the macular region change correlate with the changes of visual function. In macular edema the thickness of retinal layers is increased retinal thickness and often leads to vision loss. Macular edema is an intra-retinal fluid accumulation in the central retina. The blood-retinal barrier is responsible for the integrity of the macula. Tight junctions between cells of intra-retinal capillaries and pigmented epithelium cells prevent the progress of fluidaccumulation within the macula. Macular edema after cataract surgery occurs in a clinical and sub-clinical form. [13-16]
Materials and Methods
Cohort study with 120 patient’s eyes was conducted from March 2020 to August 2020 at Riphah International University Lahore. Sampling technique was non probability convenient sampling technique. Inclusion criteria include all patients willing to undergone phacoemulsification with intraocular lens implant (phaco) surgery and having cataract with controlled diabetes and hypertension. Exclusion criteria include all patients who didn’t agree to undergone phaco surgery. Patients with any other ocular pathology were excluded from the study. Patients with uncontrolled hypertension and diabetics were unrolled in the study. Refractive status objectively assessed by Canon Autorefractor and Heine retinoscope. Vision was assessed at six (06) meters of distance using Snellen chart and recorded using Snellen notation. Average reading of both methods was taken. The phacoemulsification was done using “OertliCataRhex 3” and foldable lens was implanted during the surgery. For the measurement of the macular thickness Zeiss Cirrus HDOCT 500 model was used. Approval from the ethical review committee of Riphah International University Lahore campus. All data were entered and analyzed by SPSS 20.0 (Statistical Package for Social Sciences). Normality of quantitative data was checked by Shapiro Wilk test. Wilcoxon sign test was used for non-parametric data. P value<0.05 was taken as significant.
Results
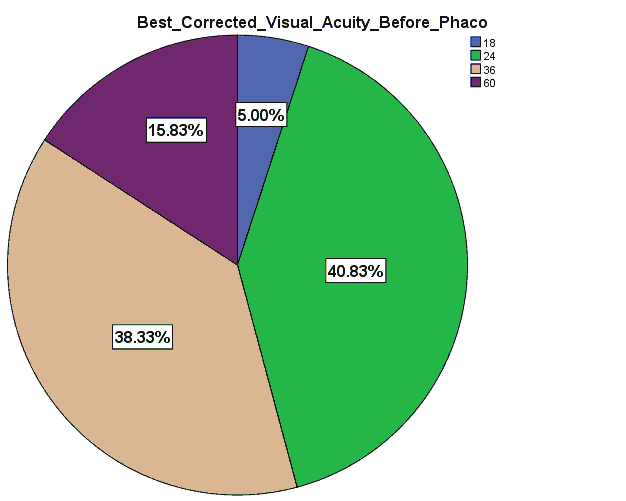
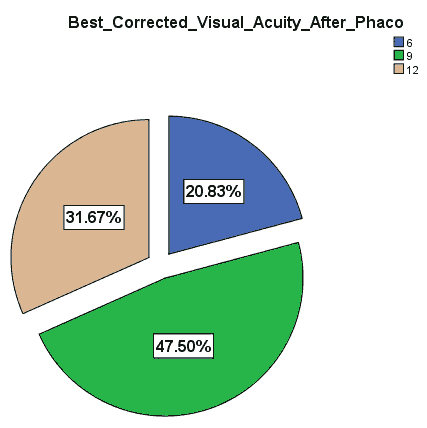
120 patient’s eyes that undergone successful phacoemulsification surgery was enrolled in this study. Macular thickness before and after the surgery was assessed and recorded on proforma. Mean macular thickness before surgery was 210 μm. After the surgery the macular thickness was recorded after 01 week and 04 weeks and the mean values were 243 μm and 207 μm respectively. The clinical characteristics are listed in Table 1 and Table 2. The frequency data of best corrected visual acuity before the phaco surgery showed that the vision of patients was 6/18 in 5%, 6/24 in 40.83%, 6/36 in 38.33% and 6/60 in 15.83% of patients respectively [Figure 1]. The frequency data of best corrected visual acuity after the phaco surgery showed that the vision of patients was 6/6 in 21%, 6/9 in 47% and 6/12 in 31% patients [Figure 2].
| Descriptive statistics | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Range | Minimum | Maximum | Mean | Std. Deviation | Variance | Skewness | Kurtosis | ||||
| Statistic | Statistic | Statistic | Statistic | Statistic | Std. Error | Statistic | Statistic | Statistic | Std. Error | Statistic | Std. Error | |
| Age | 120 | 15 | 40 | 55 | 46.94 | 0.26 | 2.8 | 7.8 | 0.07 | 0.22 | 0.8 | 0.4 |
| Macular Thickness Before Phaco | 120 | 39 | 188 | 227 | 210.58 | 0.52 | 5.7 | 32.8 | -1.41 | 0.22 | 4.2 | 0.4 |
| Macular Thickness After Phacoat 01_Week | 120 | 50 | 220 | 270 | 243.99 | 0.83 | 9.1 | 83.5 | 0.3 | 0.22 | -0.1 | 0.4 |
| Macular Thickness After Phacoat 04_Week | 120 | 39 | 188 | 227 | 207.66 | 0.65 | 7.1 | 50.9 | -0.61 | 0.22 | 1.3 | 0.4 |
*Mean macular thickness before the phaco surgery was 210 with std. error of mean 0.52. *Mean macular thickness after phaco surgery at 01 week was 243.99 with std. error of mean 0.83. *Mean macular thickness after phaco surgery at 04 week was 207.66 with std. error of mean 0.65.
Table 1: Descriptive statics of macular thickness before and after the phaco surgery.
| Kolmogorov-Smirnova | Shapiro-Wilk | |||||
|---|---|---|---|---|---|---|
| Statistic | df | Sig. | Statistic | df | Sig. | |
| Age | 0.142 | 120 | 0 | 0.965 | 120 | 0.003 |
| Macular Thickness Before Phaco | 0.158 | 120 | 0 | 0.878 | 120 | 0 |
| Macular Thickness After Phacoat 01_Week | 0.152 | 120 | 0 | 0.951 | 120 | 0 |
| Macular Thickness After Phacoat 04_Week | 0.222 | 120 | 0 | 0.91 | 120 | 0 |
Table 2: Test of normality was applied and the data was non parametric.
Descriptive statistics of macular thickness before and after the phaco surgery was presented in Table 1. Mean macular thickness before the phaco surgery was 210 with std. error of mean 0.52. Mean macular thickness after phaco surgery at 01 week was 243.99 with std. error of mean 0.83. Mean macular thickness after phaco surgery at 04 week was 207.66 with std. error of mean 0.65. There is significant difference between the macular thickness of before and after the phaco surgery (p=0.00). The macular thickness was decreases with the time and settled after 04 weeks of surgery [Table 3].
| Null hypothesis | Test | Sig. | Decision |
|---|---|---|---|
| The median of difference between macular thickness before phaco and macular thickness after phaco | Related sample Wilcoxon-Signed Rank Test | 0 | Reject the Null Hypothesis |
Discussion
In this study recent include 120 patient’s eyes that undergone successful phacoemulsification surgery. Macular thickness before the surgery was assessed and recorded on proforma. Mean macular thickness before surgery was 210 μm. After the surgery the macular thickness was recorded after 01 week and 04 weeks and the mean values were 243 μm and 207 μm respectively. The best corrected visual acuity after the surgery was 6/6 in 21%, 6/9 in 47% and 6/12 in 31% patients. There is significant difference between the macular thickness of before and after the phaco surgery (p=0.00). The macular thickness was decreases with the time and settled after 04 weeks of surgery.
In this study the range of age of patients that undergone phacoemulsification surgery was between 40 years-55 years. The mean macular thickness before the surgery was 210.58 μm ± 0.52 μm the mean macular thickness after the surgery at first week was 243.99 μm ± 0.83 μm. The mean macular thickness before the surgery at 4th week was 207.66 μm ± 0.65 μm. The maximum macular thickness that observed at 1st week of surgery was 270 μm. The minimum macular thickness that observed at 1st week of surgery was 220 μm. The minimum and maximum macular thickness that observed at 4th week of surgery was 188 μm and 227 μm respectively. A study was conducted by Irfanperente et al. showed that the mean central macular thickness was before surgery 202.4 μm ± 25.9 μm and after the surgery 200.4 μm ± 26.1 μm. The macular thickness at first week of surgery (p=0.29), 208.4 μm ± 27.6 μm and at 4th week of surgery 213.5 μm ± 29.4 μm (p<0.001). The results of this study showed the same statistics. [17-20]
A lot of studies, which showed the correlation between the progression of macular thickness and cataract surgery was done and one from it which is conducted by the Brahm et al. showed that The mean macular thickness before, phaco at postoperative week 1, and at post-operative week 4 was 257.03 μm, 262.82 μm, and 265.15 μm respectively. This study results also support these statistics. [21-23]
Another study which was conducted by the Decroos showed that the pre and post-operative macular thickness was statically significant (p=0.0001). This study also showed the same results. [24,25]
Conclusion
There is significant difference between the macular thickness before and after phaco surgery (p=0.000). The macular thickness is slightly raised after the surgery and observed to lower down after 04 week of surgery.
Recommendations
The possible onset of macular alterations after phaco surgery must be taken into account as a potential later complication, because it can lead to a permanent loss of visual acuity. Longer follow-up of patients is required for the macular consequences, and different treatment protocols should be studied in a randomized controlled fashion. The results suggest that longterm follow-up of more than 4-week is needed to see whether CMT changes return to preoperative levels.
REFERENCES
- DeCroos FC, Afshari NA. Perioperative antibiotics and anti-inflammatory agents in cataract surgery. Curr Opin Ophthalmol. 2018;19:22-26.
- Panchapakesan J, Rochtchina E, Mitchell P. Five-year change in visual acuity following cataract surgery in an older community: The blue mountains eye study. Eye. 2014;18:278–282.
- Linebarger EJ, Hardten DR, Shah GK, Lindstrom RL. Phacoemulsification and modern cataract surgery. Surv Ophthalmol. 2019;44:123–147.
- Brien TP. Emerging guidelines for use of NSAID therapy to optimize cataract surgery patient care. Curr Med Res Opin. 2015;21:1131–37.
- Nelson ML, Martidis A. Managing cystoid macular edema after cataract surgery. Curr Opin Ophthalmol. 2013;14:39–43.
- GASS JD. Cystoid macular edema and papilledema following cataract extraction. JAMA Ophthalmol. 2016;76:646-650.
- Ursell PG, Spalton DJ, Whitcup SM, Nussenblatt RB. Cystoid macular edema after phacoemulsification: Relationship to blood-aqueous barrier damage and visual acuity. J Cataract Refract Surg. 2019;25:1492–1497.
- Flach AJ. The incidence, pathogenesis and treatment of cystoids macular edema following cataract surgery. Trans Am Ophthalmol Soc. 2018;96:557–634.
- Rho DS. Treatment of acute pseudophakic cystoid macular edema: Diclofenac versus ketorolac. J Cataract Refract Surg. 2013;29:2378–2384.
- Kim SJ, Equi R, Bressler NM. Analysis of macular edema after cataract surgery in patients with diabetes using optical coherence tomography. Ophthalmol. 2017;114:881–889.
- Dowler JGF, Sehmi KS, Hykin PG, Hamilton AMP. The natural history of macular edema after cataract surgery in diabetes. Ophthalmol. 2014;106:663–668.
- Lara-Smalling A, Egilmez CT. Diabetes and cataract surgery: Preoperative risk factors and positive nursing interventions. Insight (American Society of Ophthalmic Registered Nurses) 2014;39:18–20.
- Biro Z, Balla Z, Kovacs B. Change of foveal and perifoveal thickness measured by OCT after phacoemulsification and IOL implantation. Eye. 2018;22:8–12.
- Beebe DC, Shui YB, Siegfried CJ, Holekamp NM, Bai F. Preserve the (intraocular) environment: The importance of maintaining normal oxygen gradients in the eye. Jpn J Ophthalmol. 2014;58:225–231.
- Chu CJ, Johnston RL, Buscombe C, Sallam AB, Mohamed Q, Yang YC. Risk factors and incidence of macular edema after cataract surgery. A database Study of 81984 eyes. Ophthalmol. 2015;45:34-40.
- Liu J, Jones RE, Zhao J, Zhang J, Zhang F. Influence of uncomplicated phacoemulsification on central macular thickness in diabetic patients: A meta-analysis. PLoS ONE. 2015;10:90-95.
- Chung J, Kim MY, Kim HS, Yoo JS, Lee YC. Effect of cataract surgery on the progression of diabetic retinopathy. J Cataract Refract Surg. 2012;28:626–630.
- Henricsson M, Heijl A, Janzon L. Diabetic retinopathy before and after cataract surgery. Br J Ophthalmol. 2016;80:789–793.
- Kusbeci T, Eryigit L, Yavas G, Inan UU. Evaluation of cystoid macular edema using optical coherence tomography and fundus fluorescein angiography after uncomplicated phacoemulsification surgery. Curr Eye Res. 2012;37:327–333.
- Romero-Aroca P. Targeting the pathophysiology of diabetic macular edema. Diabetes Care. 2010;33:2484–2485.
- Chae JB, Joe SG, Yang SJ, Lee JY, Sung KR, Kim JY, et al. Effect of combined cataract surgery and ranibizumab injection in postoperative macular edema in non-proliferative diabetic retinopathy. Retina. 2014;34:149–156.
- Sahin M, Cingü AK, Gözüm N. Evaluation of cystoid macular edema using optical coherence tomography and fundus autofluorescence after uncomplicated phacoemulsification surgery. J Ophthalmol. 2013;13:37-45.
- Hartnett ME, Tinkham N, Paynter L, Geisen P, Rosenberg P, Koch G, et al. Aqueous vascular endothelial growth factor as a predictor of macular thickening following cataract surgery in patients with diabetes mellitus. Am J Ophthalmol. 2016;148:895–901.
- Mittra RA, Borrillo JL, Dev S, Mieler WF, Koenig SB. Retinopathy progression and visual outcomes after phacoemulsification in patients with diabetes mellitus. Arch Ophthalmol. 2010;118:912–917.
- Liao SB, Ku WC. Progression of diabetic retinopathy after phacoemulsification in diabetic patients: A three-year analysis. Chang Gung Med J. 2013;26:829–834.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.