Efficacy of Autologous vs. Homologous Costal Cartilage Grafts in Dorsal Augmentation Rhinoplasty: A Systematic Review and Meta-analysis
2 Medical Intern, Imam Muhammad Ibn Saud Islamic University, Riyadh, Saudi Arabia
3 ER Resident, Ibn Sina National College, Jeddah, Saudi Arabia
4 Medical Intern, Jazan University, Jazan, Saud University, Saudi Arabia
5 Medical Intern, Jazan Umm AlQura University, Makkah, Saudi University, Saudi Arabia
6 General Practitioner, King Salman Specialist Hospital, Hail, Saudi Arabia
7 Medical Intern, king Khalid University, Abha City, Saudi Arabia, Email: mazen345@hotmail.com
Citation: Alhussain OH, et al. Efficacy of Autologous vs. Homologous Costal Cartilage Grafts in Dorsal Augmentation Rhinoplasty: A Systematic Review and Meta-analysis. Ann Med Health Sci Res. 2020;10:1100-1104.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Even though septal cartilage is an excellent source if available, additional material is often required for revision. Costal and auricular cartilages are well-accepted sources and thought to be superior to alloplastic implants because of the lower chance of infection and extrusion. Due to the larger quantity of cartilage available with costal cartilage in comparison with auricular cartilage, costal cartilage is often the graft of choice in augmentation rhinoplasty. Aim: This work aims to determine the efficacy and safety of Irradiated Homologous Costal Cartilage (IHCC) versus Autologous Costal Cartilage (ACC) grafts in dorsal augmentation rhinoplasty patients. Materials and Methods: A systematic search was performed over different medical databases to identify Otolaryngology studies, which studied the outcome of the IHCC group versus the ACC group of dorsal augmentation rhinoplasty patients. Using the meta-analysis process, either with fixed or random-effects models, we conducted a meta-analysis on the warping rate as a primary outcome, and resorption and revision surgery rates as a secondary outcome. Results: Seven studies were identified involving 634 patients, with 302 patients in the IHCC group, and 322 patients in the ACC group. The meta-analysis process revealed a highly significant decrease in the warping rate in the IHCC group compared to the ACC group (p=0.002). We found a non-significant difference in resorption rate and revision surgery rates in the IHCC group compared to the ACC group (p>0.05). Conclusion: To conclude, no significant difference between autologous and homologous costal cartilage grafts, including resorption, or revisions, in patients undergoing dorsal augmentation rhinoplasty, but IHCC was safer approach concerning warping rate.
Keywords
Dorsal Augmentation Rhinoplasty; Irradiated Homologous Costal Cartilage (IHCC); Autologous Costal Cartilage (ACC)
Introduction
Surgeons should understand not only the anatomy but additionally the anatomical relationship between the bone or cartilage as the body and the pores and skin and soft tissue as the envelope. What the surgeon does to correct the nasal shape is particularly done by changing the frame shape. The key to rhinoplasty is in understanding how to alternate the shape of the envelope by changing the frame. Also, very important is the experience of nasal aesthetics, but it is difficult to explain aesthetics in general. Aesthetics depends on culture, society, and community, and it is usually changing. There’s no single gold standard in nasal aesthetic. [1]
In hardly ever any other field outcome is more obvious as in plastic aesthetic nasal surgical treatment. Both the quality of the procedure and the quality of the result play an outstanding role in the area of aesthetics. Expectations and interests of the surgeon are not usually congruent with those of the patient. Furthermore, payers, in the case of combination surgical treatment, have their focus on quality, which is often confused with the economy. Objective standards play an essential role for the doctor, with soft standards being very essential for patients. This is much greater difficult because beauty is in the eye of the beholder and must be compatible with functional conditions such as respiration and smell. In the variety of quality standards, it is hard to make the right choice of surgeon for the non-professional, especially in the face of countless seals, certificates, and the influence of the internet and social media. [2]
Patients with nasal airway obstruction (NAO) secondary to nasal valve compromise will frequently require a functional septorhinoplasty (FSRP) for correction of symptomatic nasal obstruction. In primary FSRP, septal cartilage is the grafting cloth of preference for most surgeons. However, while sufferers document a record of previous nasal surgical treatment, the surgeon should be prepared to utilize an alternative grafting material if a septoplasty has been achieved and/or the septal cartilage is insufficient for the reconstructive needs of the patient. Many implant and grafting options are available. [3]
Augmentation rhinoplasty requires the addition of cartilage to offer improved support to the structure of the nostril. Even though septal cartilage is an excellent source if available, additional material is often required for revision. Costal and auricular cartilages are well-accepted sources and thought to be superior to alloplastic implants because of the lower chance of infection and extrusion. Due to the larger quantity of cartilage available with costal cartilage in comparison with auricular cartilage, costal cartilage is often the graft of choice in augmentation rhinoplasty. However, the usage of costal cartilage has hazards. The threat of warping is often discussed, which has spurred numerous maneuvers to mitigate this chance, including carving techniques, suture techniques, microplate fixation, and Kirschner wires. [4]
This work aims to determine the efficacy and safety of autologous vs. homologous costal cartilage grafts in dorsal augmentation rhinoplasty patients.
Literature Review
Our review came following the (PRISMA) statement guidelines. [5]
Study eligibility
The included studies should be in English, a journal published article, and a human study describing dorsal augmentation rhinoplasty patients. The excluded studies were non-English or animal studies or describing other types of rhinoplasty.
Study identification
Basic searching was done over the PubMed, Cochrane library, and Google scholar using the following keywords: Dorsal Augmentation Rhinoplasty, Irradiated Homologous Costal Cartilage (IHCC), Autologous Costal Cartilage (ACC).
Data extraction and synthesis
RCTs, clinical trials, and comparative studies, which studied the outcome of the IHCC group versus ACC group of dorsal augmentation rhinoplasty patients, will be reviewed.
Outcome measures included warping rate (as a primary outcome), resorption and revision surgery rates (as secondary outcomes)
Study selection
We found 150 records, 90 excluded based on title and abstract review; 60 articles are searched for eligibility by full-text review; 15 articles cannot be accessed; 20 studies were reviews and case reports; 11 were not describing functional outcome; the desired graft not used in 7 studies leaving 7 studies that met all inclusion criteria.
Statistical methodology
The pooling of data, Proportions (%), Odds Ratios (ORs), Standard Mean Differences (SMDs), with 95% confidence intervals (CI) were done, using MedCalc ver. 18.11.3 (MedCalc, Belgium). According to heterogeneity across trials using the I2- statistics; a fixed-effects model or random-effects model were used in the meta-analysis process.
Results
The included studies published between 2004 and 2020. Regarding the type of included studies, 6 studies (out of 7 studies) were retrospective while 1 study was prospective [Table 1]. [6-12] Regarding patients’ characteristics, the total number of patients in all the included studies was 634 patients, with 302 patients in the IHCC group, and 322 patients in the ACC group, while their average follow-up time was (14.6 months) [Table 1]. The mean age of all patients was (32.4 years) [Table 1].
Table 1: Patients and study characteristics.
| N | Author | Type of study | Number of patients | Age (average years) | Follow-up time (average months) | ||
|---|---|---|---|---|---|---|---|
| Total | IHCC group | ACC group | |||||
| 1 | Strauch, Erhard, and Baum [6] | Retrospective | 17 | 12 | 5 | 46.5 | 7 |
| 2 | Al-Qattan [7] | Prospective | 21 | 10 | 11 | 30 | 44 |
| 3 | Balaji [8] | Retrospective | 157 | 55 | 102 | 21.4 | 3 |
| 4 | Joo and Jang [9] | Retrospective | 244 | 176 | 68 | 30.3 | --- |
| 5 | Bhat et al. [10] | Retrospective | 12 | 6 | 6 | 26 | 6 |
| 6 | Wee et al. [11] | Retrospective | 83 | 20 | 63 | 30.6 | 12 |
| 7 | Rogal, Glasgold, and Glasgold [12] | Retrospective | 100 | 23 | 77 | 42 | 16 |
#Studies arranged via publication year.
A meta-analysis study was done on 7 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=634) [Table 2]. [6-12]
Table 2: Summary of outcome measures in all studies.
| N | Author | Primary outcome | Secondary outcomes | ||||
|---|---|---|---|---|---|---|---|
| Warping rate | Resorption rate | Revision surgery rate | |||||
| IHCC group | ACC group | IHCC group | ACC group | IHCC group | ACC group | ||
| 1 | Strauch, Erhard, and Baum [6] | 0 | 0 | 0 | 0 | 1 | 0 |
| 2 | Al-Qattan [7] | 0 | 0 | 0 | 0 | 0 | 1 |
| 3 | Balaji [8] | 5 | 36 | --- | --- | --- | --- |
| 4 | Joo and Jang [9] | --- | --- | --- | --- | 41 | 17 |
| 5 | Bhat et al. [10] | 0 | 0 | 0 | 0 | 0 | 0 |
| 6 | Wee et al. [11] | 2 | 8 | 2 | 6 | --- | --- |
| 7 | Rogal, Glasgold, and Glasgold [12] | 0 | 0 | 2 | 17 | 2 | 17 |
Each outcome was measured by:
Odds Ratio (OR):
• For warping rate
• For resorption rate
• For revision surgery rate
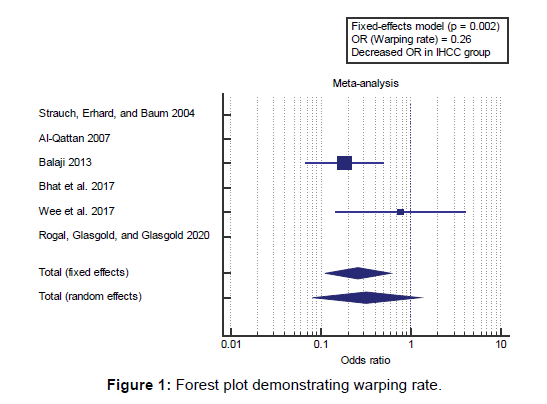
Concerning the primary outcome measure, we found 6 studies reported a warping rate with a total number of patients (N=390). I2 (inconsistency) was 53% with a non-significant Q test for heterogeneity (p<0.05), so fixed-effects model was carried out; with overall OR=0.26 (95% CI=0.111 to 0.605). Using the fixed-effects model, the meta-analysis process revealed a highly significant decrease in the warping rate in the IHCC group compared to the ACC group (p=0.002) [Figure 1].
Concerning the secondary outcome measures, we found 5 studies reported resorption rates with a total number of patients (N=233). I2 (inconsistency) was 0% with a non-significant Q test for heterogeneity (p>0.05), so fixed-effects model was carried out; with overall OR=0.52 (95% CI=0.173 to 1.617). Using the fixed-effects model, the meta-analysis process revealed a nonsignificant difference in the resorption rate in the IHCC group compared to the ACC group (p>0.05) [Figure 2].
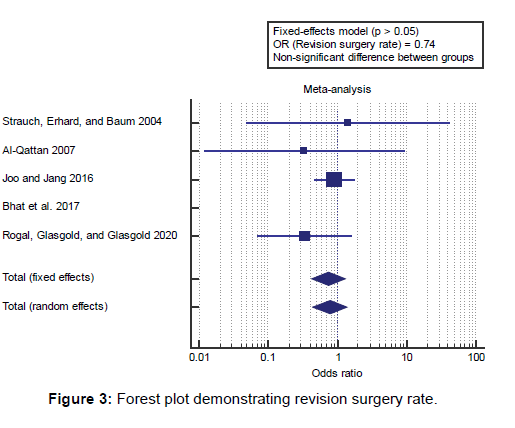
We found 5 studies reported revision surgery rates with a total number of patients (N=394). I2 (inconsistency) was 0% with a non-significant Q test for heterogeneity (p>0.05), so fixedeffects model was carried out; with overall OR=0.74 (95% CI=0.426 to 1.309). Using the fixed-effects model, the metaanalysis process revealed a non-significant difference in the revision surgery rate in the IHCC group compared to the ACC group (p>0.05) [Figure 3].
Discussion
This work aims to determine the efficacy and safety of autologous vs. homologous costal cartilage grafts in dorsal augmentation rhinoplasty patients concerning the primary outcome measure, we found 6 studies reported a warping rate with a total number of patients (N=390).
Using the fixed-effects model, the meta-analysis process revealed a highly significant decrease in warping rate in IHCC group compared to ACC group (p=0.002), which came in agreement with M. K. Suh, Lee, and Kim, [13] Justicz et al., [3] M.-K. Suh et al., [14] Yen et al. [15] and Lavernia et al. [16]
M. K. Suh, Lee, and Kim reported that, in this study, we included all patients who underwent augmentation rhinoplasty with IHCC, no matter graft location. The retrospective evaluation demonstrated a low complication rate for IHCC grafts. The resorption rate of 1.2%, fracture rate of 0.6%, and warping rate of 0.6% were confirmed. [13]
Justicz et al. reported that Of IHCC grafts in 357 patients after 386 rhinoplasties over 24 years, the rate of complications (3.25%) was no more than rhinoplasty difficulty rates while ACC grafts had been used.4 The IHCC grafts in this observe had been evaluated for warping (1.06%). [3]
M.-K. Suh et al. reported that there has been no noticeable graft warping or infective IHCC absorption. But, three patients underwent revision: 2 cases of graft avulsion fracture and 1 case of minimal nasal obstruction. Nasal length, which had increased an average of 8.5% after the procedure, became maintained at follow-up 2 years postoperatively. [14]
Yen et al. reported that the framework is vital for restoring aesthetics and function after nasal reconstruction by fortifying the construct and maximizing airflow. Cartilage is typically harvested from the nasal septum, auricular concha, or rib. Autologous materials are favored but aren’t immune to absorption and warping. [15]
Lavernia et al. reported that passaged costal chondrocytes have shown the ability to form neocartilage that is capable of remodeling in vivo to promote healing. While costal cartilage is used clinically as graft material, it frequently warps when cutting into grafts. However, while costal cartilage is used as a cell source, in particular for an allogeneic approach, issues of warping and donor site morbidity are eliminated. [16]
Concerning the secondary outcome measures, we found 5 studies reported resorption rate with a total number of patients (N=233).
Using the fixed-effects model, the meta-analysis process revealed a non-significant difference in resorption rate in IHCC group compared to ACC group (p>0.05), which came in agreement with Justicz et al., [3] Vila et al., [4] Toriumi [17] and Kim et al. [18]
Justicz et al. reported that, compared outcomes in patients who underwent rhinoplasty with ACC and IHCC. In 63 patients who had septorhinoplasty using ACC and 20 who had septorhinoplasty using IHCC, notable resorption occurred more frequently in patients using IHCC (n=6, 30%) than with ACC (n=2, 3%). [3]
Vila et al. reported that, given the varying results on outcomes with IHCC in rhinoplasty, no research, to our knowledge, have definitively demonstrated that patients experience better complications, including warping or resorption, with IHCC grafts in comparison with autologous costal cartilage grafts. Our goal became to compare rates of complications related to autologous vs. IHCC grafts in patients undergoing augmentation rhinoplasty in the published literature, including graft resorption, infection, warping, contour irregularity, and revision fees. [4]
Toriumi reported that all patients had been followed up for more than 1 yr (mean, 25.6 months). The IHCC was used in the dorsum, septum, and nasal tip. The incidence of infection and warping was not different among the two groups. Notable resorption was seen in 6 patients using IHCC (30%) and 2 patients using ACC (3%), a statistically significant difference between the two groups. [17]
Kim et al. reported that, reduction and corrective rhinoplasty are the most prevalent rhinoplastic surgery, augmentation rhinoplasty the most commonly performed cosmetic procedures in Asians, and the materials used for augmentation is an essential issue for debates amongst Asian plastic surgeons who perform rhinoplasty. Although there may be no argument that autologous tissues are the most ideal augmentation material, they’ve limited availability, unpredictable resorption rates, the difficulty of handling, and frequently donor site morbidity. Hence, alloplastic ma¬terials are frequently used as an alternative. [18]
Our result came in disagreement with Lavernia et al. [16] Lavernia et al. reported that, while the use of IHRGs is considered safe, the occurrence of IHRG resorption (31%) has been reported to be substantially greater than that of autologous costal cartilage (3%). This resorption, but maybe because of the decellularization processing or the absence of possible cells inside the dealt with graft tissue and its next lack of ability to rework in vivo. extra research should be performed to determine the elements which may affect its variable success. [16]
We found 5 studies reported revision surgery rates with a total number of patients (N=394).
Using the fixed-effects model, the meta-analysis process revealed a non-significant difference in revision surgery rate in the IHCC group compared to the ACC group (p>0.05), which came in agreement with Vila et al., [4] Justicz et al. [3]
Vila et al. reported that, of 576 unique citations, 54 researches were included in our systematic evaluation; 28 research have been included. Our search captured 1041 patients of whom 741 received autologous grafts and 293 received IHCC grafts (regardless of type), while autologous cartilage (n=748) vs. IHCC (n=153) vs. Tutoplast cartilage (n=140) grafts were in comparison, no difference in warping (5%), resorption (2%), contour irregularity (1%), infection (2%), or revision surgical procedure (5%) was found. [4]
Justicz et al. reported that there has been no significant difference in mean nose scores among the ACC and IHCC cohorts at the preoperative visit (68.5 [standard deviation, SD 24.1] and 71.7, respectively; p<0.6) or first postoperative visit (30.4 and 33.9, respectively; p<0.6) or next visits. Nose scores demonstrated a clinically and statistically significant improvement at all followup time factors for both the ACC and IHCC groups. Patients who underwent grafting with IHCC have been significantly older than those with ACC; the average age of 55.6 [SD: 17.3] as opposed to 40.1 [SD: 12.1]; (p<0.001). IHCC (0.05%) patients had postoperative infections; both resolved with antibiotics, however one required revision surgical operation. [3]
Our result came in disagreement with Toriumi. [17]
Toriumi reported that, in the discussion, the authors note that the higher resorption rates for patients the usage of IHCC could be in part because of the truth that four of the 6 patients the use of IHCC had undergone revision, which may have had reduced blood supply to the grafting. [17]
Conclusion
To conclude, no significant difference between autologous and homologous costal cartilage grafts, including resorption, or revisions, in patients undergoing dorsal augmentation rhinoplasty, but IHCC was safer approach concerning warping rate.
Competing Interests
The authors declare that they have no competing interests. All the listed authors contributed significantly to the conception and design of study, acquisition, analysis, and interpretation of data and drafting of the manuscript, to justify authorship.
REFERENCES
- Sugawara Y. A Practical Approach to Asian Rhinoplasty. Springer; 2020.
- Dacho A. Which Quality Makes the Difference?-Cosmetic Rhinoplasty. Laryngo-Rhino-Otologie 2020;99:S165.
- Justicz N, Fuller JC, Levesque P, Lindsay RW. Comparison of NOSE scores following functional Septorhinoplasty using autologous versus cadaveric rib. Arch Plast Surg. 2019;35:103-108.
- Vila PM, Jeanpierre LM, Rizzi CJ, Yaeger LH, Chi JJ. Comparison of Autologous vs. Homologous Costal Cartilage Grafts in Dorsal Augmentation Rhinoplasty: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg. 2020;146:347-354.
- Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions. Bmj 2009;339.
- Strauch B, Erhard HA, Baum T. Use of irradiated cartilage in rhinoplasty of the non-Caucasian nose. Aesthetic Plast Surg. 2004;24:324-330.
- Al-Qattan MM. Augmentation of the nasal dorsum with autogenous costal cartilage using the “edge-on” technique. Ann Plast Surg. 2007;59:642-644.
- Balaji SM. Costal cartilage nasal augmentation rhinoplasty: Study on warping. Ann Maxillofac Surg 2013;3:20-24.
- Joo YH, Jang YJ. Comparison of the surgical outcomes of dorsal augmentation using expanded polytetrafluoroethylene or autologous costal cartilage. JAMA Facial Plast Surg. 2016;18:327-332.
- Bhat U, Gupta T, Nair M, Mantri M, Pawar M, Baliarsing A. Three component cartilage framework reconstruction for correction of post-traumatic nasal septal collapse. Indian J Plast Surg. 2017;50:236-243.
- Wee JH, Mun SJ, Na WS, Kim H, Park JH, Kim D-K, et al. Autologous vs. irradiated homologous costal cartilage as graft material in rhinoplasty. JAMA Facial Plast Surg. 2017;19:183-188.
- Rogal J, Glasgold A, Glasgold RA. Safety and Efficacy of Non-and Minimally Irradiated Homologous Costal Cartilage in Primary and Revision Rhinoplasty. JAMA Facial Plast Surg. 2020.
- Suh MK, Lee SJ, Kim YJ. Use of irradiated homologous costal cartilage in rhinoplasty: complications in relation to graft location. J Craniofac Surg. 2018;29:1220-1223.
- Suh MK, Ahn ES, Kim HR, Dhong ES. A 2-year follow-up of irradiated homologous costal cartilage used as a septal extension graft for the correction of contracted nose in Asians. Ann Plast Surg. 2013;71:45-49.
- Yen CI, Zelken JA, Chang CS, Chen HC, Yang SY, Chang SY, et al. Preventing nasal airway collapse with irradiated homologous costal cartilage versus expanded polytetrafluoroethylene: a novel animal model for nasal airway reconstruction. Scientific Reports 2019;9:1-7.
- Lavernia L, Brown WE, Wong BJ, Hu JC, Athanasiou KA. Toward tissue-engineering of nasal cartilages. Acta Biomaterialia 2019;88:42-56.
- Toriumi DM. Choosing autologous vs. irradiated homograft rib costal cartilage for grafting in rhinoplasty. JAMA Facial Plastic Surgery 2017;19:188-189.
- Kim HS, Park SS, Kim MH, Kim MS, Kim SK, Lee KC. Problems associated with alloplastic materials in rhinoplasty. Yonsei Medical Journal 2014;55:1617-1623.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.