Enhanced Recovery Program (ERAS) and Colorectal Surgery: A Systematic Review and Meta-analysis
2 General Surgery Resident, King Abdulaziz Specialist Hospital, Taif, Saudi Arabia
3 Medical Intern, Ibn Sina National College, Jeddah, Saudi Arabia
4 6th Year Medical Student, Jouf University, Sakaka, Saudi Arabia
Citation: Althobaiti TS, et al. Enhanced Recovery Program (ERAS) and Colorectal Surgery: A Systematic Review and Meta-analysis. Ann Med Health Sci Res. 2020;10:1089-1094.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Enhanced Recovery after Surgery (ERAS) protocols are rapidly becoming the standard of care for patients undergoing an elective colorectal surgical operation to speed recovery and decrease the postoperative length of stay (LOS) and morbidity. Aim: This work aims to determine the efficacy and safety of the Enhanced Recovery Program (ERAS) on postoperative outcomes in colorectal surgery patients. Materials and Methods: A systematic search was performed over different medical databases to identify General Surgery studies, which studied the outcome of the ERAS group versus the Conventional group of colorectal surgery patients. Using the meta-analysis process, either with fixed or random-effects models, we conducted a meta-analysis on length of hospital stay as a primary outcome and overall complications and mortality rates as a secondary outcome. Results: Ten studies were identified involving colorectal surgery patients, 3421 patients, with 1988 patients in the ERAS group, and 1433 patients in the Conventional group. The meta-analysis process revealed a highly significant decrease in mean length of hospital stay (LOS), in the ERAS group compared to the Conventional group (p<0.001). We also found a significant decrease in complications rate in the ERAS group compared to the Conventional group (p=0.022), and a highly significant decrease in mortality rate in the ERAS group compared to the Conventional group (p=0.005). Conclusion: To conclude, ERAS program is an evidence-based multimodal perioperative protocol focused on stress reduction and the promotion of a rapid postoperative recovery. ERAS helps lowering both recovery time and postoperative complication rates while being cost-effective at the same time.
Keywords
ERAS; colorectal surgery
Introduction
Following predominant surgical treatment, the first days after discharge are a prone time for patients. This period of vulnerability has previously been defined as a post-hospital syndrome. Signs, which were not present while in hospital, may arise at home and patients must be capable of determining whether or not those symptoms are a normal part of recovery or whether they indicate the development of a complication. [1]
Enhanced Recovery after Surgery (ERAS) protocols are now the standard care for colorectal surgery patients to speed recovery and decrease the postoperative length of stay (LOS) and morbidity. While those protocols encompass numerous interventions including modified preoperative oral intake, avoidance of mechanical bowel preparation, early postoperative mobilization, and oral intake, and emphasis on laparoscopic surgical technique, one of the cornerstones of ERAS protocols is the usage of multimodal analgesic therapy. [2]
Studies on ERAS protocols have mainly originated from European countries and the USA (in which the term, ‘fast track surgical procedure’, is also used), and only a few had been performed in Asian countries. ERAS protocols had been introduced in Japan around 2008 and were initially introduced in our hospital to patients who underwent colorectal resection in July 2010. We previously demonstrated that ERAS protocols helped reduce the length of postoperative hospital stay without adversely affecting morbidity, indicating that ERAS protocols are feasible and effective in Japan, with its unique medical subculture and public health insurance system. [3]
Internationally, ERAS implementation has largely occurred inside a single site. There has been one large system-wide reported try to implement multiple guidelines for elective colorectal, orthopedic, gynecologic, and urologic surgical treatment, in the United Kingdom’s enhanced recovery Partnership program (ERPP). A recent report from ERPP suggests that stringent delivery of a regular care pathway results in extra health benefits for the patient and a cost-saving for the healthcare organization. [4]
This work aims to determine the efficacy and safety of the Enhanced Recovery Program (ERAS) on postoperative outcomes in colorectal surgery patients.
Literature Review
Our review came following the (PRISMA) statement guidelines. [5]
Study eligibility
The included studies should be in English, a journal published article, and a human study describing colorectal surgery patients. The excluded studies were non-English or animal studies or describing other types of cancer patients (e.g. pancreatic cancer).
Study identification
Basic searching was done over the PubMed, Cochrane library, and Google scholar using the following keywords: ERAS, colorectal surgery.
Data extraction and synthesis
RCTs, clinical trials, and comparative studies, which studied the outcome of ERAS group versus Conventional group of colorectal surgery patients, will be reviewed. Outcome measures included length of hospital stay as a primary outcome, and on overall complications and mortality rates as secondary outcomes.
Study selection
We found 180 records, 130 excluded based on title and abstract review; 50 articles are searched for eligibility by full-text review; 14 articles cannot be accessed; 13 studies were reviews and case reports; 5 were not describing functional outcome; the desired post-operative protocol not used in 8 studies leaving 10 studies that met all inclusion criteria.
Statistical methodology
The pooling of data, Proportions (%), Odds Ratios (ORs), Standard Mean Differences (SMDs), with 95% confidence intervals (CI) were done, using MedCalc ver. 18.11.3 (MedCalc, Belgium). According to heterogeneity across trials using the I2- statistics; a fixed-effects model or random-effects model were used in the meta-analysis process.
Results
The included studies published between 2003 and 2019. Regarding the type of surgery, 5 studies described open colorectal surgery, and the other 5 studies described open vs. laparoscopic colorectal surgery [Table 1]. [6-15]
Table 1: Patients and study characteristics.
| N | Authors | Type of surgery | Number of patients | Age (average years) | Follow-up time (average days) | Implemented ERAS items | ||
|---|---|---|---|---|---|---|---|---|
| Total | ERAS group | Conventional group | ||||||
| 1 | Anderson et al. [6] | Open | 25 | 14 | 11 | 66 | 30 | 12 |
| 2 | Gatt et al. [7] | Open | 39 | 19 | 20 | 67 | 30 | 12 |
| 3 | Muller et al. [8] | Open | 151 | 76 | 75 | 60.5 | 30 | 9 |
| 4 | Vlug et al. [9] | LPS/open | 400 | 193 | 207 | 66 | 30 | 11 |
| 5 | Ren et al. [10] | Open | 597 | 299 | 298 | 60 | 30 | 11 |
| 6 | Nelson et al. [11] | LPS/open | 1332 | 350 | 982 | 63 | -- | -- |
| 7 | Forsmo et al. [12] | LPS/open | 164 | 80 | 84 | 66.5 | -- | 15 |
| 8 | Tejedor et al. [13] | LPS/open | 312 | 156 | 156 | 79 | -- | 18 |
| 9 | Zeng et al. [14] | LPS/open | 251 | 94 | 157 | 78 | 30 | -- |
| 10 | Ostermann et al. [15] | Open | 150 | 75 | 75 | 79 | 30 | -- |
#Studies arranged via publication year. LPS: Laparoscopy.
Regarding patients’ characteristics, the total number of patients in all the included studies was 3421 patients, with 1988 patients in the ERAS group, and 1433 patients in Conventional group, while their average follow-up time was (30 days) [Table 1].
The mean age of all patients was (68.5 years), and the median number of implemented ERAS items was 12 ERAS items [Table 1]. A meta-analysis study was done on 10 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=3421) [Table 2].
Table 2: Summary of outcome measures in all studies.
| N | Authors | Primary outcome | Secondary outcomes | ||||
|---|---|---|---|---|---|---|---|
| Length of hospital stay (LOS) | Complications rate | Mortality rate | |||||
| ERAS group | Conventional group | ERAS group | Conventional group | ERAS group | Conventional group | ||
| 1 | Anderson et al. [6] | 3.9 | 7 | 4 | 6 | 0 | 1 |
| 2 | Gatt et al. [7] | 6.6 | 9 | 9 | 15 | 1 | 0 |
| 3 | Muller et al. [8] | 6.7 | 10.3 | 16 | 47 | 0 | 0 |
| 4 | Vlug et al. [9] | 5 | 6 | 33 | 33 | 2 | 2 |
| 5 | Ren et al. [10] | 5.7 | 6.6 | 28 | 29 | -- | -- |
| 6 | Nelson et al. [11] | 6.7 | 9.8 | 315 | 74 | -- | -- |
| 7 | Forsmo et al. [12] | 5 | 7 | 3 | 10 | 0 | 2 |
| 8 | Tejedor et al. [13] | 6 | 8 | 62 | 77 | 3 | 18 |
| 9 | Zeng et al. [14] | 6 | 8 | 25 | 70 | 2 | 4 |
| 10 | Ostermann et al. [15] | 5 | 9 | 26 | 49 | 1 | 2 |
Each outcome was measured by:
Standard Mean Difference (SMD)
• For LOS.
Odds Ratio (OR)
• For complications rate.
• For the mortality rate.
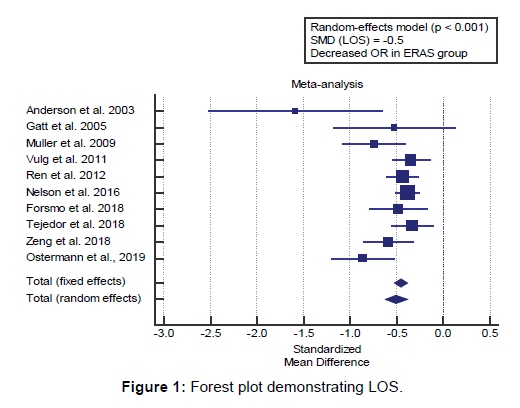
Concerning the primary outcome measure, we found 10 studies reported LOS with a total number of patients (N=3421). I2 (inconsistency) was 54.5% with a significant Q test for heterogeneity (p=0.019), so random-effects model was carried out; with overall SMD= -0.504 (95% CI=-0.624 to -0.383). Using the random-effects model, the meta-analysis process revealed a highly significant decrease in mean length of hospital stay (LOS), in the ERAS group compared to the Conventional group (p<0.001) [Figure 1].
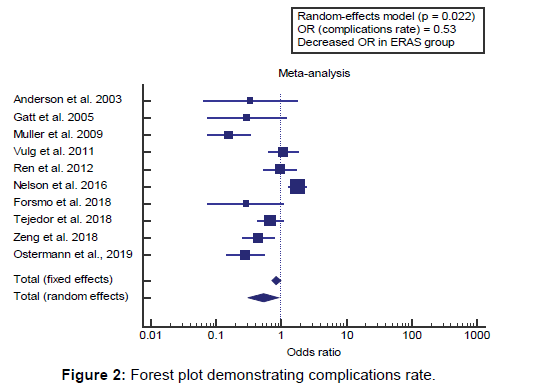
Concerning the secondary outcome measures, we found 10 studies reported complications rate with a total number of patients (N=3421). I2 (inconsistency) was 86.8% with a highly significant Q test for heterogeneity (p<0.0001), so random-effects model was carried out; with overall OR= 0.53 (95% CI=0.310 to 0.914).
Using the random-effects model, the meta-analysis process revealed a significant decrease in complications rate in the ERAS group compared to the Conventional group (p=0.022) [Figure 2].
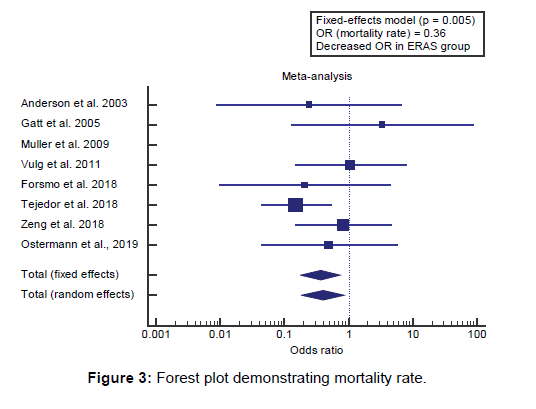
We found 8 studies reported mortality rates with a total number of patients (N=1492). I2 (inconsistency) was 0.2% with a nonsignificant Q test for heterogeneity (p > 0.05), so fixed-effects model was carried out; with overall OR= 0.36 (95% CI=0.179 to 0.735).
Using the fixed-effects model, the meta-analysis process revealed a highly significant decrease in the mortality rate in the ERAS group compared to the Conventional group (p=0.005) [Figure 3].
Discussion
This work aims to determine the efficacy and safety of Enhanced Recovery Program (ERAS) on postoperative outcomes in colorectal surgery patients. The included studies published between 2003 and 2019. Regarding the type of surgery, 5 studies described open colorectal surgery, and the other 5 studies described open vs. laparoscopic colorectal surgery.
Regarding patients’ characteristics, the total number of patients in all the included studies was 3421 patients, with 1988 patients in the ERAS group, and 1433 patients in the Conventional group, while their average follow-up time was (30 days).
The mean age of all patients was (68.5 years), and the median number of implemented ERAS items was 12 ERAS items. A meta-analysis study was done on 10 studies that described and compared the 2 different groups of patients; with an overall number of patients (N=3421).
Concerning the primary outcome measure, we found 10 studies reported LOS with a total number of patients (N=3421). Using the random-effects model, the meta-analysis process revealed a highly significant decrease in mean length of hospital stay (LOS), in ERAS group compared to Conventional group (p<0.001), which came in agreement with Nelson et al., [4] Pędziwiatr et al., [16] Cavallaro and Bordeianou, [17] Slieker et al., [18] Rinninella et al., [19] Zhu, Agarwala, and Bao, [20] Yeung et al. [21] and Forsmo et al. [22]
Nelson et al. reported that a complete of 1333 patients (350 pre- and 983 submit-ERAS) had been analyzed. Of this number, 55% have been adult males. Median overall guideline compliance was 39% in pre- and 60% in post-ERAS patients. Median LOS was 6 days for pre-ERAS in comparison to four.5 days in post-ERAS patients with the longest implementation (p value>0.0001). [4]
Pędziwiatr et al. reported that total or subtotal gastrectomies achieved between 1996 and 2014, showed no evidence in support of drainage concerning morbidity-mortality, or in the diagnosis or control of leakage. Lastly, early postoperative oral feeding in comparison with traditional, or late, feeding is related to shorter hospital length of stay and isn’t always associated with an increase in clinically relevant complications. [16]
Cavallaro and Bordeianou reported that more desirable recovery after surgery (ERAS) protocols were demonstrated to improve hospital duration of stay and outcomes in patients undergoing a colorectal surgical procedure. This text provides the specific components of an ERAS protocol implemented on the authors’ institution. [17]
Slieker et al. reported that enhanced healing after surgery (ERAS) pathway has been proven to be beneficial for patients and need to now be taken into consideration as the standard of care in a colorectal surgical operation. It allows for decrease complication rates and shortened length of hospital life at reduced costs. [18]
Rinninella et al. reported that Post-operative complications (POC) and length of hospital stay (LOS) are important issues and impact on hospital costs. Enhanced recovery after surgical treatment (ERAS) protocols are effective 50 in reducing morbidity and LOS after major surgical treatment. We propose a nutritional protocol within the ERAS program in colorectal surgical operation, beginning from preadmission. [19]
Zhu, Agarwala, and Bao reported that oral carbohydrate loading leads to other beneficial effects as well. In 2014, a Cochrane review discussed the results of 27 trials where patients received at least 45 g of carbohydrates within 4 hours earlier than surgical treatment or anesthesia. A carbohydrate load led to a shortened time to flatus by 0.39 days and a small reduction in the period of hospital stay by way of 0.30 days as compared with traditional fasting requirements or placebo controls. [20]
Yeung et al. reported that the LOS for the ERAS group was significantly shorter than that of the conventional group (6.5 compared with 9.7 d; P=0.049). There were no significant differences between the 2 groups for postoperative measures of gastrointestinal function. [21]
Forsmo et al. reported that total hospital stay was significantly shorter in the ERAS group with education than the standard care group (median, 6 days vs. 9 days; p<0.001). Regarding overall major and minor morbidity, re-admission rate. [22]
Concerning the secondary outcome measures, we found 10 studies reported complications rate with a total number of patients (N=3421). Using the random-effects model, the metaanalysis process revealed a significant decrease in complications rate in ERAS group compared to Conventional group (p=0.022), which came in agreement with Zhu, Agarwala, and Bao, [20] Pędziwiatr et al., [16] Cavallaro and Bordeianou, [17] Yeung et al. [21] and Nelson et al. [4]
Zhu, Agarwala, and Bao reported that modern perioperative care in colorectal surgical treatment is guided with the aid of enhanced recovery after surgery (ERAS) pathways.1 initially developed in Europe in the 1990s to reduce variability and improve outcomes, those units of recommendations aim to offer preoperative, intraoperative, and postoperative interventions to decrease complications and enhance patient recovery. [20]
Pędziwiatr et al. reported that the ERAS Compliance Group showed in a large-scale study on over 1500 colorectal cancer patients that increasing ERAS compliance correlates with fewer complications. [16]
Cavallaro and Bordeianou reported that we were pleased to find that the audit showed a 1-day reduction in inpatient length of stay and a 60% reduction in postoperative complications, including surgical infections. [17]
Yeung et al. reported that the ERAS group had shorter LOS (P=0.049) and fewer total infectious complications (P=0.01). Nausea was a predictor of protein intake. Nutrition variables were independent predictors of earlier discharge after potential confounders were controlled for. The ERAS group had significantly fewer total complications (39% compared with 61%; P=0.04) and significantly fewer minor complications (32% compared with 57%; P=0.01). Total infectious complications were also fewer in the ERAS group (14% compared with 35%; P=0.01), including wound infections (1% compared with 11%; P=0.04). [21]
Nelson et al. reported that adjusted risk ratio (RR) was 1.71, for 30-day readmission, comparing pre- to publish-ERAS patients. the proportion of patients who developed at least one complication was considerably reduced, from pre- to post- ERAS, the difference in proportions=11.7%, p-value: 0.0139. [4]
We found 8 studies reported mortality rates with a total number of patients (N=1492). Using the fixed-effects model, the metaanalysis process revealed a highly significant decrease in mortality rate in ERAS group compared to Conventional group (p=0.005), which came in agreement with Shida et al., [3] Wahl et al. [23] and Pędziwiatr et al. [16]
Shida et al. reported that median postoperative hospital stay was ten days in the traditional group, and seven days in the ERAS group, showing a 3-day reduction in hospital stay (p<0.01). According to the Clavien-Dindo classification, overall incidences of grade 2 or higher postoperative complications for the traditional and ERAS groups were 15 and 10% (p=0.48), and 30-day readmission rates were 0 and 1.3% (p=1.00), respectively. As for mortality, one patient in the traditional group died and none within the ERAS group (p=0.34). [3]
Wahl et al. reported that enhanced recovery after surgical operation (ERAS) pathways use standardized, multimodal perioperative techniques to reduce physiologic pressure prompted via the surgical procedure and to promote early recovery. ERAS protocols span the continuum of surgical care and consist of processes such as patient education, multimodal analgesia, and early mobility. Implementation of ERAS involves the collaboration of a multidisciplinary crew supporting the systematic coordination of procedures. Research has continuously shown that ERAS reduces LOS and may also reduce postoperative complications after surgical operation and mortality rates. [23]
Pędziwiatr et al. reported that the authors showed that the number of employed ERAS items ranged from 11 to 18 of the 20 recommended by the ERAS Society for elective procedures; patients treated within the guidelines had fewer postoperative complications, shorter hospital stays, with equal or lower mortality rates in certain studies. [16]
Our result came in disagreement with Forsmo et al. [22] and Thanh et al., [24] Forsmo et al. reported that the study revealed significantly shorter hospital stay for patients treated with ERAS care and stoma education than patients receiving standard care for stoma after colorectal surgery. The two treatment groups did not differ concerning mortality. [22]
Thanh et al. reported that, in total, 1295 post-ERAS patients (cases) and 331 pre-ERAS patients (controls) who had colorectal surgery between 2013 and 2015 in 6 hospitals/sites across Alberta were included in our analyses. There was no significant difference in mortality between the 2 groups during the study period (0.23% of cases v. 0.30% of controls, p=0.82). [24]
Conclusion
To conclude, ERAS program is an evidence-based multimodal perioperative protocol focused on stress reduction and the promotion of a rapid postoperative recovery. ERAS helps lowering both recovery time and postoperative complication rates while being cost-effective at the same time.
Competing Interests
The authors declare that they have no competing interests. All the listed authors contributed significantly to the conception and design of study, acquisition, analysis, and interpretation of data and drafting of the manuscript, to justify authorship.
REFERENCES
- Jones D, Musselman R, Pearsall E, McKenzie M, Huang H, McLeod RS. Ready to go home? Patients’ experiences of the discharge process in an Enhanced Recovery after Surgery (ERAS) program for colorectal surgery. J Gastrointest Surg. 2017;21:1865-1878.
- Simpson JC, Bao X, Agarwala A. Enhanced Recovery after Surgery (ERAS) for Colorectal Surgery: Pain Management in Enhanced Recovery After Surgery (ERAS) Protocols. Clin Colon Rectal Surg. 2019;32:121.
- Shida D, Tagawa K, Inada K, Nasu K, Seyama Y, Maeshiro T, et al. Modified enhanced recovery after surgery (ERAS) protocols for patients with obstructive colorectal cancer. BMC Surgery 2017;17:1-6.
- Nelson G, Kiyang LN, Crumley ET, Chuck A, Nguyen T, Faris P, et al. Implementation of Enhanced Recovery after Surgery (ERAS) across a provincial healthcare system: the ERAS Alberta colorectal surgery experience. World J Surg. 2016;40:1092-1103.
- Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions. BMJ 2009;339.
- Anderson ADG, McNaught CE, MacFie J, Tring I, Barker P, Mitchell CJ. Randomized clinical trial of multimodal optimization and standard perioperative surgical care. Br J Surg. 2003;90:1497-1504.
- Gatt M, Anderson ADG, Reddy BS, Hayward-Sampson P, Tring IC, MacFie J. Randomized clinical trial of multimodal optimization of surgical care in patients undergoing major colonic resection. British Journal of Surgery 2005;92:1354-1362.
- Muller S, Zalunardo MP, Hubner M, Clavien PA, Demartines N, Group ZFTS. A fast-track program reduces complications and length of hospital stay after open colonic surgery. Gastroenterology 2009;136:842-847.
- Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, et al. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg. 2011;254:868-875.
- Ren L, Zhu D, Wei Y, Pan X, Liang L, Xu J, et al. Enhanced Recovery After Surgery (ERAS) program attenuates stress and accelerates recovery in patients after radical resection for colorectal cancer: a prospective randomized controlled trial. World J Surg. 2012;36:407-414.
- Nelson G, Kiyang LN, Crumley ET, Chuck A, Nguyen T, Faris P, et al. Implementation of Enhanced Recovery after Surgery (ERAS) across a provincial healthcare system: the ERAS Alberta colorectal surgery experience. World J Surg. 2016;40:1092-1103.
- Forsmo HM, Erichsen C, Rasdal A, Tvinnereim JM, Körner H, Pfeffer F. Randomized controlled trial of extended perioperative counseling in enhanced recovery after colorectal surgery. Dis Colon Rectum. 2018;61:724-732.
- Tejedor P, Pastor C, Gonzalez-Ayora S, Ortega-Lopez M, Guadalajara H, Garcia-Olmo D. Short-term outcomes and benefits of ERAS program in elderly patients undergoing colorectal surgery: a case-matched study compared to conventional care. Int J Colorectal Dis. 2018;33:1251-1258.
- Zeng WG, Liu MJ, Zhou ZX, Wang ZJ. Enhanced recovery programme following laparoscopic colorectal resection for elderly patients. ANZ J Surg. 2018;88:582-586.
- Ostermann S, Morel P, Chalé J-J, Bucher P, Konrad B, Meier RP, et al. Randomized controlled trial of enhanced recovery program dedicated to elderly patients after colorectal surgery. Dis Colon Rectum. 2019;62:1105-1116.
- Pędziwiatr M, Mavrikis J, Witowski J, Adamos A, Major P, Nowakowski M, et al. Current status of enhanced recovery after surgery (ERAS) protocol in gastrointestinal surgery. Med Oncol. 2018;35:95.
- Cavallaro P, Bordeianou L. Enhanced Recovery after Surgery (ERAS) for Colorectal Surgery: Implementation of an ERAS Pathway in Colorectal Surgery. Clin Colon Rectal Surg. 2019;32:102.
- Slieker J, Frauche P, Jurt J, Addor V, Blanc C, Demartines N, et al. Enhanced recovery ERAS for elderly: a safe and beneficial pathway in colorectal surgery. Int J Colorectal Dis. 2017;32:215-221.
- Rinninella E, Persiani R, D’Ugo D, Pennestrì F, Cicchetti A, Di Brino E, et al. NutriCatt protocol in the Enhanced Recovery After Surgery (ERAS) program for colorectal surgery: The nutritional support improves clinical and cost-effectiveness outcomes. Nutrition 2018;50:74-81.
- Zhu AC-C, Agarwala A, Bao X. Enhanced Recovery after Surgery (ERAS) for Colorectal Surgery: Perioperative Fluid Management in the Enhanced Recovery after Surgery (ERAS) Pathway. Clin Colon Rectal Surg. 2019;32:114.
- Yeung SE, Hilkewich L, Gillis C, Heine JA, Fenton TR. Protein intakes are associated with reduced length of stay: a comparison between Enhanced Recovery after Surgery (ERAS) and conventional care after elective colorectal surgery. Am J Clin Nutr. 2017;106:44-51.
- Forsmo HM, Pfeffer F, Rasdal A, Sintonen H, Körner H, Erichsen C. Pre-and postoperative stoma education and guidance within an enhanced recovery after surgery (ERAS) programme reduces length of hospital stay in colorectal surgery. Int J Surg. 2016;36:121-126.
- Wahl TS, Goss LE, Morris MS, Gullick AA, Richman JS, Kennedy GD, et al. Enhanced recovery after surgery (ERAS) eliminates racial disparities in postoperative length of stay after colorectal surgery. Ann Surg. 2018;268:1026-1035.
- Thanh NX, Chuck AW, Wasylak T, Lawrence J, Faris P, Ljungqvist O, et al. An economic evaluation of the Enhanced Recovery After Surgery (ERAS) multisite implementation program for colorectal surgery in Alberta. Can J Surg. 2016;59:415.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.