Facial Trauma: Not a Stigma in a Newer Single Stage Reconstructive Surgery
- *Corresponding Author:
- Suryapratap Singh Tomar
Senior registrar, Department of neurosurgery, NMCH , Nellore , A.P., India.
E-mail: dr.suryapatap_singh_tomar@ yahoo.com
Abstract
in patients with depressed skull fractures, these fragments can be used to reconstruct the damaged facial architecture.The aim of the study was to test the feasibility of managing comminuted frontal bone depressed fracture by a single stage debridement, reduction and replacement of the bone fragments and soft tissue reconstruction. bone cranioplasty using the native fractured bones was prospectively done in 11 patients over a period of one year from January 2011 to December 2012. We report on our clinical cases and the surgical technique of managing comminuted frontal bone fractures. The posttraumatic frontal bone defect was caused by road traffic accident. There were no deaths due to the minimal complications from the procedure. Two patients (18%) had mild scalp infections, 1 patient (0.9%) had epileptic seizure, which was controlled by medication. It thus concluded that the fractured frontal bone can be reconstructed immediately with debridement in spite of major sinus involvement and underlying brain and dural damage. Factors contributing to success are removal of foreign debris from the fractured bone segments, perfect dural repair with the use of pericranial flaps and bone cover being provided from beneath by the pericranial flap and above the skin. These segments heal excellently with bone remodeling.
Keywords
Frontal bone fracture, Reconstruction, Single stage reconstruction
Introduction
Frontal bone fractures are most commonly encountered with facial injuries. The anatomy of frontal bone consisting of frontal sinus and their position in maxillofacial skeleton makes it more susceptible to injury. Craniofacial injuries involving the frontal bone can breach the duramater. CSF rhinorrhea, raised intracranial pressure, meningitis, meningial abscess are other known potential complications. Appropriate soft tissue and fracture management is important in overcoming these complications.
Our surgical management protocol was to reduce and replace the non vascularised fractured frontal bone segments with the soft tissue reconstruction in a single stage. The latter was achieved by a good repair of the scalp and repair of the dura with a pericranial flap. We expected the bone to heal and remodel itself.
The aim of the study was to test our abovementioned management protocol by reporting on the outcome of our clinical series. A clinical account of 2 classical cases out of 11 will be given.
Subjects and Methods
Eleven subjects were prospectively chosen from patients presenting to our trauma unit following a road traffic accident during the period January 2012 to December 2012.Their age range was 21 to 45 years. These patients were selected based on factors, which included the time of trauma, low Glasgow coma score, severity of fracture and need for emergency treatment due to cerebral edema or cerebral hematoma due to depressed frontal bone fractures.
Surgical Procedure
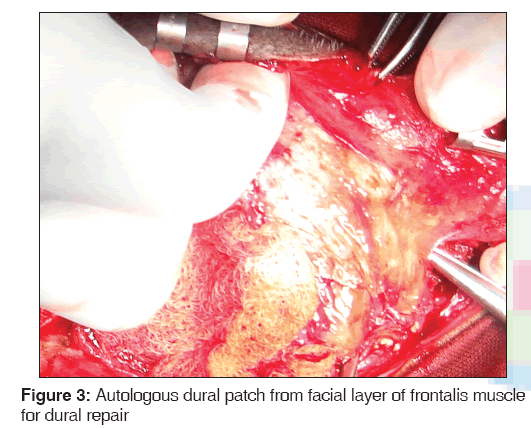
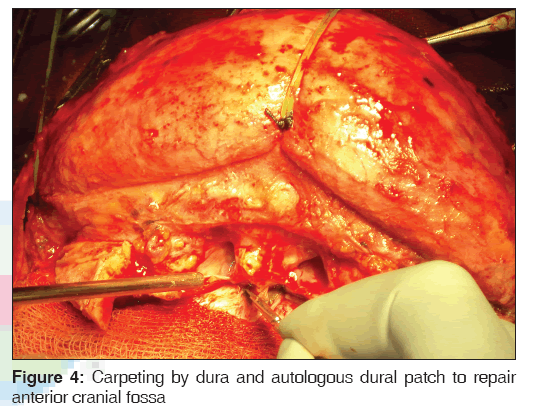
Bi-coronal scalp incision was made 3 cm behind the hairline for an inconspicuous scar. Sub-galeal dissection was done till the supraorbital rims. The fractured bone segments, which were more than 1 cm, were collected and immersed in povidine-iodine solution and smaller bone pieces were disposed off. Frontal lobe was retracted posteriorly. The frontal sinus was cranialized. Pedicled pericranial flap mimicking artificial duramater was dissected and sutured to the duramater of brain on all sides. This technique is called carpeting, which covers the frontal lobe within the anterior cranial fossa and provides a seal for the brain. Tight closure of the duramater and graft was done to prevent Cerebrospinal Fluid (CSF) leakage.
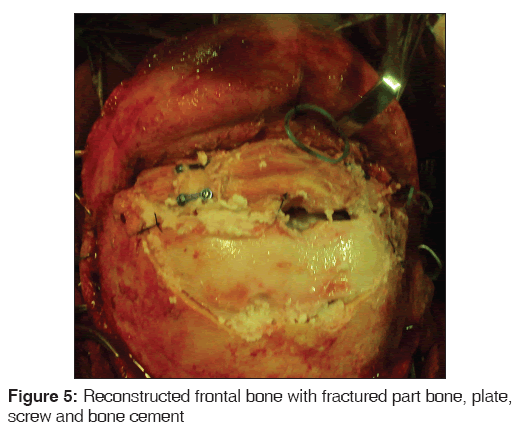
The fractured bone fragments were cleaned for debris and foreign bodies. Fractures with multiple small fragments were arranged over the pericranial flap in a mosaic pattern to cover much of the defect. In some cases it was necessary to reconstruct the contour of the frontal bone by placing strips of gel foam beneath the replaced fragments. In the event that the bone fragments were large and fewer in number the reduced bone was fixated with 2 × 2 mm holed stainless steel plates and 2 × 6 mm screws. Hydroxyapatite cement was added on the edges of the fractured segments to fill the gap between bone fragments. Scalp was closed in layers.
Case 1
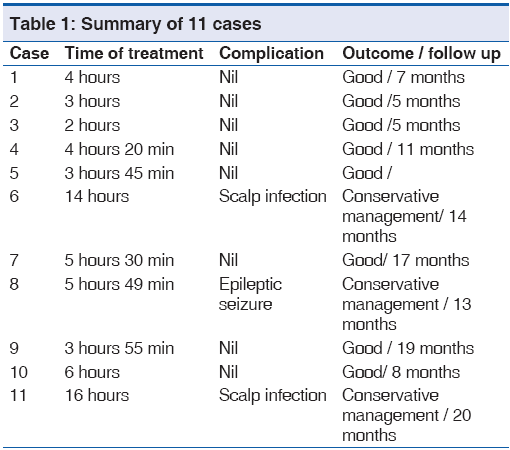
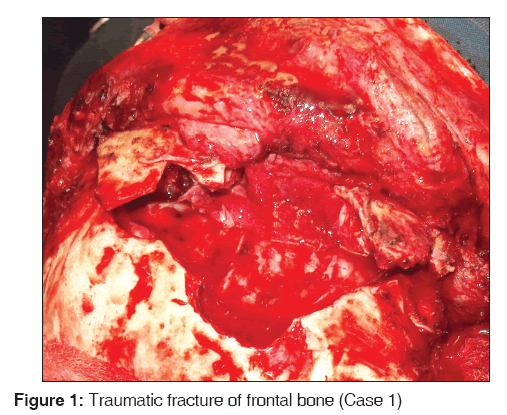
A 24 year old male presented within 4 hours following a road traffic accident. On clinical examination, he had multiple facial injuries with a depressed frontal bone fracture with cerebro-spinal fluid (CSF) rhinorrhea. Computed tomography of brain revealed comminuted fracture of frontal bone with disruption of naso-frontal junction and bilateral zygomatic complex fracture. The indication for surgery was a low Glasgow coma scale and associated depressed frontal bone fracture breaching the dura and extending to the brain. He was managed as per our surgical protocol as for multiple small comminuted fracture segments without the application of fixation. On follow up at 7 months the recovery was uneventful and free of complications [Figure 1].
Case 2
A 33 year old male presented within 3 hours following a road traffic accident. On clinical examination he had frontal depression with panfacial trauma. CT brain revealed depressed frontal bone, ethmoid bones fracture and multiple comminuted fractures of bilateral zygomatic bones and mandible with subdural hematoma. The indication for surgery was a low Glasgow coma scale, subdural hematoma and panfacial fractures. The frontal bone fracture was managed as per our surgical protocol with the large bone segments requiring reduction and fixation and intervening gaps were filled with hydroxyapatite cement. There was a mild postoperative infection of the scalp, which was controlled by antibiotics. On follow up at 5 months the recovery was uneventful and free of complications [Figure 2].
Results
Follow up period was from 5 to 20 months. Of the11 patients who were operated on, 2 patients (18%) had wound infection. Both had a delay in primary treatment from the time of trauma and had heavily contaminated wounds and mutilated tissues. Conservative treatment was successful in controlling the infection and no surgical intervention and/or removal of the replaced bone fragments was necessary. A single patient had epiletptic seizures in the postoperative period, which was controlled by parenteral phenytoin sodium given at a dose of 5-7 mg/kg. [Table 1]. There were no incidents of CSF rhinorrhea, otorrhea or deaths following the surgery.
Discussion
Management protocols for frontal fractures vary widely. Appropriate treatment depends on a correct diagnosis, physical examination and computed tomography scans analysis. Tradition favors thorough debridement of depressed frontal bone fractures with disposal of devitalized fractured bone segments. The resultant secondary frontal deformity requires correction by cranioplasty at a second stage [Figures 3 and 4].
MacEwenetal[1] in 1888 advocated the use of fractured bony segments which were soaked in bichloride of mercury which was confirmed by other authors recently with satisfactory results.[1-3]
Coleman et al.[4] and Suryapratap Singh[5] advocated replacement of the fractured segments to reconstruct the bone defect. His inclusion criteria was the time of injury to repair being less than 12 hours, the fracture being associated with a dural laceration or underlying severe injury to the brain.[4,5]
Rowbotham et al.[6] in 1964 suggested complete removal of depressed fragments when a large area of bone had been involved. However they recommended not elevating and devascularizing minimally displaced bone.[6] Autogenous grafts, either cancellous bone or calvarial bone grafts were preferred over alloplastic materials like methylmethacrylate and titanium mesh to reconstruct the residual defect.[7-9]
Jennett and Miller[3] studied 359 patients with compound depressed fractures. They overall infection rate for cases done more than 48 hours after injury was 36.5%.[6] This included preoperative infections. Our postoperative infection rate was 18%. Two patients making up this group were operated on after 13 hours following trauma and their wounds were badly mutilated and contaminated. The other 9 patients without a infection complication were operated within 6 hours of trauma.[3]
Braakman et al.[2] reported a low infection rate in his series of 225 patients who had immediate bone replacement, and reported only four cases of osteomyelitis.[2] Kriss, et al.[10] reported 2.5% infection rate in a series of 79 cases of autogenous fractured bone replacement.
Our clinical series and the literature review bears out the relative safety of reconstructing frontal bone defects with debrided and replaced fractured bone fragments. We feel that a robust dural repair is an important aspect of realizing this goal. On the other hand Jefferson and Reilly, who reviewed fractures of the anterior cranial fossa, allowed the duramater to heal itself. Failures in healing can occur in the presence of underlying brain damage. Adherence of the cerebral tissue to dural edges prevents complete closure and the resulting CSF leak has an associated morbidity and mortality.[11]
Our use of hydroxyapatite for residual bone defects was reasonable and avoided harvest from a donor site. Shehadi has shown in trephined dogs that bone dust spread on the dural surface will form a sheet of bone.[10] Hydroxyapatite cements help to form a sheet of bone segments and promote excellent bone healing [Figure 5].[12,13]
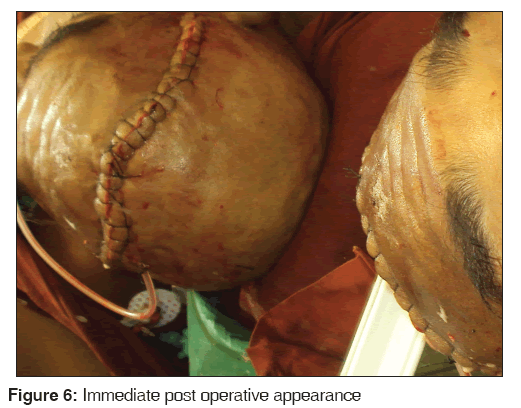
In our cases we posit that the replaced bone fragments remained vital and were revascularised from the pedicled pericranium flap and the overlying skin cover. With time the bone went on to heal and remodel [Figure 6]. Experimental work by Stringa et al.[14] in 1957 has shown a striking correlation between the rate of vascular penetration into a bone implant and its ability to survive.[14] Blood vessels penetrate cancellous bone much more readily than cortical or cranial bone because the cortex presents a physical impediment to vascular invasion. Alternatively fragments serve as a scaffold for connective tissue and osteoblastic proliferation. New bone formation may occur from underlying pericranial flaps and duramater or adjacent bone edges.
Conclusion
A team approach consisting of maxillofacial surgeon and Neurosurgeon is mandatory. A single stage reconstruction of the frontal bone fracture performed immediately is feasible if combined with adequate debridement and appropriate soft tissue lining and cover. The stigma of facial deformity associated with a multi-staged approach can thus be avoided. We admit that our series is small but our technique is cost effective, shortens operation time and has good aesthetic results with no donor site morbidity. A long term study with large number of patients will serve to further validate our results.
Source of Support
Nil
Conflict of Interest
None declared.
References
- Macewen W. An Address on the Surgery of the Brain and Spinal Cord. Br Med J 1888;2:302-9.
- Braakman R. Depressed skull fracture: Data, treatment, and follow-up in 225 consecutive cases. J Neurol Neurosurg Psychiatry 1972;35:395-402.
- Jennett B, Miller JD. Infection after depressed fracture of skull. Implications for management of nonmissile injuries. J Neurosurg 1972;36:333-9.
- Coleman CC. Treatment of compound fractures of the skull. Ann Surg 1942;115:507-13.
- Singh S. An unusual case of a compound depressed skull fracture. J Surg Pak 2009;14:184-6.
- Rowbotham GF. Acute Injuries of the Head: Their Diagnosis. Treatment. Complications and Sequels. 4th ed. London, England; E & S Li vingstone; 1964.
- Hendus J, Draf W, Bockmühl U. Reconstruction of the frontoorbital frame using split-thickness calvarial bone grafts. Laryngorhinootologie 2005;84:899-904.
- Mottaran R, Guarda-Nardini L, Fusetti S, Ferroneto G, Salar G. Reconstruction of a large post-traumatic cranial defect with a customized titanium plaque. J Neurosurg Sci 2004;48:143-7.
- Tuusa SM, Peltola MJ, Tirri T, Lassila LV, Vallittu PK. Frontal bone defect repair with experimental glass-fiber-reinforced composite with bioactive glass granule coating. J Biomed Mater Res B Appl Biomater 2007;82:149-55.
- Kriss FC, Taren JA, Kahn EA. Primary repair of compound skull fractures by replacement of bone fragments. J Neurosurg 1969;30:698-702.
- Jefferson A, Reilly G. Fractures of the floor of the anterior cranial fossa. The selection of patients for dural repair. Br J Surg 1972;59:585-92.
- Chen TM, Wang HJ, Chen SL, Lin FH. Reconstruction of post-traumatic frontal-bone depression using hydroxyapatite cement. Ann Plast Surg 2004;52:303-8.
- Shehadi SI. Skull reconstruction with bone dust. Br J Plast Surg 1970;23:227-34.
- Stringa G. Studies of the vascularisation of bone grafts. J Bone Joint Surg Br 1957;39-B:395-420.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.