Factors Influencing Prevalence of Hypertension among Healthcare Workers in Korle-Bu Polyclinic in the Accra Metropolis, Ghana
2 Department of Pathology, University of Ghana Medical School, Accra, Ghana
3 Department of Medical Laboratory Science, KAAF University College, Accra, Ghana
4 Department of Medical Laboratory Science, University of Cape Coast, Cape Coast, Ghana
Received: 27-Sep-2024, Manuscript No. amhsr-24-152749; Editor assigned: 30-Sep-2024, Pre QC No. amhsr-24-152749 (PQ); Reviewed: 14-Oct-2024 QC No. amhsr-24-152749; Revised: 14-Oct-2024, Manuscript No. amhsr-24-152749 (R); Published: 31-Oct-2024
Citation: Botchway FA, et al. Factors Influencing Prevalence of Hypertension among Healthcare Workers in Korle-Bu Polyclinic in the Accra Metropolis, Ghana. Ann Med Health Sci Res. 2024;14:1068-1074.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Hypertension, a chronic condition characterized by elevated blood pressure, poses a global public health challenge. Healthcare workers, due to demanding work schedules, shift work and exposure to stressful environments, are considered a population at increased risk for this condition. At the Korle Bu Polyclinic, healthcare workers are exposed to significant stressrelated risk factors like workload, long shift hours, etc. In this light, this study sought to assess the factors influencing the prevalence of hypertension among healthcare workers in the Korle-Bu Polyclinic.
Methods: A hospital-based cross-sectional study design to gather data from a total of 160 Healthcare workers. Participants' responses were encoded for analysis using Statistical Package for the Social Sciences (SPSS). Mean and standard deviations were used to describe the continuous variables and percentages to describe categorical variables. Binary logistic regression was used to examine the factors associated with hypertension.
Results: The results showed that 28.8% were identified as hypertensive. The analysis of determinants of hypertension among healthcare workers at the Korle Bu Polyclinic revealed age as a significant predictor of hypertension.
Conclusion: The findings supports the critical role of socio-economic factors in shaping health outcomes among healthcare workers. The study recommends that the Korle Bu Polyclinic and other healthcare facilities implement comprehensive wellness programs targeting hypertension prevention and management among healthcare workers.
Keywords
Hypertension; Healthcare workers; World Health Organisation (WHO); Ghana Demographic and Health Survey (GDHS)
Introduction
Hypertension also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated [1]. High blood pressure typically does not cause symptoms; long-term high blood pressure, however, is a major risk factor for coronary artery disease, stroke, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease and dementia [2-4].
The modern lifestyle, characterized by sedentary habits, poor dietary choices, stress and obesity, significantly contributes to the prevalence of hypertension. For instance, as found by, high sodium intake, commonly found in processed foods, disrupts fluid balance and leads to increased blood pressure. Lack of physical activity weakens the cardiovascular system, exacerbating hypertension [5]. Stress, both chronic and acute, triggers physiological responses that elevate blood pressure over time [6].
An estimated 1.28 billion adults aged 30–79 years worldwide have hypertension, most (two-thirds) living in low and middleincome countries [7]. The World Health Organisation (WHO) estimates that 7.5 million people die from hypertension-related diseases worldwide. It is the most significant risk factor for cardiovascular-related deaths and morbidity worldwide. The prevalence of hypertension varies across regions and country income groups. The African region has the highest prevalence of hypertension (27%) [8]. In Ghana, hypertension continues to be a major cause of death. In 2014, the Ghana Demographic and Health Survey (GDHS) found that 13% of adults had hypertension, 40.5% were receiving medication and only 23.8% had their condition under control [9,10].
A group of Ghanaian physicians and public health professionals developed the May Measurement Month (MMM) initiative to promote early detection of hypertension and adequate therapy to avoid consequences. The World Hypertension League (WHL) and the International Society of Hypertension (ISH) are leading the May Measurement Month campaign, which aims to test 1% of the population in each participating nation for hypertension [11].
During the global MMM campaign in 2018 and 2019, the prevalence of hypertension among participants was 33.4% and 34%, respectively [12,13]. In 2018, 6907 individuals in Ghana underwent screening for hypertension, with a 34.1% prevalence [14].
Healthcare workers are exposed to significant stress-related risk factors such as working overtime, high workload, time-intensive pressures, difficult or complex tasks, inadequate breaks, monotony and poor physical conditions. In addition, during the treatment procedures, they are exposed to various hardships such as long periods on their feet, insomnia during night shifts and dietary irregularities, depending on their workload [15]. Also, the psychological and emotional toll of caring for patients, encountering critical situations and making high-stakes decisions can contribute to chronic stress, further exacerbating the risk of hypertension among healthcare professionals [16].
At the Korle Bu Polyclinic, Healthcare Workers (HCWs) are exposed to significant stress-related risk factors such as working overtime, high workload, time-intensive pressures, difficult or complex tasks, inadequate breaks, monotony and poor physical conditions [17]. Many healthcare professionals, especially nurses and physicians, work irregular shifts that can disrupt their natural sleep patterns and circadian rhythms. This disruption has been associated with an increased risk of hypertension and other cardiovascular problems [18].
Hypertension can impair cognitive function, decrease work productivity and lead to absenteeism, potentially compromising the overall effectiveness of healthcare delivery [19]. Consequently, the health status of healthcare professionals can significantly influence the quality of patient care. Identifying modifiable risk factors associated with hypertension in healthcare professionals can lead to targeted interventions. Implementing preventive measures such as lifestyle modifications, stress management programs and regular health screenings could effectively reduce the burden of hypertension in this vulnerable population.
In line with the goal of the Ghana Health Service, Non- Communicable Disease Control Programme to strengthen early detection and management of non-communicable diseases to reduce morbidity and mortality, the current reserach sought to assess the prevalence and associated factors of hypertension among HCWs in the Korle Bu Polyclinic.
Materials and Methods
Study design
A hospital-based cross-sectional study was conducted at the Korle-Bu Polyclinic in the Accra Metropolis of Ghana. Korle- Bu Polyclinic is one of the sub-BMCs of the Korle Bu Teaching Hospital (KBTH). Its primary purpose was to act as a facility for the delivery of services within the catchment region. Since 2000, it has been accredited as a training center for family physicians by the Colleges of Physicians in both Ghana and West Africa. Korle Bu Polyclinic is the primary care provider of Korle Bu Teaching Hospital. For several decades the polyclinic has provided services to numerous clients, as well as to KBTH staff and their dependants.
Study population
A convenient sampling procedure was used to sample medical professionals working at the Korle-Bu Polyclinic.
Inclusion criteria
This study included all clinical, administrative, paramedical and public health practitioners who are either permanent or temporary staff.
Exclusion criteria
The study excluded staff who were on annual leave, pregnant women and staff with clinically diagnosed chronic conditions at the time of participant recruitment.
Sample size
The total population sampling was utilized. Based on the information provided by the facility's Human Resource Department, the total number of employees working at the facility as of December, 2023 was 169. A total of 160 of these individuals met the requirements to be included in the study. The sample size for this study was set at 160 individuals from the population and the margin of error was established at 5%.
Data collection tools and techniques
A nurse, a dietitian and a physician who also prescribes medications were all recruited to work as research assistants. At recruitment, a pre-tested questionnaire was used to collect data on participants’ socio-demographic, lifestyle and clinical characteristics. Information regarding the respondents' demographics such as age, sex, marital status, job position and years of experience in the healthcare industry were obtained. Information on participants’ medical history, which included any pre-existing health conditions, previous diagnoses of hypertension and diabetes, as well as any other co-morbid were collected. Data on socioeconomic characteristics including occupation, income level, access to healthcare services and education level were also collected. Information concerning institutional factors such as stress related to work, shift patterns and support systems was also obtained.
Anthropometric measurements
A standard stadiometer was attached to a calibrated weighing scale to collect data on respondents' height and weight. Weights and heights were measured with the participants standing in an upright position with their backs and heels against the stadiometer, facing forward with their hands hanging loosely by their sides and wearing light clothing without any footwear. Weight and height measurements were recorded in Kilograms (kg) and Centimeters (cm), respectively, with the nearest centimeter being used for the latter.
To determine the Body Mass Index (BMI), the weight in Kilograms (kg) was divided by the squared height in meters (m2). According to the World Health Organization's standard definitions, the subjects were classified into three categories based on their Body Mass Index (BMI): Normal weight (BMI<25 kg/m2), overweight (25 ≤ BMI<30 kg/ m2) and obese (BMI ≥ 30 kg/m2).
The measurements of the individual's blood pressure were taken with a digital monitor (Omron TM Blood Pressure Monitor) while wearing a sleeve that was an appropriate size for the individual's arm circumference. Measurements of the participants' systolic and diastolic blood pressure were taken twice on the right arm of the participants and the arithmetic mean of these two measurements was recorded. This was done after patients had rested for at least 15 minutes per the recommendations of the American Heart Association [20]. Those who participated in the study were deemed to have hypertension if they had a systolic blood pressure of at least 140 mmHg and/ or diastolic blood pressure of at least 90 mmHg and if they had a previous history of hypertension.
Data analysis
The data were first entered into Microsoft Excel and then exported to Statistical Packages for Social Science version 18.0 (SPSS Inc., USA) for analysis. Categorical variables were presented as percentages and analyzed using the Chi-squared test. Multivariate logistic regression analyses were adopted to identify factors associated with depressive symptoms among participants. All variables from the univariate analysis with a p-value <0.2 were entered into a forward-stepwise multivariate logistic regression analysis. A test was two-tailed and statistically significant set at 0.05 with a 95% confidence level.
Results
Demographic characteristics of the participants
Table 1 shows the distribution of demographic characteristics of participants. The largest proportion of respondents fell within the age range of 23 years-40 years, constituting 63.8% of the surveyed population. The data revealed a predominance of female representation, comprising 55.0% of the surveyed population and males representing 45%. Medical staff constituted the majority, representing 61.9% of the surveyed population, while non-medical/administrative staff accounted for the remaining 38.1%.
| Frequency (N) | Percentage (%) | ||
|---|---|---|---|
| Age | |||
| 23-31 years | 48 | 30 | |
| 32-40 years | 54 | 33.8 | |
| 41-49 years | 30 | 18.8 | |
| 50 years and above | 28 | 17.5 | |
| Sex | |||
| Male | 72 | 45 | |
| Female | 88 | 55 | |
| Job position | |||
| Medical staff | 99 | 61.9 | |
| Non-medical/Administrative staff | 61 | 38.1 | |
Table 1: Demographic characteristics of the participants.
Blood pressure and BMI of HCWs
Table 2 shows the distribution of blood pressure and BMI of Healthcare Workers (HCWs. The mean systolic blood pressure was 122.11 mmHg, with a standard deviation of 15.205 mmHg. Meanwhile, the mean diastolic blood pressure was 81.14 mmHg, with a standard deviation of 9.475 mmHg. The mean Body Mass Index (BMI) of the HCWs was 25.90 kg/m2, with a standard deviation of 4.908 kg/m2.
| Mean | Std. Deviation | |
|---|---|---|
| Systolic (mmHg) | 122.11 | 15.205 |
| Diastolic (mmHg) | 81.14 | 9.475 |
| BMI (kg/m2) | 25.9 | 4.908 |
Note: BMI- Body Mass Index, HCWs-Healthcare Workers
Table 2: Blood pressure of HCWs.
Distribution of BMI and hypertensive status among HCWs
Table 3 shows the distribution of Body Mass Index (BMI) and hypertensive status among HCWs. Among the participants, 43.8% were identified as having a normal weight, while 33.1% were overweight and 23.1% were obese. Out of the 160 participants sampled, 46 (28.8%) were classified as hypertensive.
| Frequency (N) | Percent (%) | |
|---|---|---|
| BMI | ||
| Normal weight | 70 | 43.75 |
| Over weight | 53 | 33.125 |
| Obese | 37 | 23.125 |
| Hypertension status | ||
| Hypertensive | 46 | 28.75 |
| Not hypertensive | 114 | 71.25 |
Note: BMI-Body Mass Index
Table 3: Distribution of BMI and hypertensive status among HCWs.
Prevalence rate of hypertension among HCWs
Table 4 shows the distribution of the prevalence rate of hypertension among HCWs. Among medical staff, 21 out of 99 individuals (21.2%) were hypertensive, while among nonmedical/ administrative staff, 25 out of 61 individuals (41.0%) were hypertensive. 18 out of 72 male participants (25.0%) were hypertensive, while among females, 28 out of 88 individuals (31.8%) were hypertensive. Those with a family history of hypertension demonstrated a higher prevalence of hypertension (41.0%) compared to those without such a history (24.8%). Among shift workers, 32 out of 118 individuals (27.1%) were hypertensive, while among non-shift workers, 14 out of 42 individuals (33.3%) were hypertensive. Among healthcare workers (HCWs), the distribution of hypertensive individuals varies significantly based on their Body Mass Index (BMI). Among those with normal weight, only 7.1% were hypertensive, while 24.5% of overweight individuals and a striking 75.7% of obese individuals suffered from hypertension. This disparity supports a significant association between BMI and systolic hypertension (p=0.000), highlighting the critical role of weight management in combating hypertension among HCWs.
| Variables | Categories | Systolic | p-value | |
|---|---|---|---|---|
| Hypertensive | Not Hypertensive | |||
| Salary/income | < GhË 2000.00 | 13(52.0) | 12(48.0) | 0.007 |
| Above GhË 2000.00 | 33(24.4) | 102(75.6) | 0.001 | |
| Age | Less than 40 years | 20(19.6) | 82(80.4) | |
| More than 40 years | 26(44.8) | 32(55.2) | 0.22 | |
| Sex | Male | 18(25.0) | 54(75.0) | |
| Female | 28(31.8) | 60(68.2) | 0.006 | |
| Profession | Medical staff | 21(21.2) | 78(78.8) | |
| Non-Medical/Administrative staff | 25(41.0) | 36(59.0) | 0.283 | |
| Shift worker | Yes | 32(27.1) | 86(72.9) | |
| No | 14(33.3) | 28(66.7) | ||
| BMI | Normal weight | 5(7.1) | 65(92.9) | 0 |
| Over weight | 13(24.5) | 40(75.5) | ||
| Obese | 28(75.7) | 9(24.3) | ||
Note: BMI-Body Mass Index, HCWs-Healthcare Workers
Table 4: Prevalence rate of hypertension among HCWs.
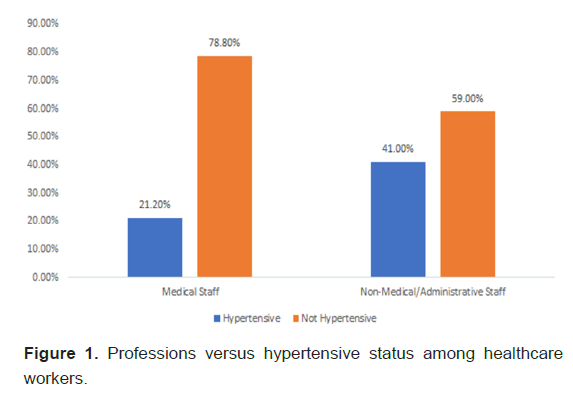
Professions versus hypertensive status among healthcare workers
21 out of 99 (21.2%) medical staff were hypertensive, while 25 out of 61 (41.0%) non-medical/administrative staff were hypertensive (Figure 1).
Factors influencing prevalence of hypertension among HCWs
Table 5 shows the distribution of factors influencing the prevalence of hypertension among HCWs. Age emerged as a predictor of hypertension among HCWs. Participants older than 40 years had 3 times increased odds of being hypertensive compared to their younger counterparts (OR=3.221, 95% CI:1.530 - 6.77).
| B | Wald | Sig. | Exp (B) | 95% C.I. for EXP (B) | 95% C.I. for EXP (B) | |
|---|---|---|---|---|---|---|
| (Lower) | (Upper) | |||||
| Sex (Male) | 0.538 | 1.909 | 0.167 | 1.713 | 0.798 | 3.675 |
| Alcohol intake (Yes) | -0.574 | 1.42 | 0.233 | 0.563 | 0.219 | 1.448 |
| Physical (Yes) | 0.098 | 0.045 | 0.832 | 1.102 | 0.448 | 2.715 |
| Age (<40 years | 1.17 | 9.487 | 0.002 | 3.221 | 1.53 | 6.779 |
| Constant | 0.417 | 0.607 | 0.436 | 1.517 | _ | _ |
Note: C.I.=Confidence Interval; Exponentiated Coefficients (EXP)
Table 5: Factors Influencing Prevalence of Hypertension among HCWs.
Institutional factors influencing prevalence of hypertension among HCWs
Table 6 shows the distribution of institutional factors influencing the prevalence of hypertension among HCWs. Participants who were medical staff had 4.051 higher odds of developing hypertension compared to non-medical staff (OR=4.051, 95% CI:1.600-10.258). The number of years on shift duty was a significant predictor of hypertension risk among HCWs (p-value=0.002).
| B | Wald | Sig. | Exp (B) | 95% C.I. for EXP (B) | 95% C.I. for EXP (B) | |
|---|---|---|---|---|---|---|
| (Lower) | (Upper) | |||||
| Shift/duty | -0.714 | 1.874 | 0.171 | 0.49 | 0.176 | 1.361 |
| Shift (Yes) | -0.135 | 10.033 | 0.002 | 0.873 | 0.803 | 0.95 |
| Profession (Medical staff) | 1.399 | 8.709 | 0.003 | 4.051 | 1.6 | 10.258 |
| Constant | 1.522 | 10.9 | 0.001 | 4.58 | _ | _ |
Note: C.I.=Confidence Interval; Exponentiated Coefficients (EXP)
Table 6: Institutional Factors Influencing Prevalence of Hypertension among HCWs.
Table 7 shows the distribution of socio-economic factors influencing the prevalence of hypertension among HCWs. Individuals with salaries below GhS 2000.00 have approximately one-third the odds of being hypertensive relative to those with salaries above GhS 2000.00 (OR=0.299, 95% CI:0.124-0.718).
| B | Wald | Sig. | Exp (B) | 95% C.I. for EXP(B) | 95% C.I. for EXP(B) | |
|---|---|---|---|---|---|---|
| (Lower) | (Upper) | |||||
| Income/Salary | -1.209 | 7.289 | 0.007 | 0.299 | 0.124 | 0.718 |
| Constant | 1.128 | 31.751 | 0 | 3.091 | _ | _ |
Note: C.I.=Confidence Interval; Exponentiated Coefficients (EXP)
Table 7: Socio-economic factors influencing prevalence of hypertension among HCWs.
Discussion
Hypertension, a chronic condition characterized by elevated blood pressure, poses a significant public health challenge globally. Healthcare Workers (HCWs), due to demanding work schedules, shift work and exposure to stressful environments, are considered a population at increased risk for this condition. This study investigated the risk factors influencing the prevalence of hypertension among HCWs at the Korle Bu Polyclinic in Ghana, offering valuable insights while raising intriguing points for discussion in comparison to previous literature.
The study identified a 28.8% prevalence of hypertension among surveyed HCWs, which stood notably lower than the national average of 30.3% for Ghanaian adults [21]. This seemingly positive finding, however, requires cautious interpretation. While a lower prevalence compared to the general population might suggest a relatively healthier workforce, it was important to acknowledge that even 28.8% signifies a concerning number of affected HCWs, underlining the need for continued vigilance and preventive measures.
One intriguing finding was the observed higher prevalence of hypertension among non-medical/administrative staff (54.3%) compared to medical staff (45.7%). This contradicted several studies demonstrating a higher prevalence among healthcare professionals due to work-related stress [22,23]. While administrative roles might generally involve lower physical demands, they could entail distinct stressors related to workload, deadlines and interpersonal interactions within the healthcare setting.
The study aligned with previous findings by revealing a higher prevalence of hypertension among female HCWs (60.9%) compared to their male counterparts (39.1%) [24]. While biological factors undoubtedly contributed to this disparity, it was imperative to delve deeper into socio-economic and work-life balance challenges that disproportionately impacted women in healthcare settings. Gender expectations, childcare responsibilities and potential workplace discrimination could intertwine with biological factors to exacerbate the risk for female HCWs.
The findings from this study did not show any significant association between alcohol intake, frequency of physical activity and hypertension risk among HCWs. However, the role of occupational factors and sedentary lifestyles in hypertension incidence cannot be overlooked. Akinwale and George emphasized the adverse health effects of prolonged and sedentary work hours, suggesting a potential link to hypertension development among HCWs [25,26]. Moreover, Rike, et al., featured the heightened hypertension risk among professions characterized by prolonged sitting and limited physical activity, such as truck drivers. These findings supported the importance of promoting active lifestyles and ergonomic work environments to reduce hypertension risk among HCWs.
The findings of this research featured the significance of age as a compelling predictor of hypertension among Healthcare Workers (HCWs). Our study showed a significant association between age and hypertension among healthcare workers. This observation is similar to previously reported findings, where advancing age consistently emerges as a prominent risk factor for hypertension [27,28].
Notably, the study showed a significant inverse association between salary and the likelihood of hypertension, with individuals earning lower incomes exhibiting reduced odds of being hypertensive compared to their higher-earning counterparts. The observed association between income and hypertension prevalence aligned with previous literature highlighting the impact of socioeconomic disparities on health outcomes among healthcare workers. Addo, Smeeth emphasized the existence of income disparities within the healthcare sector, with support staff often facing lower incomes compared to highly specialized professionals [27]. These disparities contributed to financial strain, limiting access to healthy food, recreational facilities and preventive healthcare services, all of which are known risk factors for hypertension. Thus, the findings of the current study supported the importance of addressing income disparities and promoting financial equity within healthcare settings to reduce the burden of hypertension among healthcare workers.
Contrary to expectations, a family history of hypertension did not significantly predict hypertension among HCWs in the current analysis. This finding is in accordance with the findings from a study conducted in Nigeria by Egbi, Rotifa [28]. However, existing literature offers insights into the impact of family history on hypertension risk [29]. Studies by Nobahar, et al., and Bosu featured the positive association between a family history of hypertension and hypertension incidence, suggesting a potential genetic predisposition among affected individuals [30,31].
Conclusion
The results featured the significance of addressing the risk factors associated with the prevalence of hypertension among Healthcare Workers (HCWs) at the Korle Bu Polyclinic and the potential impact on the health of the workforce and the delivery of healthcare services. The observed patterns supported the need for targeted interventions and health promotion strategies to reduce hypertension risk among HCWs, particularly addressing gender-specific disparities, socio-economic inequalities and age-related risks. This study emphasized the significance of age as a key determinant of hypertension among HCWs, aligning with previous literature highlighting the strong association between advancing age and hypertension risk. However, there was insignificant association with alcohol intake, physical activity, gender and family history of hypertension suggesting that other factors may influence hypertension risk among HCWs at the Korle Bu Polyclinic.
It is recommended that the Korle Bu Polyclinic management implements comprehensive wellness programs targeting hypertension prevention and management among HCWs. These programs should incorporate education on lifestyle modifications, stress management techniques and regular health screenings. By prioritizing the health and well-being of HCWs, healthcare facilities can promote a supportive environment conducive to optimal patient care and staff productivity.
Limitations
The study design does not establish causality between some institutional factors and hypertension. The non-probability sampling technique used in this investigation is prone to selection bias. The study only included employees who were available for the screening process, thus it might not have been a complete picture of the whole population. It is possible that bias was introduced into the data collected for this study because it relied on self-reporting by healthcare workers themselves. However, despite these limitations, the findings of this study remain valid.
Ethical Committee Consent
Ethical clearance was obtained from the Ethical and Protocol Review Committee of the College of Health Sciences, University of Ghana Medical School, Korle-Bu, Accra and consent was also sought from each participant of the study. Ethics identification number: (CHS-Et/M.7-P/2023-2024).
Authors’ Contributions
FAB perceived the study. Felix Abekah Botchway and Prince Agyeman developed the methods for investigation. Prince Agyeman and Felix Abekah Botchway were involved in data collection and analysis. All authors were involved in the development of the manuscript for submission.
References
- Balwan WK, Kour S. A systematic review of hypertension and stress-the silent killers. Sch Acad J Biosci. 2021;6:150-4.
- Siu AL, US Preventive Services Task Force. Screening for high blood pressure in adults: US Preventive Services Task Force recommendation statement. Annals of internal medicine. 2015;163:778-86.
[Crossref] [Google Scholar] [PubMed]
- Pérez de Isla L, Alonso R, Mata N, Saltijeral A, Muñiz O, et al. Coronary heart disease, peripheral arterial disease and stroke in familial hypercholesterolaemia: Insights from the SAFEHEART Registry (Spanish Familial Hypercholesterolaemia Cohort Study). Arterioscler Thromb Vasc Biol. 2016;36:2004-10.
[Crossref] [Google Scholar] [PubMed]
- Olesen JB, Lip GY, Lane DA, Køber L, Hansen ML, et al. Vascular disease and stroke risk in atrial fibrillation: A nationwide cohort study. The American journal of medicine. 2012;125:826-e13.
[Crossref] [Google Scholar] [PubMed]
- DeGuire, J, Clarke J, Rouleau K, Roy J, Bushnik T. Blood pressure and hypertension. Health Rep; 2019. 30:14-21.
- Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. The Lancet. 2008;371:1513-8.
[Crossref] [Google Scholar] [PubMed]
- Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nature Reviews Nephrology. 2020;16:223-37.
[Crossref] [Google Scholar] [PubMed]
- Bromfield S, Muntner P. High blood pressure: The leading global burden of disease risk factor and the need for worldwide prevention programs. Current hypertension reports. 2013;15:134-6.
[Crossref] [Google Scholar] [PubMed]
- Bosu WK. Epidemic of hypertension in Ghana: A systematic review. BMC public health. 2010 Dec;10:1-4..
[Crossref] [Google Scholar] [PubMed]
- Sanuade OA, Boatemaa S, Kushitor MK. Hypertension prevalence, awareness, treatment and control in Ghanaian population: Evidence from the Ghana demographic and health survey. PloS one. 2018 ;13:e0205985.
[Crossref] [Google Scholar] [PubMed]
- Tannor EK, Nyarko OO, Adu-Boakye Y, Owusu Konadu S, Opoku G, et al. Prevalence of hypertension in Ghana: Analysis of an awareness and screening campaign in 2019. Clinical Medicine Insights: Cardiology. 2022;16:11795468221120092.
[Crossref] [Google Scholar] [PubMed]
- Beaney T, Burrell LM, Castillo RR, Charchar FJ, Cro S, et al. May Measurement Month 2018: A pragmatic global screening campaign to raise awareness of blood pressure by the International Society of Hypertension. European heart journal. 2019;40:2006-17.
[Crossref] [Google Scholar] [PubMed]
- Beaney T, Schutte AE, Stergiou GS, Borghi C, Burger D, et al. May Measurement Month 2019: The global blood pressure screening campaign of the International Society of Hypertension. Hypertension. 2020;76:333-41.
[Crossref] [Google Scholar] [PubMed]
- Twumasi-Ankrah B, Myers-Hansen GA, Adu-Boakye Y, Tannor EK, Nyarko OO, et al. May Measurement Month (MMM) 2018: An analysis of blood pressure screening results from Ghana. European Heart Journal Supplements. 2020;22:H59-61.
[Crossref] [Google Scholar] [PubMed]
- Oparil S, Acelajado MC, Bakris GL, Berlowitz DR, Cífková R, et al. Hypertension. Nature reviews. Disease primers. 2018;4:18014.
- Thomopoulos C, Parati G, Zanchetti A. Effects of blood-pressure-lowering treatment on outcome incidence in hypertension: 10–Should blood pressure management differ in hypertensive patients with and without diabetes mellitus? Overview and meta-analyses of randomized trials. Journal of hypertension. 2017 ;35:922-44.
[Crossref] [Google Scholar] [PubMed]
- Kjeldsen SE. Hypertension and cardiovascular risk: General aspects. Pharmacological research. 2018 Mar 1;129:95-9.
[Crossref] [Google Scholar] [PubMed]
- Ljevak I, Vasilj I, Lesko J, Neuberg M, Perić O, et al. Utjecaj smjenskog rada na metabolizam i cjelodnevni ritam kod medicinskih sestara i tehničara. Acta clinica Croatica. 2021;60:476-82.
- Forte G, De Pascalis V, Favieri F, Casagrande M. Effects of blood pressure on cognitive performance: A systematic review. Journal of clinical medicine. 2019;9:34.
[Crossref] [Google Scholar] [PubMed]
- Kirkendall WM, Burton AC, Epstein FH, Freis ED. Recommendations for human blood pressure determination by sphygmomanometers. Circulation. 1967;36:980-8.
[Crossref] [Google Scholar] [PubMed]
- Asante DO, Walker AN, Seidu TA, Kpogo SA, Zou J. Hypertension and diabetes in Akatsi South District, Ghana: Modeling and forecasting. BioMed Research International. 2022;2022:9690964.
[Crossref] [Google Scholar] [PubMed]
- Prabhakaran D, Jeemon P, Ghosh S, Shivashankar R, Ajay VS, et al. Prevalence and incidence of hypertension: Results from a representative cohort of over 16,000 adults in three cities of South Asia. Indian heart journal. 2017;69:434-41.
[Crossref] [Google Scholar] [PubMed]
- Piper MA, Evans CV, Burda BU, Margolis KL, O’Connor E, et al. Screening for high blood pressure in adults: A systematic evidence review for the US Preventive Services Task Force. 2015.
[Google Scholar] [PubMed]
- Mohammed Nawi A, Mohammad Z, Jetly K, Abd Razak MA, Ramli NS, et al. The prevalence and risk factors of hypertension among the urban population in Southeast Asian countries: A systematic review and meta‐analysis. International journal of hypertension. 2021;2021:6657003.
[Crossref] [Google Scholar] [PubMed]
- Akinwale OE, George OJ. Work environment and job satisfaction among nurses in government tertiary hospitals in Nigeria. Rajagiri Management Journal. 2020;14:71-92.
- Rike ME, Diress M, Dagnew B, Getnet M, Hasano Kebalo A, et al. Hypertension and its associated factors among long-distance truck drivers in Ethiopia. Integrated Blood Pressure Control. 2022;21:67-79.
[Crossref] [Google Scholar] [PubMed]
- Anteneh ZA, Yalew WA, Abitew DB. Prevalence and correlation of hypertension among adult population in Bahir Dar city, northwest Ethiopia: A community based cross-sectional study. International journal of general medicine. 2015:175-85.
[Crossref] [Google Scholar] [PubMed]
- Egbi OG, Rotifa S, Jumbo J. Prevalence of hypertension and its correlates among employees of a tertiary hospital in Yenagoa, Nigeria. Annals of African medicine. 2015;14:8-17.
[Crossref] [Google Scholar] [PubMed]
- Addo J, Smeeth L, Leon DA. Socioeconomic position and hypertension: A study of urban civil servants in Ghana. Journal of Epidemiology and Community Health. 2009;63:646-50.
[Crossref] [Google Scholar] [PubMed]
- Nobahar M, Razavi MR. Lifestyle and the most important risk factors of cardiovascular disease in physicians, nurses and faculty members. Middle East Journal of Rehabilitation and Health. 2015;2.
- Bosu WK. Determinants of mean blood pressure and hypertension among workers in West Africa. International journal of hypertension. 2016;2016:3192149.
[Crossref] [Google Scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.