Female Genital Mutilation: Description and Prevalence of Obstetric and Neonatal Complications
2 Department of Physical Medicine and Rehabilitation, University of Kinshasa, Kinshasa, Democratic Republic of the Congo, Congo
3 Department of Functional Anatomy, University Libre de Bruxelles, Brussels, Belgium
Received: 15-Nov-2022, Manuscript No. AMHSR-22-79880; Editor assigned: 17-Nov-2022, Pre QC No. AMHSR-22-79880 (PQ); Reviewed: 01-Dec-2022 QC No. AMHSR-22-79880; Revised: 25-Mar-2023, Manuscript No. AMHSR-22-79880 (R); Published: 01-Apr-2023
Citation: Bertuit J, et al. Female Genital Mutilation: Description and Prevalence of Obstetric and Neonatal Complications. A Review of the literature. Ann Med Health Sci Res. 2023;13:520-529.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Female genital mutilation is not without consequences, varying according to the type and severity includes complications of pregnancy and childbirth.
Objective: The objective of this systematic review of literature is to assess the prevalence of obstetric and neonatal complications in women with genital mutilation compared to women without genital mutilation.
Method: Literature searches carried out on three scienti ic databases (CINAHL, Science direct and PubMed) selected observational studies published from 2010 to 2021 assessing prolonged of second phase of labour, vaginal outlet obstruction, emergency cesarean section, perineal tear, instrumental births, episiotomy and postpartum hemorrhage in women in both groups, as well as APGAR score and resuscitation of their newborns.
Results: Nine studies were selected including case-control, cohort and cross-sectional studies.
Data synthesis: Studies found links between genital mutilation and vaginal outlet obstruction, emergency cesarean section and perineal tear.
Conclusion: As for other obstetrical and neonatal complications the researcher’s opinions remain divided. Still, there is some evidence to support the impact of genital mutilation on obstetric and neona tal harm, particularly in type II and III.
Keywords
Female genital mutilation; Cutting; Obstetric; Neonatal complications; Perineal injuries
Introduction
Female Genital Mutilation (FGM) refers to all procedures involving the partial or total removal of the external female genitalia or other mutilation of the female genital organs for non-therapeutic purposes. It is mainly classified by the World Health Organization (WHO) into four main types, which are further divided into subcategories in order to make this classification more complete and precise;
• Type I: Partial or total removal of the clitoris and/or the
prepuce (clitoridectomy).
• Type II: Partial or total removal of the clitoris and the
labia minora, with or without excision of the labia majora
(excision).
• Type III: Narrowing of the vaginal orifice with covering
by cutting and appositioning the labia minora and/or the labia majora, with or without excision of the clitoris
(infibulation).
• Type IV: All other harmful procedures to the
female genitalia organs for nontherapeutic purposes,
such as pricking, piercing, incision, scarification,
and cauterization.
In 2016, the United Nations International Children's Emergency Fund (UNICEF) estimated that 200 million worldwide are victims of FGM. FGM is mainly practiced on Africa, in the Middle East and in Asia. However, with increase in emigration, FGM is found in other parts of the world. Each year, the number of potential new victims amounts to 3 million women. These practices are not without consequences, varying according to the type and severity of FGM. Immediate complications were assessed regardless of the type of mutilation performed. These complications are correlated with hygiene, the experience of the exciser, the procedure and the behavior of the victim. There is a risk of infection (local infection, septic shock). The risk of infection is mainly related to the use of equipment that does not comply with medical hygiene rules urinary disorders (urinary retention, edema of the urethra, dysuria), injuries (damage to adjacent organs, fractures to the femur, collarbone and humerus) and bleeding (hemorrhage, hemorrhagic shock, anemia and death). In addition, there are long-term complications at the urological level (repeated urinary tract infections, urination disorders, urinary incontinence), at the scar level and at the psychological level (depression, post-traumatic syndrome, anxiety). Long-term sequelae of this practice include complications of pregnancy and childbirth. The presence of incision or infibulation increases the chances of developing numerous obstetric complications such as postpartum haemorrhage, episiotomy, cesarean section and neonatal death. Several studies dealing with the effects of FGM on the obstetrical sphere have given divergent results. Some agree and others disagree with the occurrence of obstetric complications. A systematic review and meta-analysis on this topic published in 2014 found that FGM causes harm related to obstetric circumstances, but without considering neonatal consequences. Given the advances in research with new scientific publications on the topic, we therefore decided to carry out an updated systematic review of the scientific studies published from 2000 to 2021 with the aim of studying the various obstetric and neonatal consequences encountered in women who have undergone FGM in order to acquire in-depth knowledge on these consequences [1-8].
Literature Review
Guidelines
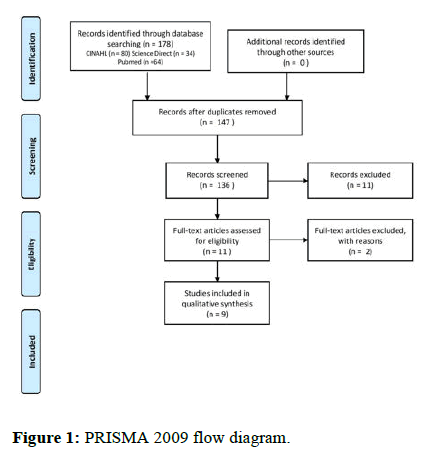
This is a literature review based on the link between FGM and obstetric and neonatal consequences carried out in 2021. The official PRISMA recommendations were used for carrying out and writing the literature review [9].
Database and keywords
The documentary research was carried out from January to October 2021. Different databases were used: PubMed, CINAHL and Science Direct. The descriptors were found using the thesaurus of the various databases. Subsequently, the use of the Boolean operators “OR and AND” allowed to assemble the keywords and descriptors in order to create the search equation which was then developed and specified according to each database. The final generic equation was: (Female genital mutilation OR female genital cutting OR female circumcision) AND (Pelvic pain OR vulval pain OR gynaecology disorders OR delivery disorders OR rupture vulval scar OR perineal tears OR avulsion of the urethra OR avulsion of the bladder OR labour complication OR pelvic organ prolapse OR vaginal injuries OR genital trauma OR pelvic floor dysfunction OR perineal damage OR pelvic floor muscle dysfunction OR pelvic floor disorder OR neonatal OR fetal OR APGAR OR infant OR new-born). Specificity equation was used for each database [10-13].
Eligibility criteria
The selection criteria for the articles were drawn up on PICO basis (Table 1).
| Population | Women who have undergone some type of FGM (I, II, III or IV) and who have obstetric and neonatal complications. |
|---|---|
| Intervention | / |
| Comparison | Women without FGM and/or different types of FGM between themselves. |
| Outcomes | Epidemiological data concerning the following parameters: |
| Vaginal outlet obstruction | |
| Emergency cesarean section | |
| Perineal tear | |
| Instrumental births (forceps, vacuum extractor). | |
| Duration of second stage of labour | |
| Episiotomy | |
| Postpartum hemorrhage | |
| APGAR score | |
| Resuscitation of newborn | |
| Dates | Published Articles from 2010 to 2021. |
| Languages | Articles published in English and French |
Table 1: Eligibility criteria.
Strategy of selection
Two authors independently reviewed the titles and the abstracts of the studies obtained on the databases. Compliance with the eligibility criteria was checked. Subsequently, the same authors independently verified, by using a full reading of the studies, the criteria defined in order to include or exclude them from the review. In case of disagreement, another author helped to decide between the situations.
Methodological quality assessment
To assess the quality of the studies, the McMaster grid was selected. It allowed to assessing different types of studies as well as their internal and external validity. This grid is made up of nine items.
Data analysis
The first table describes the characteristics of the included studies such as design of the study, grade and level of scientific, age, type of mutilation and division of sample. The Table 2 shows the comparison of obstetric outcomes between mutilated women and not mutilated women. The Table 3 shows the comparison of neonatal outcomes in the two groups.
Results
Selection of studies
A total of 178 studies reports were identified. After sorting studies by eligibility criteria according to outcomes, 9 publications reporting on obstetric and neonatal outcomes were included. The selection of studies is represented in a flow chart (Figure 1).
Quality of the studies
Eight studies were considered of good methodological quality whiles the study of presented poor methodological quality (Table 2). This study did not illustrate the eligibility criteria for the participants and the statistics.
| Reference | Design-grade-scientific evidence level | Sample | MGF Type | Age: mean (DS) | McMaster/14 points |
|---|---|---|---|---|---|
| Wuest, et al. | Case-control-grade C-L3 | with FGM n=122, without FGM n=110 | Type I-n=21 | with FGM=27, without FGM=29 | 9 |
| Type II-n=29 | |||||
| Type III-n=58 | |||||
| Type IV-n=14 | |||||
| Chibber, et al. | Case-control-grade C-L3 | with FGM n=1 842 | All type | 23 | 6 |
| without FGM n=2 958 | |||||
| Frega, et al. | Case-control-grade C-L3 | with FGM n=85 | type I et II | with FGM=28 (8,2) | 8 |
| without FGM n=95 | without FGM=23 (6) | ||||
| Abdulcadir, et al. | Case-control-grade C-L3 | with FGM n=76 | Type I-n=5 | 29,6 | 8 |
| Type II-n=12 | |||||
| Type III-n=59 | |||||
| Varol, et al. | Case-control-grade C-L3 | with FGM n=196 | Types I/II-n=131 | 20 to 34 | 8 |
| without FGM n=8 852 | Type III-n=65 | ||||
| Saleh et al. | Cohort study-grade B-L2 | with FGM n=300 | Type I-n=150 | with FGM type I: 30, 6 ± 4 ; Type II: 30, 5 (4,1) | 9 |
| without FGM n=150 | Type II-n=150 | without FGM: 29,6 (4,2) | |||
| Yassin, et al. | Cohort study-grade B-L2 | with FGM n=230 | Type I-n=74 | with FGM=27, 2 (5,8) | 9 |
| without FGM n=190 | Type III-n=156 | without FGM=26 (5,7) | |||
| Gebremicheal, et al. | Cohort study-grade B-L2 | with FGM n=142, without FGM n=139 | Type I-n=37 | with FGM=25, 5(5,6), without FGM=26,1 (4,8) | 9 |
| Type II-n=45 | |||||
| Type III-n=60 | |||||
| Anikwe et al. | Cross sectional study-grade C-L4 | with FGM n=248, without FGM n=248 | Type I-n=50 | with FGM=27,9 (4,8), without FGM=28,4 (4,9) | 9 |
| Type II-n=192 | |||||
| Type III-n=6 |
Table 2: Characteristics of studies.
Data extraction
Characteristics of included studies: All the studies were observational including three cohort studies, five case-control studies and one cross-sectional study. These studies compared groups of mutilated women to not mutilated women, with the exception of which compared only mutilated groups (type I and II vs. type III). Data were collected from medical records of pregnant women attending the maternity wards where the studies took place. The total sample size ranges from 76 to 9048 women with a mean age ranging from 20 and 34 years (Table 3).
| Outcomes | Sample and division | Wuest, et al. | Chibber, et al. | Frega, et al. | Abdulcadir, et al. | Varol, et al. | Saleh, et al. | Yassin et al. | Gebremicheal, et al. | Anikwea, et al. |
|---|---|---|---|---|---|---|---|---|---|---|
| duration of second stage of labor (min) | with FGM | 39*** | - | - | - | - | type I/II: 52 (17,3)* | - | Total=17 (12,4)*; type I:2 (5,6)*; type II: 5 (11,4)*; type III: 10 (17,5)* | type I: 6 (2,4)*; type II: 31 (12,5)*; type III: 6 (2,4)* |
| without FGM | - | - | - | - | 22 (14,6)* | - | 9 (7,1)* | 26 (11,3)* | ||
| P value | - | - | - | - | Length> 60 min: p=NS | - | p=NS; type I: p=NS; type II: p=NS; type III: (p=0,01 ; RR 2,47: 95% CI 1,06-5,76) | Length>2 hours : p=0,001 | ||
| Vaginal outlet obstruction (min) | with FGM | - | - | type I/II: 9,2 (3,7)** | - | - | - | - | Total=50 (35,2)*; type I: 6 (16,2)*; type II:16 (35,6)*; type III: 38 (46,7)* | - |
| without FGM | - | - | 3,2(2,1)** | - | - | - | - | 20 (14,4)* | - | |
| P value | - | - | p=0,001 | - | - | - | - | (p<0,001 ; ARR 1,83: 95% CI 1,19-2,79); type I: p=NS; type II: (p=0,001 ; RR 2,38: 95% CI 1,39-4,08); type III: (p<0,001; RR 2,94 : 95% CI 1,84-4,71) | - | |
| Cesarean section | with FGM | 9* | 884 (48)* | - | I/II : 4 (23,3)* Vs III : 14 (23,7)* | I/II : 36 (32,9)*; III : 16 (26,5)* | I/II : 43 (14,3)* | - | - | type I: 2 (0,8)*; type II: 6 (2,4)*; type III: 0 (0)* |
| without FGM | 8*** | 532 (20)* | - | - | 1706 (20,4)* | 18 (12)* | - | - | 5 (2)* | |
| P value | p=NS | (p<0,05 ; OR 1,7: CI 95% 1,2-2) | - | p=NS | p=0,01 | p=NS | - | - | p=NS | |
| Emergency cesarean section | with FGM | 18*** | - | - | - | - | - | - | Total=26 (18,3)*; type I: 5 (13,5)*; type II:7 (15,6)*; type III: 14 (23,3)* | - |
| without FGM | 3*** | - | - | - | - | - | - | 10 (7,2)* | - | |
| P value | p=0,001 | - | - | - | - | - | - | (p=0,01; ARR 2,31 : 95% CI 1,10-4,82); type I: p=NS; type II: p=NS; type III: (p=0,001 ; RR 3,60 : 95% CI 1,65-7,86) | - | |
| Instrumental births (ventouse/forceps) | with FGM | forceps: 3***; ventouse: 11*** | - | - | type I/II: 4 (23,5)* Vs. type III: 12 (10,4)* | type I/II: 8 (8,2)*; type III: 1 (1,6)* | type I/II: 12 (4)* | - | Type I: 0 (0)*; type II: 4 (1,6)*; type III: 0 (0%)* | |
| without FGM | forceps: 0***; ventouse: 10*** | - | - | - | 574(65)* | 6 (4)* | - | - | 2 (0,8)* | |
| P value | forceps: NS; ventouse: NS | - | - | p=NS | p=NS | p=NS | - | - | p=NS | |
| Episiotomy | with FGM | 24*** | - | primiparous=type I/II: 22 (95,6)*; multiparous=type I/II: 49 (79)* | type I/II : 17 (12,7)*; type III: 7 (10,5)* | type I/II: 153 (51)* | 176 61,7)* | - | type I: 14 (5,6)*; type II: 85 (34,3)*; type III: 6 (2,4)* | |
| without FGM | 16*** | - | primiparous=18 (47,3)*; multiparous=11 (19,3)* | 946 (10,9)* | 946(10,9)* | 71 (47,3)* | 57 (30)* | - | 75 (30,2)* | |
| P value | p=NS | - | primiparous=(p=0,001; OR 24,44:CI 95% 2,99-200); multiparous=(p < 0,001; OR 15,76 : CI 95% 6,42-38,7) | p=NS | p=NS | p=NS | p<0,05 | - | p<0,01 | |
| Perineal tear | with FGM | T1: 6*; T2:6***; T3: 9*** | - | - | T, T1, T2, T3=type I/II Vs. type III | T1/T2=type I, II, III | type I/II=TI: 4 8 (16)*; T2: 43 (14,3)*; T3: 18 (6)*; T4: 0 (0) | - | Total=33 (23,3)*; type I: 4 (10,8)*; type II: 8 (17,8)*; type III: 21 (35,6)* | type I: 14 (5,6)*; type II: 85 (34,3)*; type III: 6 (2,4)* |
| without FGM | T1: 28***; T2: 22***; T3: 1*** | - | - | - | T1/T2 | T1: 8 (5,3)*; T2: 3 (2)*; T3: 1 (0,6)*; T4: 0 (0) | - | 10 (7,2)* | 75 (30,2)* | |
| P value | T1: p<0,001; T2: p <0,01; T3: p <0,05 | - | - | p=NS | p < 0,05 | p < 0,001 | - | (p=0,001; ARR 2,52: 95% CI 1,26-5,02); type I: (p=NS ; RR 1,49 : 95% CI 0,49-4,48); type II: (p=0,042 ; RR 2,45 :95% CI 1,03-5,83); type III: (p<0,001 ; RR 4,91: 95% CI 2,46-9,77) | p<0,01 | |
| Postpartum hemorrhage (ml) | with FGM | 400*** | 254 (13,8)* | - | I/II Vs. III | I/II : 7 (5,6)*; III: 1(1,6)* | I/II: 11(3,6)* | 5 (2,2)* | Total: 16 (11,3)*; type I: 1 (2,7)*; type II: 3 (6,7)*; type III: 11 (18,3)* | type I: 2 (0,8)*; type II: 22 (8,9)*; type III: 4 (1,6)* |
| without FGM | 350*** | 142 (4,8)* | - | - | 615 (7)* | 2 (3)* | 3 (1,5)* | 5 (3,6)* | 24 (9,7)* | |
| P value | p=NS | p=NS (OR 3,3 (95% 0,8-5,5 CI)) | - | p=NS | p=NS | p=NS | p=NS | p: 0,022; type I: p=NS (RR 0,93 (95% CI 0,10-8,15)); type II: p=NS (RR 2,31 (95% CI 0,53-9,96)) ; type III: p=0,001 (RR 6,37 RR 6,37 (95% CI 2,11-19,20)) | p<0,01 |
Table 3: Obstetric outcomes: comparison between women with FGM and women without FGM.
Obstetric outcomes
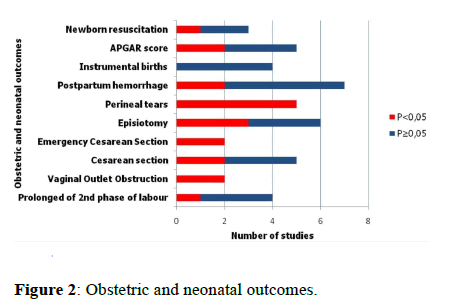
Length of second phase of labour: Found that FGM prolonged the length of the second phase of labour beyond two hours that twice more likely for type III than types I and II according to while three studies found no significant difference.
Vaginal outlet obstruction
The studies of estimated the risk of vaginal outlet obstruction was also observed to be significantly associated with FGM status. Women who undergone FGM had 1.83 times higher risk of vaginal outlet obstruction than women who not undergone FGM (RR=1.83; 95% CI 1.19–2.79). This risk of vaginal outlet obstruction was twice as high in type II and three times as high in type III. So, the mean time of the vaginal outlet obstruction was 9.2 (3.7) min in women who undergone FGM whereas that for women who not undergone FGM was 3.2 (2.1) min (p<0.001) [14-16].
Cesarean section
Found that mutilated women underwent significantly more cesarean sections than not mutilated women while three others studies found no difference between the two groups. In the studies emergency cesarean section was significantly more common in mutilated women point out that this risk is more than four times higher in type III FGM.
Episiotomy
Three authors found that mutilated women were more likely to undergo an episiotomy during childbirth than not mutilated women noted that FGM resulted in a 24-fold increased risk of episiotomy in primiparous and a 16-fold increased risk in multiparous. While other studies found no link.
Perineal tears
Perineal tears are classed in 4 levels (T1 to T4) according to severity. Four studies found that mutilated women had more perineal tears than not mutilated women. This risk was three times higher in type II and five times in types III with significantly more likely to have only third-degree vaginal tears.
Postpartum hemorrhage
Found that mutilated women had a higher risk of postpartum hemorrhage than not mutilated women, with six times the risk in type III. Other studies found no link.
Neonatal outcomes
The results show in Figure 2.
APGAR score
According to Frega, et al. new borns from not mutilated women had a higher Apgar score than new-borns of mutilated women. New-borns of mutilated women had four times higher risk of having an Apgar score of <7 compared to newborns of not mutilated women. Other studies found no significant difference concerning Apgar score.
New-born resuscitation
One study found that FGM was fourfold factor in favour of new-born resuscitation while two studies found no link. Obstetric and neonatal outcomes: Results (test significance) of intergroup comparison between women with FGM and women without FGM (Table 4).
| Wuest, et al. | Chibber, et al. | Frega, et al. | Saleh, et al. | Gebremicheal, et al. | Anikwe, et al. | |
|---|---|---|---|---|---|---|
| APGAR score | APGAR score <7 at 5 min with FGM: 8 (nb) without FGM: 9 (nb) p=NS | APGAR score 9/10 with FGM :17,65% without FGM: 51,6% p<0,001 | APGAR score <7 at 5 min with FGM :1,6% without FGM: 2% p=NS | APGAR score <7 with FGM :12,4% (type I:4,5%, type II:9,1%, type III: 19,9%) without FGM: 5,2% p <0,05 | APGAR score>8 with FGM :type I:19,4%, type II:68,5%, type III:2,4% without FGM: 93,5% p=NS | |
| Newborn resuscitation | with FGM :9,8% without FGM: 5,3% OR 2,2 (95% 1-3,3 CI) | with FGM :35,3% without FGM: 11,58% p<0,001 | with FGM :1,3% without FGM: 0,6% p=NS |
Table 4: Neonatal outcomes: comparison between women with FGM and women without FGM.
Discussion
Characteristics of included studies
Mutilated women were compared to not mutilated women, with the exception of Abdulcadir et al. who compared only the mutilated groups (type I and II vs. type III) attending a specialist clinic for women with FGM in a tertiary center.
Accessibility to optimal obstetric care is not the same in the nine studies: Six took place in countries where FGM is frequently practiced (Burkina Faso, Kuwait, Egypt, Sudan, Niger, Somalia/Ethiopia) and three in western/industrialized countries (Switzerland and Australia) where women victims of mutilation are in minority and are predominantly of migrant origin and have received specialised care. Almost all studies do not distinguish between types of FGM, with the exception of who found the high risk of developing more severe obstetric and neonatal complications in type III compared to others types. There is also a lack of representativeness of the population as the studies did not sufficiently take into account the personal, cultural and socio-economic characteristics of the participants. In addition, a significant proportion of mutilated women are not included in these studies because of the lack of access to health care because of their geographic isolation, the retrospective nature of some studies, the difficulty of contacting mutilated women because of language barriers, and frequent changes in contacts of this population [17-21].
Obstetric and neonatal outcomes
FGM of all types disrupts the normal functioning of the female external genitalia. Although serious complications are possible from all types of FGM, those resulting from type III are common, tend to be more serious and last longer.
Prolonged (length) of second phase of labor and vaginal outlet obstruction
According to the WHO, there is no relationship between prolonged and/or obstructed labour and FGM on the other hand some recent studies have found the influence of FGM on the second phase of labour. This may be explained by the association of high maternal and fatal morbidity at delivery, such as fetomaternal disproportion. According to Larsen, et al. the intact perineum easily gives way during the second stage of labour due to overstretching. This stage is complicated by the presence of scar tissue resulting from FGM, which opposes fatal descent due to vaginal outlet obstruction, prolonging the second phase of labour and increasing maternal and neonatal complications (perineal tears and stillbirths). These complications are more prevalent in types II and III FGM.
Perineal tear, postpartum hemorrhage and neonatal complications
All studies have shown that FGM causes perineal tears during labour with the higher risk depending on the severity of the damage to the female external genitalia (scars). The studies of Abdulcadir, et al. found that perineal tears were not significantly more frequent in infibulated women, probably due to defibulation performed during obstetric management. Scarred portion of the introitus becomes more resistant than the perineum with a higher concentration of mature collagen in the tissues after recurrent incision and healing. Thus, parous women after FGM may have reduced tissue elasticity and, therefore, a greater probability of third-degree vaginal tears. Some authors have found that women with FGM have a higher risk of postpartum haemorrhage than women without FGM and FGM type III have a six-fold increased risk of postpartum haemorrhage. Although uterine atony is the most common cause of postpartum haemorrhage, genital laceration (scars and keloids) is a significant contributor in case of FGM. Therefore, FGM is associated with excessive blood loss through bleeding at the episiotomy site, genital laceration and tears. This finding is also consistent with other studies. These complications may be fewer when the procedure is undertaken by a trained operator, although cases of death due to uncontrolled bleeding from the clitoral artery have occurred even when performed by a trained physician [22].
APGAR score and neonatal resuscitation
Interestingly, prolonged second phase of labour or vaginal outlet obstruction in mutilated women contributes to lower Apgar scores and neonatal resuscitation. Type III is the most favourable factor. Scarring leads to vaginal stenosis with loss of its natural elasticity resulting in cessation of the decent of the fetus presentation at birth. Because of this obstetric situation, fetal distress may result in lower Apgar scores and neonatal resuscitation. According to Saleh, et al. the lack of implication of FGM on neonatal outcomes should be interpreted with caution. This could be attributed to studies investigating the impact of more severe types of genital cutting or else the level of care in a tertiary referral unit might have reduced the potential complications associated with this practice.
Management strategies
In order to prevent the complications mentioned above in mutilated women, they may either undergo defibulation, episiotomy or cesarean section, and this is often done urgently. For Frega, et al. first and foremost, health professionals need to know the most common complications of childbirth in order to prevent them and provide the best individualised care to mutilated women. Defibulation procedures are practiced by the specialist team of midwives and obstetricians. It is performed in women with type III FGM before pregnancy, during second trimester or during labour to reduce the risk of prolonged second phase of labour and spontaneous laceration. Women can choose whether they prefer partial (to the urethral meatus) or total (to the clitoris) opening. Some mutilated women who have a strong traditional and cultural background request infibulation or restore of the vaginal orifice in postpartum period. Episiotomy was more performed in women with type I and II FGM. These results must be qualified because of the preventive practice of these episiotomies, the aim of which is to prevent perineal tears and prolonged of second phase of labour or because of the practitioners’ habits and/or the protocol implemented in each place of care. Some authors found significant relationship between the practice of FGM and the episiotomy because of pelvic floor and vagina scars. This risk of episiotomy was 24 times in primiparous and 16 times in multiparous women with FGM. If keloids have formed and are too large or in case of type III FGM cesarean section may be the best option to manage the delivery. According to some authors, women with FGM have twice as many cesarean sections or emergency cesarean section as women without FGM women with type III have a significantly higher risk (four times) of emergency cesarean section. However, according to the study by the main reason for emergency cesarean section was the inability to perform a vaginal exam during labour in women with FGM III who had not been defaulted. They wonder whether the cesarean section rate would have been even higher if all women had been defaulted and allowed to continue labour.
Although some authors have not found an association between FGM and certain obstetric and neonatal complications such as prolongation of the second phase of labour, episiotomy, postpartum haemorrhage, APGAR score and resuscitation new-borns, it is important to note that FGM can lead to major long-term sequelae that may influence them. According to there is uncertainty about the magnitude of the greater risk of obstetric harm in mutilated women compared to women without FGM, but there is sufficient evidence to conclude that FGM causes obstetric damage.
Involvement of re-education
Episiotomy, defibulation or surgical repair of a perineal tear can sometimes heal with scars that may adhere to underlying structures which if left untreated become a persistent problem leading to postnatal perineal pain, urinary or fecal incontinence, dysuria. Given all FGM obstetric and neonatal consequences revolve around scarring, physiotherapy management is beneficial to influencing these consequences before pregnancy and after childbirth in mutilated. In the study by a long-term follow-up, including counselling and postpartum perineal physiotherapy was organized, aiming to improve perineal tone and self-knowledge of genital organs anatomy and physiology. Therefore, some re-education techniques and their benefits in these cases are developed in the literature such as therapeutic ultrasound, scar mobilization and massage resulting in tissue repair and remodelling and pain relief had noticed in their study that awareness of physiotherapy management for FGM is neglected by physiotherapists and gynaecologists in India, possibly even in other countries. Reason why research in this area is very minimal to support and define the best physiotherapy management for the women benefits. It is therefore important to continue to conduct studies on this topic in order to establish individualised management protocols for each type of mutilation, in particular for physiotherapy.
Conclusion
Studies are unanimous on the association between FGM and vaginal outlet obstruction, emergency cesarean section and perineal tear. As for other obstetrical and neonatal complications the researchers opinions remain divided. The methodological quality limits of those studies do not allow for proof causation. So, the lack of FGM involvement on those obstetric and neonatal outcomes should be interpreted with caution. Still, there is some evidence to support the impact of FGM on obstetric and neonatal harm, particularly in type II and III. For this reason, reducing the practice of FGM will reduce the risk of obstetric and neonatal complications.
Implications for practice
• Studies are unanimous on the association between FGM
and vaginal outlet obstruction, emergency cesarean
section and perineal tear.
• The opinions of the researchers remain divided
concerning the link between FGM and some obstetric and
neonatal consequence during childbirth such as prolonged
of the second phase of labour, episiotomy, cesarean
section, postpartum hemorrhage, APGAR score and
resuscitation of the new-born.
• This systematic review shows that there is some evidence
to support the impact of FGM on obstetric and neonatal
harm, particularly in type II and III.
Conflict of Interest
The authors declare no competing interest.
References
- UNICEF (Ed). Female genital mutilation/cutting: A statistical exploration 2005. United Nations Children’s Fund. UNICEF Publications, London, United Kingdom. 2005:1-53.
- World Health Organization. Eliminating female genital mutilation: An interagency statement-OHCHR, UNAIDS, UNDP, UNECA, UNESCO, UNFPA, UNHCR, UNICEF, UNIFEM, WHO. World Health Organization publication. Geneva, Switzerland. 2008:1-40.
- Llamas J. Female Circumcision: The history, the current prevalence and the approach to a patient April 2017 Jewel. Course Hero. 2022;22:1-7.
- Yoder PS, Khan S. Numbers of women circumcised in Africa: The production of a total (DHS Working Papers No. 39). DHS Working Papers, Maryland, USA. 2008.
- Andro A, Lesclingand M. Les mutilations genitales feminines. Etat des lieux et des connaissances. Popul. 2016;71:224–311.
- Berg RC, Underland V, Odgaard-Jensen J, Fretheim A, Vist GE. Effects of female genital cutting on physical health outcomes: A systematic review and meta-analysis. BMJ Open. 2014;4:006316.
[Crossref] [Google Scholar] [PubMed]
- Reisel D, Creighton SM. Long term health consequences of Female Genital Mutilation (FGM). Maturitas. 2015;80:48–51.
[Crossref] [Google Scholar] [PubMed]
- Agugua NE, Egwuatu VE. Female circumcision: Management of urinary complications. J Trop Pediatr. 1982;28:248-252.
[Crossref] [Google Scholar] [PubMed]
- Millet P, Vinchant M, Sharifzadehgan S, Vieillefosse S, Gantzer GH, Deffieux X. Lower urinary tracts symptoms after female genital mutilation: A review. Prog Urol. 2019;29:209-215.
[Crossref] [Google Scholar] [PubMed]
- Nzinga AM, Castanheira SDA, Hermann J, Feipel V, Kipula AJ, Bertuit J. Consequences of female genital mutilation on women’s sexual health systematic review and meta-analysis. J Sex Med. 2021;18:750-760.
[Crossref] [Google Scholar] [PubMed]
- Teufel K, Dorfler DM. Female genital circumcision/mutilation: Implications for female urogynaecological health. Int Urogynecol J. 2013;24:2021-2028.
[Crossref] [Google Scholar] [PubMed]
- Berg RC, Jensen J, Fretheim A, Underland V, Vist G. An updated systematic review and meta-analysis of the obstetric consequences of female genital mutilation/cutting. Obstet Gynecol Int. 2014;014:542859.
[Crossref] [Google Scholar] [PubMed]
- Essen B, Sjoberg NO, Gudmundsson S, Ostergren PO, Lindqvist PG. No association between female circumcision and prolonged labour: a case control study of immigrant women giving birth in Sweden. Eur J Obstet Gynecol Reprod Biol. 2005;121:182-185.
[Crossref] [Google Scholar] [PubMed]
- Meirik E, Farley T, Akande O, Bathija H, Ali M. Female genital mutilation and obstetric outcome: WHO collaborative prospective study in six African countries. Lancet 2006;367:1835-1841.
[Crossref] [Google Scholar] [PubMed]
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. PRISMA-P Group preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;1:4:1.
- Law M, Stewart D, Pollock N, Letts L, Bosch J, Westmorland M. Guidelines for critical review form quantiative studies. Rev Quant. 1998;2:1-9.
- Abdulcadir J, Dugerdil A, Yaron M, Irion O, Boulvain M. Obstetric care of women with female genital mutilation attending a specialized clinic in a tertiary center. Int J Gynaecol Obstet. 2016;132:174-178.
[Crossref] [Google Scholar] [PubMed]
- Anikwe CC, Ejikeme BN, Obiechina NJ, Okorochukwu BC, Obuna JA, Onu FA, et al. Female genital mutilation and obstetric outcome: A cross-sectional comparative study in a tertiary hospital in Abakaliki South East Nigeria. Eur J Obstet Gynecol Reprod Biol. 2019;10:100005.
[Crossref] [Google Scholar] [PubMed]
- Chibber R, Saleh E, Harmi J. Female circumcision: Obstetrical and psychological sequelae continues unabated in the 21st century. J Matern Fetal Neonatal Med. 2011;24:833–6.
[Crossref] [Google Scholar] [PubMed]
- Frega A, Puzio G, Maniglio P, Catalano A, Milazzo GN, Lombardi D, et al. Obstetric and neonatal outcomes of women with FGM I and II in San Camillo Hospital, Burkina Faso. Arch Gynecol Obstet. 2013;288:513-519.
[Crossref] [Google Scholar] [PubMed]
- Gebremicheal K, Alemseged F, Ewunetu H, Tolossa D, Ma’alin A, Yewondwessen M, et al. Sequela of female genital mutilation on birth outcomes in Jijiga town, Ethiopian Somali region: A prospective cohort study. BMC Pregnancy Childbirth. 2018;18:305.
[Crossref] [Google Scholar] [PubMed]
- Saleh WF, Torky HA, Youssef MA, Ragab WS, Ahmed MAS, Eldaly A. Effect of female genital cutting performed by health care professionals on labor complications in Egyptian women: A prospective cohort study. J Perinat Med. 2018;46:419-424.
[Crossref] [Google Scholar] [PubMed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.