Gorlin‑Goltz Syndrome
- *Corresponding Author:
- Dr. Dhaval N Mehta
Department of Oral Medicine and Radiology, Karnavati School of Dentistry, Gandhinagar, Gujarat, India.
E-mail: drdhaval80@gmail.com
Citation: Mehta DN, Raval N, Patadiya H, Tarsariya V. Gorlin-Goltz syndrome. Ann Med Health Sci Res 2014;4:279-82.
Abstract
The Gorlin‑Goltz syndrome (GGS) (the nevoid basal cell carcinoma syndrome) is a rare autosomal dominant syndrome caused due to mutations in the patched gene found on chromosome arm 9 q. It shows high penetrance and variable expressivity; is characterized by basal cell carcinomas, odontogenic keratocysts, palmar and/or plantar pits and ectopic calcifications of the falx cerebri. Until date, very few cases of GGS have been reported in India. Early diagnosis and treatment as well as genetic counseling are essential for this syndrome. A rare case report of a patient with characteristic features of GGS diagnosed at a rural dental college of Gujarat, India is presented here. This case report draws attention of the valuable role of dentist in diagnosis and early management of this syndrome.
Keywords
Carcinoma, Gorlin-Goltz syndrome, Odontogenic keratocyst
Introduction
Gorlin-Goltz syndrome (GGS) is an uncommon autosomal dominant inherited disorder.[1] It is characterized by basal cell carcinomas, odontogenic keratocysts (OKCs), palmar and/or plantar pits and ectopic calcifications of the falx cerebri.[2] It was first reported by Jarisch and White in 1894. Ljubenovi M had mentioned that Robert J. Gorlin and Robert W. Goltz described the distinct syndrome, consisting of the presence of multiple nevoid basal cell epitheliomas, jaw cysts and bifid ribs.[1] This triad was later modified and established that, for giving the diagnosis at least cysts had to appear in combination with calcification of the falx cerebri or palmar and plantar pits.[3] The incidence of this disorder is estimated to be 1 in 50,000-150,000 in the general population, varying by region. The prevalence rate in the United Kingdom was 1/560,000. He reported review revealed that, to date, there are only seven cases of the GGS reported from India, out of which only two were from North India and five were from South India. It arises in all ethnic groups, but most reports have been in whites. The clinical features of nevoid basal cell carcinoma arise in the first, second or third decade of life.[4] Generally OKC are not associated with nevoid basal cell carcinoma Syndrome (NBCCS), which are more common in the adult life, the peak incidence being the third decade of life. However, in the GGS, OKC occurs at a much younger age. OKCs were often the first sign of NBCC in 78% of the cases and they could be detected in patients younger than 10 years of age. Males and females are equally affected. Male to female ratio is 1:0.62 for OKC not associated with NBCCS and 1:1. For OKC in NBCCS, that is, simple keratocysts are more common in males, but more females with NBCCS develop OKCs.[2]
We here report a case of GGS, which emphasizes the role of dentist in recognizing these features in order to get early diagnosis and a multidisciplinary approach in treating the condition.
Case Report
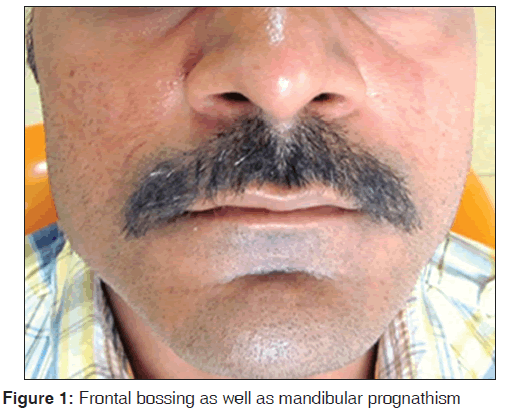
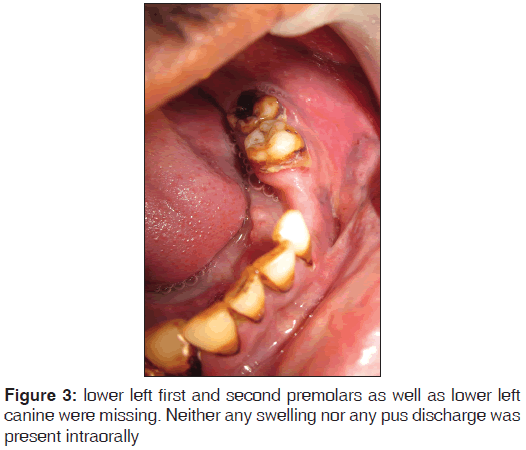
A 32-year-male patient came with difficulty in chewing on lower left back teeth region since 1 year due to missing teeth. He got extracted these teeth due to carious lesions of the teeth before 1 year. Patient had a habit of Gutkha chewing since 8 years. Patient was conscious, co-operative, fairly built and well oriented to time and place. Height (5′9″) and weight (70 kg) were normal. Body mass index was 22.8. Patient had bilaterally symmetrical face. Flattening of the nasal bridge was evident. There was a presence of frontal bossing (head circumference was 61 cm). Mandible appeared to be prognathic [Figure 1]. Palmar pits in both hands were evident [Figure 2]. Extrinsic tobacco stains were present in all teeth. Lower left first and second premolar as well as lower left canine was missing [Figure 3]. Neither any swelling nor any pus discharge were present (intra or extra-orally).
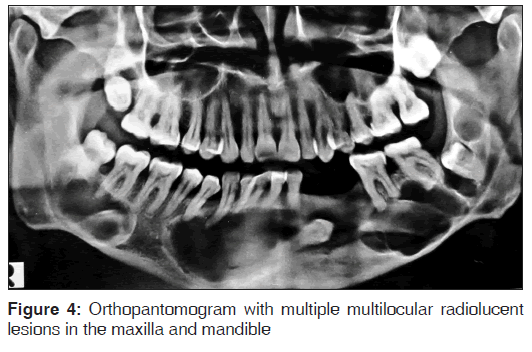
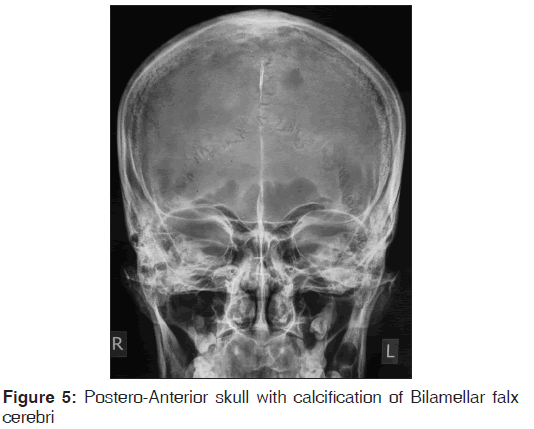
Orthopantomogram showed multiple (three) radiolucencies in the mandibular throughout the length of the mandible along with impacted third molar and canine on the right side. Moreover, radiolucency is present in the maxilla in relation to impacted third molar on the right side. All radiolucencent lesions were multilocular with well-defined sclerotic borders [Figure 4]. The Skull radiograph showed bilamellar calcification of falx cerebri [Figure 5]. Chest radiograph did not show any significant changes no other anomalies of the skeletal, cardiovascular or central nervous system were present. A provisional diagnosis of GGS was made.
An incisional biopsy of cystic lesions of the jaw was performed and histopathological examination showed the cystic tissue with corrugated, wavy parakeratotic squamous epithelium lining. The cyst wall is composed of fibrous tissue with moderate subepithelial mixed inflammatory infiltrate composed of neutrophils and lymphoplasmacytic cells suggestive of OKC. Patient was then referred to the Department of Oral and Maxillo Facial Surgery for the further management. On the basis of classical clinical, radiographic and histologic features, final diagnosis of GGS was made. None of the family members of the patient have the same problem.
Discussion
GGS is an infrequent multisystemic disease that is inherited in a dominant autosomal way, which shows a high level of penetrance and variable expressiveness. This syndrome has received several names throughout the times such as “basal cell nevus syndrome” “nevoid basal cell carcinomas syndrome” or the most complex name of “multiple basal epithelioma, jaw cysts and bifid rib syndrome.”[3] The GGS is manifested by multiple defects involving the skin, nervous system, eyes, endocrine system and bones.[2]
The tumor suppressor gene called Patched located in the 9q22.3 chromosome, has been identified as the cause of GGS.[3]
Clinical manifestations of the syndrome are grouped into the following five categories:[2]
1. Cutaneous anomalies: Basal cell nevus, other benign dermal cysts and tumors, palmar pitting, palmar and plantar keratosis and dermal calcinosis
2. Dental and osseous anomalies: Multiple OKC, mild mandibular prognathism, frontal and temporoparietal bossing, kyphoscoliosis or other vertebral defects, bifurcated ribs, spina bifida and brachymetacarpalism
3. Ophthalmic anomalies: Hypertelorism, wide nasal bridge, dystopia canthorum, congenital blindness and internal strabismus
4. Neurological anomalies: Mental retardation, dural calcification, bridging of sella, agenesis of the corpus callosum, congenital hydrocephalus, occurrence of medulloblastoma
5. Sexual anomalies: Hypogonadism, ovarian tumor-like fibrosarcoma.
Clinically this condition is characterized by different signs and symptoms. Diagnosis is based on the most frequent and specific features of the syndrome as given by Evans et al. in 1993.[5] Diagnosis of GGS can be established when two major or one major and two minor criteria are present.[5-7]
The major criteria are:
1. Multiple basal cell carcinomas or one occurring under the age of 20 years
2. Histologically proven OKCs of the jaws
3. Palmar or plantar pits (three or more)
4. Bilamellar calcification of the falx cerebri
5. Bifid, fused or markedly splayed ribs
6. First-degree relative with NBCCS.
The minor criteria are:
1. Macrocephaly (adjusted for height).
2. Congenital malformation: Cleft lip or palate, frontal bossing, coarse face, moderate or severe hypertelorism
3. Other skeletal abnormalities: Sprengel deformity, marked pectus deformity, marked syndactily of the digits
4. Radiological abnormalities: Bridging of the sella turcica, vertebral anomalies such as hemivertebrae, fusion or elongation of the vertebral bodies, modeling defects of the hands and feet or flame shaped hands or feet
5. Ovarian fibroma
6. Medulloblastoma.
In our patient, the diagnosis of the GGS was established by the presence of two major criteria (viz., multiple OKC and calcified falx cerebri) and three minor criteria (viz. palmer pits, mandibular prognathism, frontal bossing).
Multiple OKCs usually occur as a component of NBCCS or GGS, Oro-facial-digital syndrome, Noonan syndrome, Ehler-Danlos syndrome, Simpson-Golabi-Behmel syndrome.[8] In our case, clinical and radiological features were not in concordance with any other syndromes except GGS.
Although GGS is primarily recognized by multiple basal cell carcinomas, it was not evident in our case. The incidence varies widely among ethnic groups. Only about 40% of black patients affected by NBCCS manifest basal cell carcinoma, while in whites they are reported in up to 90% of cases.[9]
The reported review revealed that, to date, there are only seven cases of the GGS reported from India, out of which only two were from North India and five were from South India. This most probably represents under-recognition due to inadequate dental facilities, especially in the vast rural regions of India, outside big cities. Less than 10% of patients with multiple OKCs have other manifestations of this syndrome. It has therefore been suggested that multiple OKCs alone may be confirmatory of the syndrome. Our case too presented with multiple cystic lesions involving the mandible, which was histopathologically diagnosed as an OKC.[2]
Conclusion
Early diagnosis of GGS is important to reduce the severity of complications, such as skin and brain malignant tumors. Radiographic examination of the patient helped in diagnosis of GGS so role of oral physician is very important in reducing and preventing serious complications of GGS.
References
- Ljubenovi M, Ljubenovi D, Bini I, Jovanovi D, Stanojevi M. Gorlin-Goltz syndrome. Acta Dermatoven 2007;16:166-9.
- Jawa DS, Sircar K, Somani R, Grover N, Jaidka S, Singh S. Gorlin-Goltz syndrome. J Oral Maxillofac Pathol 2009;13:89-92.
- Ortega García de Amezaga A, García Arregui O, Zepeda Nuño S, Acha Sagredo A, Aguirre Urizar JM. Gorlin-Goltz syndrome: Clinicopathologic aspects. Med Oral Patol Oral Cir Bucal 2008;13:E338-43.
- Patil K, Mahima VG, Gupta B. Gorlin syndrome: A case report. J Indian Soc Pedod Prev Dent 2005;23:198-203.
- Evans DG, Sims DG, Donnai D. Family implications of neonatal Gorlin's syndrome. Arch Dis Child 1991;66:1162-3.
- Pandeshwar P, Jayanthi K, Mahesh D. Gorlin-goltz syndrome. Case Rep Dent 2012;2012:247239.
- Agrawal A, Murari A, Vutukuri S, Singh A. Gorlin-goltz syndrome: Case report of a rare hereditary disorder. Case Rep Dent 2012;2012:475439.
- Auluck A, Suhas S, Pai KM. Multiple odontogenic keratocysts: Report of a case. J Can Dent Assoc. 2006;72:651-6.
- Lo Muzio L. Nevoid basal cell carcinoma syndrome (Gorlin syndrome). Orphanet J Rare Dis 2008;3:32.





 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.