Hashimotos Thyroiditis with Coexistent Papillary Carcinoma and Non‑hodgkin Lymphoma‑thyroid
- *Corresponding Author:
- Dr. Kishan Prasad HL
Department of Pathology, KS Hegde Medical Academy of Nitte University, Deralakatte, Mangalore - 575 018, Karnataka, India.
E-mail: dr_kishanpath@yahoo.com
Citation: Jayaprakash KS, Kishanprasad HL, Hegde P, Chandrika R. Hashimotos thyroiditis with coexistent papillary carcinoma and non-hodgkin lymphoma-thyroid. Ann Med Health Sci Res 2014;4:268-70.
Abstract
Lymphocytic thyroiditis and hashimoto’s thyroiditis (HT) are the two main forms of autoimmune thyroiditis among which the latter is most frequent. A vast majority of cases of papillary carcinoma and primary thyroid lymphoma (PTL) arise in the setting of HT. A case of 32‑year‑old female who presented with thyroid enlargement, post‑thyroidectomy showed hashimoto’s thyroiditis (HT) with coexistent papillary carcinoma and non‑hodgkin lymphoma (NHL). The immunohistochemistry was positive for CD 20, CD 45, bcl 2 for lymphoma, low and high molecular cytokeratin for papillary carcinoma. The staging studies showed no evidence of metastasis. It is thus concluded that papillary carcinoma and NHL can coexist with HT. The thyroid lymphoma or papillary carcinoma has to be thought off, whenever patients presents with sudden enlargement in a known case of HT. A patient presenting with concomitant primary thyroid lymphoma and papillary thyroid carcinoma must be judiciously evaluated, since, the treatment has to prioritize the tumor with worst stage at the time of diagnosis.
Keywords
Extranodal, Hashimoto’s thyroiditis, Non-hodgkin, Papillary carcinoma
Introduction
Lymphocytic thyroiditis and hashimoto’s thyroiditis (HT) are the two main forms of autoimmune thyroiditis among which the latter is most frequent.[1-3] A vast majority of cases of papillary carcinoma and primary thyroid lymphoma (PTL) arise in the setting of HT. The estimated risk of developing a thyroid lymphoma is increased to 67-80 fold in patients with HT and evolution to PTL occurs in 0.5% of patients.[4] Malignant lymphomas of the thyroid gland constitute 2-5% of thyroid malignancies.[1,3-5] Simultaneous occurrence of both papillary carcinoma and PTL in HT is very rare.[3,4,6] Here, we report such association in a 32-year-old female, who presented with solitary thyroid nodule. Complete evaluation revealing HT with stage IE non-hodgkin lymphoma (NHL) and papillary carcinoma, who was treated with R-CHOP regime. After 12 months of follow-up, the patient is stable without evidence of recurrence or metastasis.
Case Report
A 32-year-old female with solitary nodule and hypothyroidism since 6 months, presented with a sudden increase in size since 15 days. Local examination showed a solitary nodule in the left lobe of the thyroid. General, physical, and systemic examinations were within normal limits. There were no clinically palpable cervical lymphnodes. Thyroid function test showed high thyroid stimulating hormone and decreased T4 levels. Ultrasound neck showed enlarged thyroid with nodularity and hyperechoic areas. Fine needle aspiration cytology (FNAC) of the nodule showed features of HT with papillary carcinoma.
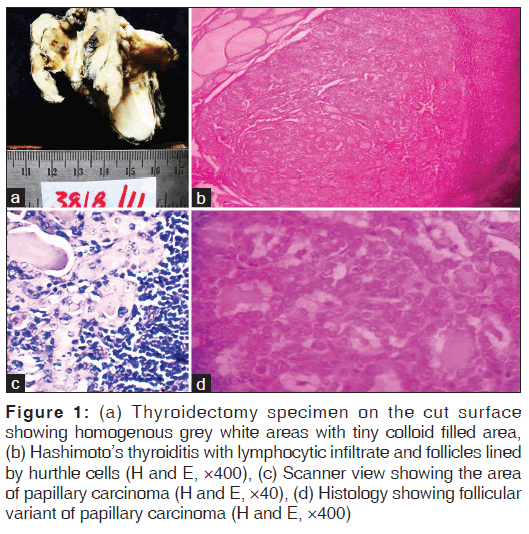
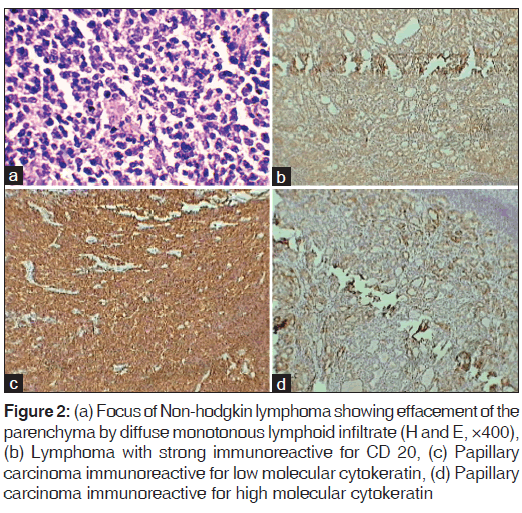
Hence, a total thyroidectomy was performed and revealed nodularity on the outer surface. Left lobe measured 4 cm × 2.5 cm × 1.5cm and right lobe measured 3 cm × 2 cm × 1 cm. Cut surface of both the lobes was homogenous, grey white with tiny colloid filled areas [Figure 1a]. Histology showed areas of HT with prominent lymphoid follicles having germinal center and atrophied thyroid follicles lined by hurthle cells [Figure 1b]. A tiny focus of follicular variant of papillary carcinoma was also seen [Figure 1c and d]. Another focus showed effacement of the thyroid parenchyma by diffuse monotonous lymphoid infiltrate suggestive of NHL [Figure 2a]. Immunohistochemistry showed these cells immunoreactive for CD 45, CD 20, and bcl 2, which suggested a B-cell origin [Figure 2b]. Areas of papillary carcinoma showed positivity for both low and high molecular weight cytokeratin [Figure 2c and d]. Hematological parameters and marrow evaluation were within the normal limits. Hence, the final diagnosis of HT coexisting with papillary carcinoma and primary NHL (B-cell lineage) was made. Levothyroxine was initiated at 300mcg/day and patient was treated with chemotherapy (R-CHOP regime). Patient tolerated the chemotherapy well and with 12 months of follow-up, no recurrence or metastasis was noted.
Figure 1: (a) Thyroidectomy specimen on the cut surface showing homogenous grey white areas with tiny colloid filled area, (b) Hashimoto’s thyroiditis with lymphocytic infiltrate and follicles lined by hurthle cells (H and E, ×400), (c) Scanner view showing the area of papillary carcinoma (H and E, ×40), (d) Histology showing follicular variant of papillary carcinoma (H and E, ×400)
Figure 2: (a) Focus of Non?hodgkin lymphoma showing effacement of the parenchyma by diffuse monotonous lymphoid infiltrate (H and E, ×400), (b) Lymphoma with strong immunoreactive for CD 20, (c) Papillary carcinoma immunoreactive for low molecular cytokeratin, (d) Papillary carcinoma immunoreactive for high molecular cytokeratin
Discussion
HT is the most common form of autoimmune thyroiditis. Papillary carcinoma is one of the complications of HT.[3,5] Several retrospective studies have revealed a strong correlation between these two diseases, where as some studies have failed to show any such association.[4-6] Majority of the HT patients with associated papillary carcinoma will have a dominant thyroid nodule and they do not respond to suppressive therapy and have clinical signs of metastasis.[4] Most of these lesions are detected incidentally suggesting the requirement of a routine follow-up in HT patients. According to some studies, FNAC has a sensitivity of > 90% and negative predictive value of 96% in detecting these lesions.[4,6,7] FNAC is the procedure of choice for evaluating thyroid nodules and selecting candidates for surgery.[7] FNAC followed with biopsy has resulted in improved diagnostic accuracy and significant cost reductions.[6,7] In our case, FNAC showed papillary carcinoma with HT.
Most thyroid lesions can be readily diagnosed using histopathologic criteria, which allow the pathologist to differentiate benign and malignant lesions and guarantee an accurate classification for the majority of the variants of carcinomas derived from follicular epithelial cells.[7-9] In few cases, immunohistochemistry will be useful to confirm the finding. From the extensive list of markers, the ones that have shown acceptable sensitivity and specificity includes low and high molecular weight cytokeratin, galectin 3, HBME-1, and cyclooxygenase 2.[8,9] In our case, papillary carcinoma foci was immunoreactive for low and high molecular cytokeratin.
Malignant lymphoma of the thyroid is a rare complication of HT. This association represents a pathogenic link between neoplastic proliferation and autoimmune disease.[5-8] This tumor comprises 2.5-3% of all extra nodal lymphomas, 4-5% of all thyroid malignancies and is predominantly seen in elderly females.[5,6] However, our case was 32-year-old female and lymphoma occurring in young patients is rare. Non-hodgkins lymphoma of B-cell type is the most common. These lymphomas mainly include lymphomas of the mucosa associated lymphoid tissue (MALT), which is characterized by the presence of atypical lymphoid cells, which originate within the marginal zone of lymphoid follicles and extend to inter-follicular space.[3,5,7,8] Tumor spread can be to cervical or perithyroid lymph nodes followed by mediastinal and abdominal nodes. In our case, complete evaluation revealed no significant lymph nodes. Immunohistochemistry plays a vital role in confirmation of the type of lymphoma. In our case, lymphoid cells were strong immunoreactivity for CD 45, bcl 2 and CD 20 suggesting B-cell origin of the tumor.
Extranodal marginal zone B-cell lymphoma of MALT type has a better prognosis compared to diffuse large B-cell type.[1,3,7,8] Tumor bulk and extra capsular extension have adverse prognostic effects.[3,7,8] Staging includes computed tomography (CT) neck, thorax, abdomen and pelvis, positron emission tomography-CT, total body scintigraphy with MIB
1, laboratory evaluation, and bone marrow biopsy.[8] All investigations showed no evidence of metastasis, hence staged as stage IE, without systemic B symptoms.
There has been no literature to date regarding the optimal management of the simultaneous occurrence of papillary carcinoma and MALT lymphoma.[8,9] The management of one is not affected by the management of the other, and the prognosis is probably affected by the one having the worst stage.[9] A patient presenting the concomitant MALT thyroid lymphoma and papillary thyroid carcinoma must be judiciously evaluated; since, the treatment has to prioritize the tumor with the worst prognosis at the time of diagnosis. In our case, after 12 months of follow-up, patient is stable without evidence of recurrence or metastasis.
We here by conclude that papillary carcinoma and non-hodgkins lymphoma can coexist with HT. In a pre-existent case of HT, newly developed solitary nodule should be carefully evaluated to rule out associated malignant tumors.
References
- Satish V, Bhagavan BC, Sridhar. Primary non-hodgkins lymphoma of the thyroid with lymphocytic thyroiditis. RGUHS J Med Sci 2011;3:62-4.
- Panayiotides IG, Foukas PG, Meristoudis C, Zourla AP, PerosG, KarakitsosP. Simultaneous occurrence of Warthin-like papillary carcinoma and lymphoma of the mucosa associated lymphoid tissue in Hashimoto thyroiditis. J Clin Pathol 2010;63:662-3.
- Banu DG, Mustafa OG, Karamanoglu Z. Primary thyroid lymphoma arising in the setting of Hashimotos thyroiditis. Turk J Med Sci 2004;34:395-8.
- Cheng V, Brainard J, Nasr C. Co-occurrence of papillary thyroid carcinoma and primary lymphoma of the thyroid in a patient with long-standing Hashimoto’s thyroiditis. Thyroid 2012;22:647-50.
- Singh B, Shaha AR, Trivedi H, Carew JF, Poluri A, Shah JP. Coexistent Hashimoto’s thyroiditis with papillary thyroid carcinoma: Impact on presentation, management, and outcome. Surgery 1999;126:1070-6.
- Melo GM, Sguilar DA, Petiti CM, Eichstaedt AG, Caiado RR, Souza RA. Concomitant thyroid Malt lymphoma and papillary thyroid carcinoma. Arq Bras Endocrinol Metabol 2010;54:425-8.
- Mazokopakis EE, Tzortzinis AA, Dalieraki-Ott EI,Tsartsalis AN, Syros PK, Karefilakis CM, et al. Coexistence of Hashimoto’s thyroiditis with papillary thyroid carcinoma. A retrospective study. Hormones (Athens) 2010;9:312-7.
- Fischer S, Asa SL. Application of immunohistochemistry to thyroid neoplasms. Arch Pathol Lab Med 2008;132:359-72.
- Baloch ZW, LiVolsi VA. Fine-needle aspiration of the thyroid: Today and tomorrow. Best Pract Res Clin Endocrinol Metab 2008;22:929-39.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.