Health Risk Assessment Linked to Critical Air Pollutants’ Exposure
2 Department of Health Science, Asthma Bhawan, Shyam Nagar, Jaipur, India
Received: 05-Aug-2022, Manuscript No. AMHSR-20-21747; Editor assigned: 08-Aug-2022, Pre QC No. AMHSR-20-21747; Reviewed: 22-Aug-2022 QC No. AMHSR-20-21747; Revised: 29-Aug-2022, Manuscript No. AMHSR-20-21747; Published: 05-Sep-2022
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Air pollution causes serious health impact as one-third of deaths occur due to exposure to air pollutants. The pollutant has both acute and chronic effects which go deep into the organ systems and deposit into tissues and causes long-term and short-term effects on the human body. Objective: The objective of this review is to develop a quantitative understanding of the current state of knowledge about potential health effects with respect to the dose-response relationship between exposure to criteria air pollutants and health risk assessment. Methods: High quality scientific research papers were drawn with consideration of experimental design, conduct and reporting for analyzing the exposures to criteria air pollutants via inhalation which imitate the expected route of exposure to the humans. Results: The majority of the evidence refers to effects on the respiratory system, cardiovascular, inflammatory and blood affecting diseases. Conclusion: This critical assessment investigated the effects on susceptible subjects and stimulated diseases which are classified as physiological and psychological diseases. This critical assessment investigated the effects on susceptible subjects and stimulated diseases like asthma, chronic obstructive pulmonary disease, allergic rhinitis, Alzheimer's, Diabetes, etc.
Keywords
Criteria air pollutants; Lung disorders; Heart diseases; Auto-immune diseases; Blood disorders
Introduction
Environmental contamination is a serious concern which arises due to natural and anthropogenic activities and adversely affects human health. One of the major types of environmental pollution attributed to air pollutants is considered in terms of exposure and the consequences due to exposure on human health. Based upon the air pollutant mixture, these can be divided into primary pollutants and secondary pollutants. Primary air pollutants directly emit from the source and enter into the atmosphere. Primary air pollutants such as burning of fossil fuels, gases emissions from vehicles, thermal power plants emit nitrogen oxides while Volatile Organic Compounds (VOCs) are released by human activities such as gasoline and solvents. Nitrogen oxides and VOCs react and form highly reactive secondary pollutants in the presence of sunlight. These emissions combine with primary emissions to form smog. The reactions create tiny airborne particles, surface ozone (O3), sulphur-dioxide (SO2) nitrogen dioxide (NO2), Carbon Monoxide (CO) and affect children, senior citizens and vulnerable population with severe health problems. Rapid industrialization, urbanization and use of vehicles release harmful gases resulting in outdoor air pollution. The properties of gases such as solubility, concentration and size determine penetration into the respiratory tract. Burning of fossil fuels such as crop, wood, waste and dung lead to indoor air pollution producing allergies. Metal and radioactive particles may result in severe non-communicable health problems (WHO 2006). Indoor air pollutants are more concentrated than outdoor air pollutants because the small area covered by the pollutant exerts effects very rapidly; therefore, the pollutants are scattered more efficiently in a limited area and easily penetrate the human body from their origin. Hence, indoor air pollution is more dangerous than outdoor air contamination. Weather and geography affect the location and severity of the magnitude of the pollution. The temperature regulates the length of time taken by smog formation and may occur more rapidly and severely during sunny days. When temperature inversions occur and the wind is calm, smog may remain trapped over the area for a few days. As traffic and other sources add more pollutants to the air, the smog gets worse.
London smog consisted of SO2 resulted in approximately 1200 deaths within a year while 6000 deaths were reported due to Bhopal gas leak of 40 tons methyl isocyanate. Recently similar pollution accidents were noted in Delhi when the emergency measures need to be maintained by temporarily shutting down all types of smog releases to control the emissions. SOx concentration was found more in urban areas, but later this gas reached rural areas as the study revealed that the daily mean concentrations of SOx had fallen 1000 to 500µg/m3.
Large developed chimneys help to transport pollutants’ dispersal widely and concentration fell to 25µg/m3. The correlations among criteria pollutants (NO2 vs. CO; NO2 vs. PM2.5; NO2 vs. PM10) from 2004 to 2009 vary annually and spatially from site to site, indicating the heterogeneous nature of air mix in Delhi. Significant PM10 concentrations were initiated by roadside dust, industrial emissions and long-distance transport from the Thar Desert during summer time. Recent studies revealed that North Indian cities like Delhi and Lucknow are polluted predominantly by particulate matter. NO2 and SO2 concentrations have decreased mostly due to fuel switching and more industrial controls. However, aerosol concentrations emitted from sources such as vehicular, industrial emissions, road dust, and crop burning, domestic, or construction activities, are on the rise with ever increasing population and urbanization. The highest level of PM10 (200µg/m3) was measured in residential areas of Lucknow which is above the limit (60µg/m3) prescribed by central pollution control board, indicates distinct seasonality during winter months. However, the concentration levels of SO2 (8 µg/m3) and NO2 (30 µg/m3) are at permissible limits. The pollutants enter into the deep alveoli of the lungs and also may damage the brain barrier. The Government of India had taken severe action up to closing the schools to shut down coal and chemical factories that release smog. These data show that currently air pollution has become a severe problem, especially in developing countries which results in non-communicable disease such as ischemic heart disease, stroke, COPD, lung cancer etc and increase the risk for disease in 75% human population.
Carbon monoxide is known as silent killer as it is difficult to detect. LAugessele and Fardeau (1967) reported the association of neuropathologic damage with CO as evidenced by globes pallidus lesions, white matter changes and diffuse low-density lesions in the brain. Even the room temperature level, CO emission is highly toxic which affects the sense organs like brain and heart leading to several disorders. Very low levels of COHb (<5%-10%) were detected in smoking persons. CO enters into the organism and combines with haemoglobin which occupies the oxygen carrying capacity thus decreasing organ functions. Severe CO toxicity may induce tachycardia and tachypnea by cellular hypoxia. CO exposure produces morphological changes in the myocardium and lowers skeletal muscle function due to cytochrome oxidase inhibition. Tissue injury and ECG results verified the mortality in hospitals.
Nitrogen dioxide plays a major role in the atmospheric reactions that produce ground-level O3 or smog. The health risk factors are directly or indirectly dependent upon cooking practices in most crowded places in a small area. Short term exposure of NO2 leads to a greater risk for hospitalization rate and diagnoses for cardiovascular disease (CVD related mortality (69%), pulmonary disease (28%) while its combination with 10 µg/m3 PM2.5 increased cardiovascular mortality rate. The combined short-term effects of PM, O3 and temperature were observed in 70 subjects suffering from diabetes mellitus by examining systolic and diastolic blood pressure. The blood pressure was elevated due to the PM induced rise in myocardial oxygen demand. Early population based cross sectional studies indicated that the mortality rates with long term effects depend upon the concentration of pollutants. Physical activity reduced the mortality frequency with CVD deaths (Lear et al 2017). A monitoring program was held in 11 fitness centers in Libson and the parameters such as temperature and humidity, PM, CO2, CO and VOCs were monitored. The results indicated enhanced toxicity attributed to infections in the respiratory tract and inner parts of the nose. Acute lower respiratory infections diseases occur above the epiglottis such as pharyngitis, laryginitis or rhinitis. The daily counts of health-related incidence and population of the monitors situated in the study area observed individual data of pollutants with approximately 1% increase in daily deaths with level of particulates. Ambient air contains various highly reactive pollutants such as oxides of nitrogen and oxygen which are inhaled with the particles and produce a severe effect on the tissue cells of the lung. Long term exposure to outdoor air pollution increases the risk of chronic respiratory disease leading to CVD. Alwahaibi and Zeka (2016) found allergic and acute respiratory health effects in young populations due to air pollution exposure. They defined allergic diseases as conjunctiva, dermatitis and eczema while acute respiratory diseases included upper and lower respiratory infections, pneumonia and asthma. This review is primarily concerned with examination of studies on some important criteria air pollutants including PM10, PM2.5, CO, NO2 and SO2 in terms of methodology and human health risk assessment. Pollutants and their adverse health effects with corresponding concentrations are presented in Table 1.
Material and Methods
The measurement of the degree of pollution using data for modelling and to measure the quantity and quality of any pollutant in a systemic way is known as a pollution monitoring method. Since the main objective of this review is to assure the health impacts of pollutants due to indoor and outdoor exposure, different techniques for different samples are required to measure the concentrations of the pollutants. Earlier the studies were simply depending on the changes in clinical implications as per the pollution effects. However, the studies after 1960’s were developed by population based cross sectional methods followed by mortality rates with long term and short-term effects. The research methods are based on evaluation of the daily counts in relation with hours to minutes by monitoring health-related incidence equipments. Pollutant wise methods for their measurements according to health impacts have been given in this section.
Particulate Matter (PM)
The particulate matter may deposit easily in different parts of the body and can spread to upper parts like nose and also penetrate deep into the alveolar region of the respiratory system. Measurements for particulate matter began in 1964 with simple statistical calculations. Later on, the methodology was developed and induced better PM estimations. The regression analysis for PM concentrations with reference to the hospital admissions indicated the increased admissions due to respiratory illness caused by PM10 emissions from steel mill (Pope III 1989). Since 1970’s to mid-1990, the PM effects have been calculated by studying the population-based observations, after that during 1970-1980, elemental concentration became a major source for mass balance. The CMB receptor was used for measuring the particulate matter to determine PM 2.5 and PM10 concentrations by different sources such as diesel, fossil fuel and vehicle exhaust. The sources like coal combustion (42%), vehicular emission (47%) were determined through CMB model and observed seasonal variations in Kolkata during 2003 to 2004. Karar et al.,monitored ambient PM10 mass concentration by atomic emission spectrophotometer and found higher concentrations in winter seasons. The 24-hour PM10 concentrations were analyzed by poison regression analysis model and gravimetric filter-based method with meteorological aspects. The scientists estimated the concentrations of PM10, PM2.5 and PM1 in indoor areas by using LUPED model. This model is based on the endotoxins concentration deposits in the cellular regions of the respiratory tract and its breathing rates at regular intervals of time. Particulate matter was also determined by low pressure three cascade impactor or Dektai impactor (www.dekati.com). Therefore, the analytical methods transformed from simple population calculations to fully scientific and economically skilled equipment, which gives better results to determine the effective concentrations.
| Table 1: Pollutants and their health effects along with pollutants’ corresponding concentration. | |||||
|---|---|---|---|---|---|
| Pollutant | Concentration | Health Effects | Reference | ||
| Particulate Matter (PM) | |||||
| PM10 | 100-299 µg/m3 | The exposure to air borne particles shows increase in mortality and morbidity. The particles can easily penetrate deep into the tissue like alveoli in the respiratory system and cause severe cardiovascular problems. Particulate matter has stronger effluence over the age of 65 cause respiratory deaths and also decrease in pulmonary function | Samet et al 2000 | ||
| PM10 | The typical range of about 102-105 cm2 and 1-100 µg/m3 increased 1.7% of mortality with 3.3% increase in COPD and 4% pneumonia deaths. | Dockery et al 2000 | |||
| 150 µg/m3 | |||||
| PM10 | 150 µg/m3 | The short-term exposure indicated the effects of daily levels of PM10 for CVD hospitalisation in daily life during 1995-2004. | Middleton et al 2008 | ||
| PM2.5 | 57 µg/m3 | The impact of PM2.5 concentration on the people leads to premature births. | Ritz et al 2000 | ||
| PM2.5 | 11-33 µg/ m3 | Mortality in 65 year aged persons was recorded more (0.64%) than the younger ones (0.34%) and diagnosed with the probability of respiratory diseases | Faustini et al 2013 | ||
| PM2.5 | 10-27% µg/ m3 | Clinical conditions especially in elder people and acute health illness were affected more with pre-existing diseases like diabetes and CVD | Zanobetti et al 2014 | ||
| PM10& PM2.5 | 10 µg/m3 PM2.5 and 0.74% per 14.4 µg/m3 PM10 | A 5- lag days increase 1.05% per 10ug/m3 in PM2.5 and 0.74% per 14.4 µg/m3 in PM10. It is associated that PM2.5 had a deep association with mortality than PM10 because of lesser size. | Alessandrini et al , 2016 | ||
| PM10& PM2.5 | 54.4 µg/ m3 | The epidemiological studies differentiated the complete attributable mortality and morbidity in the case of PM2.5 and PM10 in the 5years of period of time. | Dholakia et al 2014 | ||
| PM10& PM2.5 | 115 µg/ m3 | By increasing PM concentrations, the premature births had been reached to 0.59 million cases. | Lelieveld et al 2015 | ||
| PM10& PM2.5 | 120 µg/m3 PM10,100.2 µg/m3 PM2.5 | The concentrations of endotoxins with pollutants including environmental factors highly affected the houses where biomass fuel was used than LPG using houses. It was observed that the deposition of particulate pollutants found more in infants and children than in adults which caused 75% of endotoxins deposition in alveolar region. | Padhi et al 2017 | ||
| PM10& PM2.5 | 65.5µg/ m3, 153 µg/ m3 | The endotoxins of PM (PM2.5, PM10& PM1) are the major indoor air pollutants which can cause the respiratory problems. | Cifuentes et al 2000; GI 2015 | ||
| CO2, PM | 900-1500 µg/ m3 | Mainly children, women and elderly persons were observed with frequent illness, cough and other respiratory problems due to improper ventilation system which spread endotoxins rapidly. | Peters et al 2001 | ||
| PM10,PM2.5 | 56.3 µg/ m3, | Short term air pollution had increased the respiratory hospital admissions of all ages (0-65yrs). | Çapraz et al 2017 | ||
| & NO2 | 29 µg/ m3, | ||||
| 41.8 µg/ m3 | |||||
| Gaseous Pollutants | |||||
| Carbon monoxide (CO) | 3.69% | Higher COHb levels were found in the traffic police at junctions than the normal office staff; correlated with high mobility and mortality rate i.e. 400-500 deaths in 5 years (1999 to 2004) in US. | Nair et al 2017 | ||
| CO | 70% | In India, the traffic regions have dangerous effects because these are ground level sources, so it may spread easily. | Sood 2012 | ||
| CO | 2.55-4.98 µg/ m3 | Severe headache, cardiovascular disabilities, dizziness etc. CO exposure may lead to premature births in pregnant woman and low birth weight in new born babies. | Rudra et al 2010 | ||
| CO | 0.46-11.3 µg/ m3 | Attack in cellular functions, tissue injury and transmits in the central nervous system. | Atimtay, et al 2000 | ||
| CO | 33.1 µg/ m3 | Acute CO poisoning in blood samples which leads to myocardial perfusion. | Satran et al 2005 | ||
| CO | ≥ 500 µg/ m3 | Chronic exposure causes CO toxicity like general illness, flu based fevers and psychosomatic symptoms. The chronic toxicity is more because the CO levels leads to tissue damage and reduces oxygen carrying capacity. So it is very dangerous to sensitive parts like brain heart and lungs. | Parsons 2004 | ||
| CO | 8.7-87 µg/ m3, | COHb is dependent on its CO level and the way of exposure as well. The ambient air pollution with CO at 100ppm is more effected to health. | Townsend and Maynard 2002 | ||
| 100 µg/ m3 | |||||
| CO | 2.5-4.98 µg/ m3 | Toxicity in cellular level bonding refers oxygen carrying capacity of Hb is the major acute mechanism. Non-Smokers with high COHb levels were observed. | Nair 2017 | ||
| (0.008 µg/ m3-exposure as CoHb levels) | |||||
| CO | 100-400 µg/m3 (0.01%-0.04%) | Not only coronary but also causes the neurological problems. Disturbance in brain developing and functioning caused by CO toxicity. It induces the tissue hypoxia which affects the cerebellum. | Cho et al 2014 | ||
| CO | 13.6 µg/ m3, 48% of CO exposure | About 84% people were suffered from headache at 21.3% COHb level. | Handa and Tai 2005 | ||
| CO | 11-25 µg/ m3 | The headache is caused by chronic CO poisoning. COHb levels >30-40% causes dizziness, general weakness, fatigue and sleeping sickness. These symptoms can cause from days to months rather than 6 months. So mainly the CO effect can cause by long term more efficiently. | Abelsohn et al 2002 | ||
| (1-8hrs) | |||||
| CO | 0.5 µg/ m3 | Formations of COHb mechanism in blood streams may lead to coronary artery diseases. The CO diffuses from the alveolar capillaries through a membrane into the blood stream by diffusion method. The affinity absorption of CO to Hb is 210 times more than the O2. This mechanism affects the mortality by arrhythmia and heart attacks. | Prockop and Chichkova 2007 | ||
| Nitrogen dioxide (NO2) | 30-90 µg/ m3 | Serious lung damage with a delayed effect, shortness of breath and chest pains. | Katsouyanni 2003 | ||
| NO2 | 0.62 µg/ m3 | Increased NO2 concentration increases lower respiratory infections and also increases asthma in children. | Adams et al 1987 | ||
| NO2 | 0.053-10 µg/ m3 | Patients of asthma and COPD cause rapidly responsiveness to NO2. Traffic and indoor air pollution cause respiratory illness, bronchitis etc | Bauer et al 1986 | ||
| NO2 | >200 µg/ m3 | Higher level exposure causes cough, chest pain, vomiting and headache affects tachycardia, radiographic bilateral pulmonary functions etc. | Hedberg et al 1989 | ||
| NO2 | 50-100 µg/ m3 | Asthmatics are susceptible to long term of NO2 pollution. | Mayorga 1994 | ||
| NO2 | >100 µg/ m3 | Acute and chronic exposure of NO2 was observed experimentally showed greater mortality by inducing bacterial and viral infections. | Folinsbee 1993 | ||
| NO2 | ≥ 40 µg/ m3 | NO2 causes the increment in asthma by 3.1%. | Weinmayr et al 2010 | ||
| Sulphur-Di-Oxide (SO2) | 1-2 µg/ m3; | SO2 is one of the pollutants that can be more harmful due to the outdoor than indoor pollution, influenced by pollutant responsiveness. | Bell and Davis 2001 | ||
| Response concenteration-8 µg/ m3 | |||||
| SO2 | 1.5-13 µg/ m3 | SO2 concentration goes to peak while doing physical activity like jogging, exercise etc, and observed high SO2 concentration in oral breathing. | Frank et al 1969 | ||
| SO2 | 1-50 µg/ m3 | SO2 response gradually increases from nose to oral while doing mild to heavy exercise shows sensitivity of the pollutant. | Niinimaa et al 1980 | ||
| SO2 | 3-4 µg/ m3 | Relationship was observed for mortality based on physical factors and different seasons. | Fairley 1990 | ||
| SO2 | 19.2 µg/ m3 | At low temperatures and the low levels of air pollution the hospital admissions for asthma and CVD were observed in daily mortality. | Ponka and Virtanen 1996 | ||
| 830 µg/ m3 | |||||
| 65.7 µg/ m3, | FEV and FVC observed for the associations on mortality. | He et al 2010 | |||
| SO2 | ≥0.005 µg/ m3 | ||||
| SO2 | 10 µg/ m3 | Lower FEV1 by 54 ml. caused bronchitis, emphysema or asthma and respiratory illnesses in new borns and elderly people, but now young people (>16-35-65>) are also affected. | Forbes et al 2009 | ||
| SO2 | 19.2-23.3 µg/m3 | SO2 with association of PM shows higher sulphate levels in urban areas which caused lower FEV1 levels about 151ml. | Jedrychowski et al 1999 | ||
| SO2 | 4.2-27.8 µg/ m3 | The associations of TSP, TSO4 and SO2 affect the preadolescent children causing cough, respiratory illness etc. | Ware et al 1986 | ||
| SO2 | 2.29 µg/ m3 | The concentrations can induce hypothesis by inflammatory pathway to cause cardiovascular problems. | Alwahaibi and Zeka 2016 | ||
| SO2 | 3.9-4.13 µg/ m3 | Bond between the pollutants like sulphate with biological mechanisms leads to CVD. Two major traffic air pollutants (SO2 & O3) have marked on inflammation, oxidative stress and blood coagulation in healthy humans. | Chuang et al 2007 | ||
Carbon monoxide (CO)
The effects of CO have been recognized in neuropathy logical studies in white matter in the brain through CT and MRI in the 1970’s. Later on, it was observed with the help of simple graphical experiments followed by identifying COHb levels. The COHb levels in the pregnant women who had smoked habit were observed 1.8 times greater than the normal blood level. The levels of CO in tissue were examined by Red Cell Mass in 32 participants and > 6.8% CoHb, 82.3 kg RCM levels were recorded in smokers while <2% CoHb, 73.6 kg RCM levels in non-smokers. The CO levels were also estimated in about 30 patients of middle and older age, which had ischemic heart disease with the hypothesis on ST depression, angina and maximum exercise sessions Around 40 male subjects with myocardial ischemia disease were examined through electrocardiographic changes and results showed reduced COHb levels in the range from 0.6% to 0.3% and decrease in subendocardial thickness end point and angina before and after exercise tests [1]. Another study was based on 30 ventricular ectopic beats hour-1 over 20 hours upon coronary artery disease. After exercise the ventricular ectopic beats were recorded non-significant in arrhythmia frequency. The patients having non recognizable COHb levels were examined by different symptoms for effective treatment. The symptoms hypothesized as CO effect were examined through a simple questionnaire based on the tool named CH2OPD2 mnemonic and sequential questionnaire to obtain an environmental exposure history. The cross-sectional studies on the blood samples of 708 subjects experienced the analysis of head space capillary gas chromatography, mass spectroscopy with an HP mole sieve plot column. The correlation between CO exposure and carboxyhaemoglobin was analyzed through regression models indicated that COHb concentration increased by 1.29% to 10% increase of CO exposure. The blood samples of a group of 30-40 yrs aged traffic police were compared with the same age persons of a hospital for about 2 yrs through spectrophotometer and Mann-Whitney U test to determine the difference in CO toxicity. The scientists had developed the scientific techniques according to increasing concentration and varieties of sources and found that time series analysis is the most suitable model to predict the CO concentrations. On the other hand, the removal analysis of CO toxicity is becoming advanced technique now-a-days; Norma Baric Oxygen therapy is the method to eliminate CO toxicity from the patient. Empirical mode description (EMD) was used to calculate the suicide population in association with air pollution and weather variables as one of the factors (Yang et al 2011). Therefore, these studies prove that CO affects not only the blood serums, but other systems of the body are also affected.
Nitrogen dioxide (NO2)
The effects of long term NO2 exposure were identified by using different lung models and cultured cells, regression models and diagnosed with tissue injury. NO2 responsiveness to asthmatic patients was observed for 30 min. exposure in four days and found SRAW at 0.05 p.m. of the pollutant level (Bylin et al 1988; Mohsenin 1988). They also observed 40% decreases in PVP by inducing methacholine. The analysis of lung parameters Fev1, Fec and specific airway resistance of NO2 exposure revealed acute responsiveness (Mohsenin 1988). The asthmatic subjects were exposed to 0.30 ppm NO2 concentration after exercise on treadmill with resting time of 10 minutes and revealed increased SRAW but decreased Fev1 and Fec. (Roger et al 1990). As an indoor air pollutant, NO2 can affect sometimes in short terms and long terms as well. Long term exposure (4 years) to high levels of NO2 concentration (>40 µg/m3) affected 5758 children diagnosed with lung functioning parameters and skin prick tests resulted decreased lung function.
Sulphur dioxide (SO2)
The breathing patterns of the responsiveness of SO2 were examined through a simple questionnaire survey of selected areas such as Nashville and its suburban fringe. The Oesophageal cathedral method was applied on 8 male subjects to examine pulmonary flow resistance and lung volume through gas compression method. The studies on the effect of SO2 on broncho-constriction through SRaw revealed that the induced SO2 stimulates bronchi construction in persons affected with mild asthma while hyperventilation induces the increasing bronchi construction. The association of compound mucous cilia with SO2 exposure was observed through the biological marker and revealed that SO2 caused the epithelial tissue injury (Carson et al 1986). The data of suspended particles like sulphates, nitrates and mortality of the Santa Clara county, city were correlated with relative temperature, humidity and seasonality by a regression model to determine the effectiveness of the pollutant. The poison regression, autocorrelation analysis of 15 European cities with a population count, concentrations of black smoke, nitrogen dioxide and ozone revealed that meteorological variables affect the air quality and observed the SO2 concentrations ranged approx. 30-300 µg/m3 could lead to positive association with daily mortality in highly polluted years of Athens (1984-1988) through auto regression model with 1-day log. Comparative studies on associations of pollutants had been conducted by many scientists recently. The cross-sectional studies of >16yrs (1995 to 2001) revealed SO2 concentration approximately 10 µg/m3 correlated with 54 ml of Fev1 in individual caused lower rate of lung function. Fev1 and Fvc were measured by Spirometer and statistically analyzed by chi-square test and variance of the post and present estimations. The association of SO2 and PM affected around 1414 persons who lived in higher sulphate and STR (Sulphur transformation ratio) area with lower Fev1 levels by 151 ml. The effect of SO2 concentration (151-350 µg/m3) on lung function growth in about 1001 preadolescent children of 10 to 12 yrs age was observed in Cracow and Poland by measuring Fvc and Fev1 for 2 years through spirometric and multivariate model analysis (Jedrychowski et al 1999). The study of biological mechanisms through Mann-Whitney method revealed the effects of SO2 and inflammatory markers, oxidative stress, fibrinogen, coagulation factors were measured by Elisa based method. Blood samples of diabetic patients were analyzed for different parameters such as CRP, Glucosamine, HbAc, haemoglobin over 3 weeks. The data were analyzed with the association of pollutants and meteorological factors statistically by Spearman and Pearson correlation co-efficient (Chuang et al 2007).
Results and Discussion
The increasing population along with industrialization and urbanization are the major causes to modify the efficiency of the pollutant concentration as the effects of pollutants can be seen even in a short period of time. However, all the diseases which are affecting the people from several microorganisms, but its productiveness can depend on the increasing pollutant concentration. Depending upon the efficiency of the diseases, it is classified into Physiological and Psychological diseases in this study. The effects of the diseases related to individual pollutants are discussed here within these two categories.
Physiological diseases
Health problems related to respiratory system due to major pollutants prevents the oxygen binding capacity with the blood, PM cause inflammation in the lungs; NO2 causes respiratory infections, especially in children and increases chronic respiratory diseases including shortness of breath etc. On the basis of reviewing peer reviewed papers of each pollutant, it was found that physiological diseases occur due to pollutants are CVD, COPD, Asthma, Diabetes and Cancer. Therefore, it is necessary to identify potential pollutants’ correlation with the diseases.
PM10 and associated physiological diseases: Previous studies reveal that the mortality due to PM concentration may be evidenced mainly through the criteria of observing hospitalization. Hospital admissions due to PM caused the pulmonary inflammation triggering systemic hyper coagulability increased the heart rate leads to myocardial infarction followed by heart attack and high risk of CVD mortality. The postmenopausal women have been seen suffering from obesity due to the 10 µg/m3 PM exposure and found with 76% increased risk in mortality due to CVDs. The associations of various pollutant effects on hospital admissions due to CVDs have been increased by 2.79% per 23 µg/m3 PM10 and 1.66 µg/m3 CO concentrations. Some studies revealed that PM affects middle aged persons and caused CVDs and observed with a tremendous increase in C - reactive protein, a protein produced by liver shows the presence of inflammation and breast cancer. PM10 caused CVD, COPD and pneumonia diseases observed through hospital admissions due to vehicular pollution. Long term exposure to PM10, O3, NO2 and SO2 can cause hyper coagulability and thrombosis due to adverse effects on ATPP, PT, CRP and tissue type plasminogen activator (t-PA) etc. which leads to CVD. PM exposure above acceptable levels in persons working in photocopy shops felt very high nasal blockage and other lung infections resulted CVD issues. Urban air pollution exposure caused hypermia due to high level of PM10 and PM2.5 concentrations and exaggerates the response of small arteries to cardiac ischemia. Association of PM10 and NO2 long-term exposure was reported the decrease in lung volume and airway resistance in children examined by spirometry. The comparative study of LPD and HPD was revealed the high-risk asthma, changes in the FEV1, FEF and other respiratory problems in children. The emergency visits for asthma were strongly increased due to PM10 and PM2.5 exposure.
Particulate matter plays a vital role in morphological changes which increases the risk of non- malignant respiratory diseases and IHD . PM10 was recognised as a specific pollutant among other pollutants indicated a significant role in increasing COPD admissions in winter season and asthma in warm days. Elevated levels of PM10 concentration were reported the cases of CHF. It was found that 10 µg/m3 increased by 0.72% (0.35%-1.10% at 95% confidence interval) increase the rate of admission of CHF. An association of particulate and gaseous pollutants caused blood coagulation factors like prothrombin time, activated partial thromboplastin, fibrinogen etc. risk in women. The InterLeukin-6 expression in around 430 children was found higher with more exposure to PM2.5 (45.38µg/m3) and PM10 (80.07µg/m3) while TNF-alpha were reported due to PM emission through vehicles followed by pulmonary illness. The strongest association of PM10 and FVC was reported in a European study of Cohorts of Air pollution effects based on long term air pollution levels in a standard manner. Hospital admissions of the cases of COPD in above 65yrs aged patients indicated positive associations with PM10.
According to emergency visits to hospital with acute respiratory diseases in 65yrs age female had a higher risk of acute COPD due to exposure of association of PM10 and SO2 with meteorological properties, showed prominent IQR range, i.e. 28.3µg/m3 and 7.8µg/m3 respectively. The concentrations of PM2.5 and PM10 in the form of Asian dust (AD) were detected by LIDAR in 231 adults’ asthmatic patients found with reduced lung functioning by PEF. The study on short term exposure of traffic related pollutants reported the increase in CVD and respiratory hospital admissions while Long term exposure of PM10 to middle aged women caused a 13% increase in COPD . Even low level of air pollutants’ association below the Environmental Protection Agency standards (PM10 & NO2) showed the association with chronic respiratory diseases in adults and 15% increase in children’s hospitalizations. The association of air pollutants PM10, NO2 and CO caused an increase in the visits of Allergic Rhinitis (AR) in winters while the association of short-term exposure of PM10 and SO2 showed increased FVC and FEV1 levels [2]. Weather variables were also found as a predictor of increasing COPD admissions.
There is no direct evidence on the effect of particulate matter on diabetes, however, the nurses living in residential places near the roadways were examined with little association and effectiveness. Around 54-55yrs old women were diagnosed with subclinical inflammation added to PM relate type-2 diabetes and was observed stronger in women than men. Low socioeconomic status had a higher risk of diabetes with PM10 association. Long term air pollution with two pollutant model which is experimental evidence found with limited epidemiological evidence for diabetes mellitus.
PM2.5 and associated physiological diseases: The fine particulate pollutant (PM2.5) enters into the deep alveoli in respiratory symptoms while the ultra-fine particles (PM1) reaches into deep cellular regions and lymph nodes mixes with the blood. Short-term PM2.5 (10 µg/m3) exposure led to 13% increase in CHF admissions, the risk of ischemic stroke and cerebrovascular diseases. The association of PM2.5 and NO2 caused the supra ventricular tachycardia, which increases risk of heart arrhythmia. PM2.5 emission was observed as the reason for the increased levels in urinary 8-hydroxy the oxygenation concentrations in 110 inspectors at diesel vehicle inspection station. PM2.5 effect was observed as oxidative stress in asthmatic patients with the exchange in neutrophils indicated high oxidation of plasmatic lipids causes decrease in defence mechanism in human blood. Traffic exposure was found to elevate endotoxin in 1yr old child caused the development of allergic wheeze conditions. An increment of 10 µg/m3 in PM2.5 concentration was found associated with an increase in ERV1 based URTI, LRT and AECOPD. People working at Oxford Street for 2-4 hrs showed decrease in FEV1, FVC in asthmatic individuals due to association of diesel traffic exposure. Long term traffic exposure of PM2.5 to a population-based study showed increased levels in CIMT (a marker of subclinical atherosclerosis),TNF-alpha, fibrinogen, PA-1, t-PA, Soluble platelet selctin, t-Hcy (blood markers of inflammation and blood coagulation) leads to cardiovascular and respiratory issues. The pollutant exposure to the children (0-17yrs) caused asthma showed stronger association in winter season. The cases of hospital admissions due to PM2.5 associated with organic carbon was found more associated with URI and pneumonia while traffic related PM2.5 had lagged association with asthma in children and COPD in adults. The throat diagnosis of coronary angiography indicated the PM2.5 as a risk factor for stroke in residents (Hartiala et al., 2016). PM2.5 along with particle bound Polycyclic Aromatic Hydrocarbons and 8-hydroxy-2’deoxyguanosine level caused PM induced DNA damage and inflammatory responses in the lungs. The impact of particulate matter exposure revealed the low level of TNF- alpha, IL-10 with the association of suppression of Th1-Thr caused development by allergic and autoimmune diseases in the adolescents of starazagora. Fifty-seven adult asthmatics with a source of PEF were found with the association of 5-day average PM2.5 concentration (1.3 µg/m3) and average 1.14 L min-1 decreased level of PEF in the evening. PM2.5 and chemical constituents like EC, OC, silicon and sulphur etc. were found strongly associated with increased arthrosclerosis. The effect of long-term air pollution on resident population lived nearby 50-200 m highly traffic areas were reported the decrease in ankle brachial index and peripheral arterial disease, especially in women. The longitudinal cohort study of survival models associated with PM2.5, an attributable factor indicated the risk of diabetes mellitus due to long term exposure of PM2.5 while another study of 44 aged patients reported hypertension and diabetes. PM2.5 with NO2 may increase the risk of hypertension in diabetes women obesity, CVD may be suspected to increase the diabetes in non-smokers also. Long term air pollution with the incidence of acute coronary syndrome patients had increased the risk of STEMI due to particulate air pollution; later on, people were at high risk of CVD. PM2.5 exposure can play a prominent role in increasing type 2 diabetes as it has adverse effects on glucose tolerance, insulin activity and blood lipid concentration which increases the diabetic activity. High levels of BP and BMI resulting from high concentration of NO2 and PM2.5 exposure ensured high risk of type-2 diabetes, significant risk of lung cancer and respiratory disease [4]. The association of PM2.5 and NO2 caused high HbA1C levels, could be a risk factor for the imbalanced glucose metabolism in diabetic patients.
CO and associated physiological diseases: The carbon monoxide is a poisonous gas mainly emitted from vehicles causes primarily severe headache, cardiovascular problems, premature births, low birth weight in newborn babies, dizziness, etc. Increasing levels of CO concentration was correlated with decreasing BP and other health effects like headache, dizziness and slight fever etc. The binding mechanism of CO with Haemoglobin (Hb) forms cell affinity of oxygen molecule called hypoxemia which inhibits the oxygen binding capacity caused gasometrical and respiratory issues. Increasing Serum Ischemia modified albumin is a diagnostic biomarker in blood COHb showed positive association of CO poisoning. Another source of CO pollution caused diseases is smoking habits. The researchers studied about different smoking units with the help of simple questionnaire and biochemical markers were used to validate levels of nicotine, thiocyanate and CO concentrations. Bilirubin was found as a key enzyme of lipid oxidation formation of oxygen radicals. The CO with low blood plasma concentration affects the bilirubin may cause high risk factor for ischemic heart diseases, CAD related diseases and arteriosclerosis etc. which leads to high morbidity and mortality rate. CO pollution affects the Coex levels, is a simple surrogate biomarker related to wealth consequences. Coex levels were found higher in smokers than non-smokers in rural and urban areas and may associate with increased risk of myocardial infarction, respiratory infections and other diseases. Recent studies on the direct effect of CO on lungs is very less, however, the association of CO with other pollutants has been reported. For instance, the association of CO with NO2 and PM effects as inflammatory with COPD, exhaled CO with MRI measures lead to increase the risk of stroke and different cardiovascular problems, metal concentration with CO causes severe diseases such as hypertension and anaemia, etc.; oxygen and CO poisoning caused cardiovascular squeals in 37% of patients. The association of outdoor pollutant mainly PM10, NO2, CO and O3 with CVD was observed as CO (0.9ppm for 8hrs; 6.0%) and NO2 (5.1ppb for 24hrs; 6.9%) increased the risk of cardiac failure (CVD). This result indicates that low concentration of CO shows the least effect, but with high intensity and prominent effect of COPD admissions in hospitals. The people working in various toll plazas and signals and roadside shopkeepers was exposed to CO higher than the WHO’s permissible level were diagnosed with depression, tidiness, fatigue, forgetfulness, respiratory problems with a high pulse rate and low oxygen levels. CO showed significant association of North Atlantic Ocean with meteorological properties and reported with heat stress and coronary diseases which indicated a prominent risk for CVDs [4]. The number of emergency visits under CO and NO2 exposure was associated with 2%-3% increase in COPD while other combination of CO with O3 also reported increased COPD admissions and asthma.
Outdoor air pollution, mainly traffic related pollution increased haemorrhage stroke while another study reported acute myocardial infarction. Weak association was recorded between pollutants and cerebrovascular diseases by two pollutant model (CO & NO2). CO (0.1ppm) was correlated with a 3.6% increase of IHD admissions in association with CHF and arrythrimia (Mann et al 2002). Increasing distance with traffic related air pollution reduced the mortality rate with acute HF and increased CVD mortali. Long term and short-term air pollution showed increased inflammation by increasing ferritin and WBC counts. On warm days, the CO toxicity is responsible for increasing hospitalization due to allergic rhinitis. An increase of COAD (chronic obstructive airway disease) emergency hospital admissions was found from the short-term air pollution at All India Institute of Medical Sciences hospital, Delhi.
NO2 and associated physiological diseases: Average and peak concentration of NO2 penetrates deep peripheral bronchi leads to mild and moderate type of asthma. High annual mean temperatures altered the interaction of NO2 exposure to ambient air increased the risk of allergic rhinitis and asthma in traffic police and roadside shopkeepers, airway resistance and induced allergic sensitization also reported in 2 months to 4yrs children. Asthma related factors were also associated with hand eczema (Lindgren et al 2009). Around 114 asthmatic children of 7-12 yrs age examined due to increase in upper respiratory infections even at relatively low levels of pollutant exposure. Increased ED asthma visits were reported due to high NO2 concentration and the effect of meteorological properties particularly in cold season [5]. Diesel exhaust was seen as a source of the reduction in lung function, airway resistance, airway acidification and neutrophilic inflammation effects in asthma patients. Exhaled nitric oxide (eNO) affected the airway inflammation and other biomarkers were also observed with enhanced allergic conditions in 6-15 yrs children. 200 Association of traffic related PM and NO2 caused COPD mortality and lung cancer. A positive association of NO2 and pollen was observed with increase in asthma emergency admissions . On analyzing the pollutant exposure with two pollutant model, the CVD effects were observed through the measurement of hsCRP (High sensitivity c-reactive protein), bow like biomarkers which were associated with the inflammation. Lower pulmonary function was diagnosed due to increasing emissions from a local coal fired station even in limit of pollution standards in Hadera, Isreal.
The study designed by the generalized additive model used in the association of traffic related air pollutants with hospitalization on an AMI, an 11 % increase in COPD was observed in cold season due to NO2 exposure correlated with meteorological factors and reduced expiratory flow. Outdoor air pollution and asthma fluctuations associated with lung function with high levels of motor vehicle emissions (NO2, SO2, CO etc.) leads to lower pulmonary function. Morning Fev1 measurements were found with the strong effectiveness of pollutants like NOx and O3 indicates lower lung function (Nkosi et al 2016). Short term traffic related NO2 along with other pollutant concentration promotes cardiovascular and respiratory mortality, COPD and lung cancer mortality (Atkinson et al 2016; Brunekreef et al 2009). The study of short-term exposure of NO2 in association with PM10 caused acute lower respiratory infections in young children. Long-term air pollution affects living beings near major roads which are high risk to COPD mortality. Among the lag of 0-5 days about 3.95% increase in respiratory mortality with NO2 exposure. Traffic related NO2 was observed as a cause of diabetes mellitus, especially in women, however, healthy non-smokers were also found with high level of glucose. Around 30.6 ml lower FEV1 measurement had been identified in a large cohort study due to NO2 exposure. The number of emergency visits with NO2 and CO exposure was associated with 2-3% increase COPD cases. Short-term exposure of NO2 (2.67%) showed an association for increasing CVD also correlated with diabetes (3.5%). Ten Italian residents had diabetes and other chronic diseases with an increase of 10ug m-3 NO2 exposure and type2 diabetes diagnose due to the traffic related buffer (250m) with NO2 exposure while 100m traffic buffer caused high risk of increasing Atherosclerosis. High levels of HbA1C and FBG were observed with 5 µg/m3 of NO2 exposure in Taiwan. Traffic related air pollution with the PM and NO2 exposure in the association of incidence of C3c marker used in the inflammation process caused a risk by increasing diabetes. Long term exposure of NO2 with PM is a higher risk of chronic diseases like CVD with diabetic mortality
SO2 and associated physiological diseases: The concentration of SO2 in ambient air depends upon meteorological conditions. The risk level of SO2 is 0.3 µg/m3, which may affect the human health by causing asthma, bronchitis, airway inflammation, breathing difficulties psychiatric alterations, heart failure, circulatory collapse, etc. A spirometric air pollution monitoring program reported cough, lower respiratory illness and bronchitis due to the exposure of TSO4, TSP and SO2 with CO. There was 200 ppb of SO2 and 400ppb of NO2 in 4 to 6 hrs responded mild optic asthma and increased plasma viscosity in men and women with meteorological properties while Fev1, FVC and CBU (Cumulative breath units) levels decreased after exposure to combined pollutants. The heavy traffic enhances the airway response to inhaled allergies possibly as a result of airway inflammation by the combination of SO2 and NO2. 100 The association of air pollution, especially SO2 and suspended particles caused an increase in blood pressure (1.79 mm Hg per 80 µm/m3 SO2), lipid peroxidation, which may alter antioxidant enzyme activities to sensory evoked potentials. In the coal burning areas, the effect of PM and SO2 concentration responded on vitro and vivo relations to neuron degeneration and positively correlated with the risk of neuronal dysfunction and increased in morbidity from COPD. SO2 pollution causes brain inflammation and related micro vasculature dysfunction. The action of endogenous 2-AG suppress the inflammatory related micro vasculature dysfunction. The receptors CB1 and CB2 can be used in medication of brain injuries due to SO2 inhalation.
The effect of SO2 on mortality depends on temperatures except with humidity. At a minimum temperature (<20ºC), the SO2 concentration may increase the COPD admissions, PC20 Methocholine may not be controlled, but reduced effectiveness of lung function increased the asthmatic conditions. Asthma ED transport visits were reported more in cold season from 73ppb SO2 exposure. 199 Around 5416 Ohio Medical cases were diagnosed with about 35% increase of asthmatic conditions correlated with 50 µg/m3 SO2 concentrations. The daily ER visits were recorded as 6% increase in asthma and 5% of COPD correlated with ambient SO2 exposure. Early pregnancy and preconception with ambient NOx and SO2 exposure leads to increase the risk of Gestational Diabetes mellitus. Association of pollutants such as PM10, NO2 and SO2 with fasting blood glucose led to increase the FBG levels. 10 µg/m3 SO2 exposure showed increase in lipid levels like Total cholesterol, Triglycerides and Low density lipoprotein cholesterol etc. especially in women and elderly people, which is a sign of risk of Diabetes. The annual mean concentration of SO2 revealed lung cancer and respiratory mortality in Japan and cancer in Stockholm, Sweden.
Psychologically the effectiveness of behavior is known as stress or depression. Psychological stress influences humans in two ways the amount of sadness, self-pain, bad incidents, sad thoughts and other as emotions cause depression. Hypotension and low lipid level have been associated with the depression symptoms especially in adults. The research of air pollution on human behavior started from the 1970’s, its conceptual framework for future research based on the relationship between air pollution with human behavior may very hypothetically. The high level of concentration of pollutants affects the physiological process may cause stress. Psychological stress may act as an environmental disruptive pollutant that affects the human health. However, very less research done on pollutants’ effect on stress and depression, but on the basis of discussion on the interactions, physiological diseases such as dementia, depression and stress are being discussed in this section.
PM10 and associated psychological diseases: The increment in suicide risk showed positive correlation with the exposure of PM10 is one of the evidences of the pollutants affect caused depression. Exposure to pollutants like SO2, NO2, PM10 and CO increases the ED visits for depression with CVD, asthma and diabetes etc. Korean version of the SGDS-K was used to measure the symptoms of depression to know the pollutant concentrations with various diseases. Some pollutants (e.g. PM10 associated with O3) have indirect effect and caused dementia. Long term pollution increases the dementia with Alzheimer’s symptoms like memory impairment and communication impairment, etc. Traffic related particulate pollution in elderly people shows the symptoms to become transition state between aging with dementia and Mild Cognitive Impairment). Air pollution causes acute epidemiologists stress by increasing psychological disorders. Urban pollutants affect the plasma levels and ACTH hormone which promotes psychosocial stress in non-smoking police officers. Effect of ambient pollutants influences suicide risk in low educated, white collar and married people. Association of traffic exposure with APOE decreases in cognitive impairment.
PM2.5 and associated psychological diseases: The depression was noticed in large population-based nurses, due to impact of PM2.5 at 0-45 depression scale. A positive correlation was observed between long term exposure of PM2.5 and socioeconomic stress signified the symptoms of psychological diseases like moderate to severe anxiety and depression. Another study proved the positive association of PM2.5 exposure with stress, even by controlling age, gender, demographic and socioeconomic health status. Stress toxicants can influence disease risk in immune function, lung structure and its function, etc. Asthmatic children were identified with stress by measuring blood markers (IgE, interleukin-5, interaction beta etc.) which indicated higher chronic stress. Social environmental status (SES) reflects from poor asthmatic conditions. The highest level of stress was associated with chronic stress and statistically evidenced with the pathways between SES and immune response in children having asthma (Chang et al 2014). National life, Health and aging project observed the association of air pollutant exposure with erectile dysfunction (a sign of psychological stress) in old age people enhanced the psychosocial, environmental stresses with air pollution increased the risk of CVD. Around 6.7% dementia was diagnosed in 67 older aged people with PM2.5 exposure. Individuals with CVD disease due to PM2.5 exposure associated with a 10.1% increase in stressful suicide risk. Air pollution with a positive association of poor cognitive function may intend to high risk for dementia [6].
CO and associated Psychological diseases: CO exposure also increases the risk of dementia substantiate with the study of vehicular exposure of NO2 and CO with increase of dementia cases in Taiwanese. High levels of diesel exhaust exposure of pollutants reported the symptoms of acute psychological stress. An association of HBO2 (Hyperbaric Oxygen) with CO exposure resulted out the declination in cognitive behaviour. ED visits were associated with correlation between CO concentrations and meteorological factors. Indoor CO exposure increased depressive symptoms in rural women because of the emission from kerosene stoves was found associated with higher cognitive impairment even at low level of acute CO poisoning [7]. A 43yr old woman was diagnosed with the cognitive impairment due to CO exposuRE.
NO2 and associated psychological diseases: From the neurological point of view, parasympathetic activity can cause inflammation. High concentrations of pollutants may cause psychological stress due to imbalance in different lifestyles. The pollutants’ concentrations (PM2.5, PM10 and NO2) were correlated with depressed mood of the people through validated questionnaires showed the effect of pollution on psychological diseases. Females were found with higher levels of depression than males due to NO2 and SO2 exposure (Blazer et al 2001). Each 10 µg/m3 level of NO2 increased the odds ratio of depression of 2:00 (95% CI; 1.37, 2.93) ranking with the use of antidepressant. In a chemical analysis of the population-based survey, dementia was diagnosed with is the effect of NO2 and CO exposure. Around 3 yrs follow up study on elderly persons resulted out the chronic and socioeconomic history led to increase the depression deaths Blazer, Hybels, and Pieper 2001). Parental stress is an outcome with NO2 exposure without smoking habit may lead to decrease in lung function. Increased temperatures along with increasing ambient NOX concentrations caused the risk of suicide Guangzhou, China. Even low-level pollutant concentrations would have increased the psychiatric admissions along with increased risk of suicide distress due to exposure of gaseous pollutants. The lower cognitive decline was associated with O3, NO2 and PM2.5 concentration in which NO2 exposure is inversely proportional to logical memory abilities. The mental development (prenatal/postnatal periods) in infants was affected with NO2 with Benzene exposure.
SO2 and associated psychological diseases: The long-term and short-term effects of low levels of SO2 exposure correlated with chronic stress, history revealed the mood distortions and stress followed by impact on physiological systems (Wang et al 2014). Short term exposure to air pollution affected the person suffering from physiological diseases had a high risk of depressive mood. The exposure to high levels of SO2, NO2 and PM10 to the pregnant women found with high levels of depression scores (i.e. P. -75-100) showed severe depression in cold weather. Linking mechanism of the air pollutant levels on suicide mortality increase the chances of depression. PM2.5, BC and SO42- concentrations were reported as higher Perceived Stress Scale (PSS) which is a marker of increasing depression and stress in people. Effect of air pollution between prenatal and postnatal was associated with parental stress increases childhood asthma. High levels of pollutant exposure to >30 yr age were found with increased stress and suicide mortality. Recently, a case of cognitive disorder was observed after the surgery remained exposed to PM2.5 and SO2 is a sign of increasing dementia .
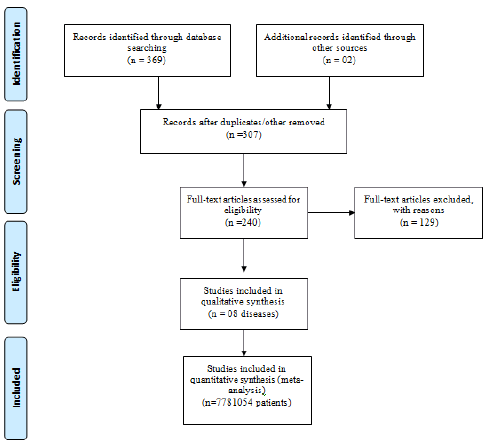
Characteristics of study objects: There were total 369 papers were accessed for conducting this review study. After exclusion of papers which were either repeated/ old information (n=60) or the study period was unknown (n = 02), research papers remained 307. Out of which, 60 papers were excluded for missing data on age, sex, mortality regarding physiological diseases (CVD, COPD, Asthma, Diabetes and Cancer) and 07 for psychological diseases (Dementia, Depression and Stress). In this way, only 240 papers were found eligible to consider for this review. Records of (1997-2019) years across the globe with an insufficient number of included individuals were also excluded (n = 22). The remaining 7781054 patients were included in the study. A cohort for the primary outcome, 2754056 patients had a valid record of physiological diseases and psychological diseases (with pollutants concentration and age), whereas methodology and results for physiological diseases (2088092) and psychological diseases (665975) included in the study of functional outcome. A detailed flow diagram is presented in Figure 1.
Review Interpretation
The present study is based on the interpretations of >360 peer reviewed research papers from international journals (all references are not mentioned in this paper). Out of which 40-50 research papers belong to each pollutant (PM2.5, PM10, CO, NO2 & SO2) and associated physiological diseases (CVD, COPD, asthma, diabetes & Cancer) along with psychological diseases (dementia, stress & depression). General review of air pollution and their health effects indicated two main groups of diseases, physiological diseases and psychological diseases. Physiological diseases may occur either from direct exposure of the pollutants or association of pollutants. On the other hand, psychological diseases are persuaded direct and combined with exposure of the pollutants or consequence of physiological diseases. The pollutant may affect directly or indirectly on endocrine glands, which spoils the hormonal system leads to neuropsychological diseases. Short term and long-term effects of pollutants on mortality and morbidity have been also discussed. Trends were analyzed for pollutants’ concentration levels over the years, associating of pollutants with different diseases and age-wise effect of diseases.
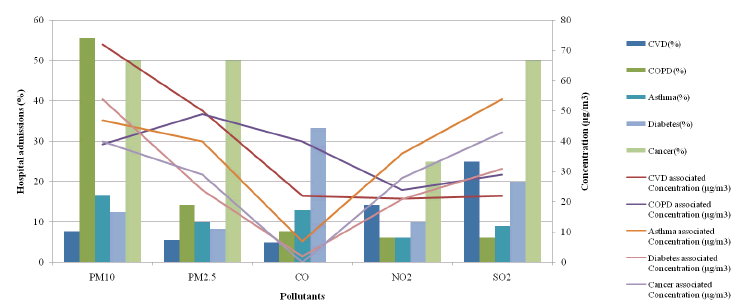
Figure 2 gives global overview of the diseases caused due to direct and indirect exposure of the pollutants. Largest hospitalizations’ cases of COPD (>50%) caused by PM10 followed by >15% cases due to PM2.5 exposure. Both types of particulate matter (PM10 & PM2.5) and SO2 are responsible for almost 50% cases of cancer. Fourth highest disease is diabetes as >30% cases are observed due to CO exposure. For the cases of asthma, almost all five pollutants are accountable but PM10 is the main contributor (15% cases). SO2 is the main contributor for CVD hospitalizations >20%).
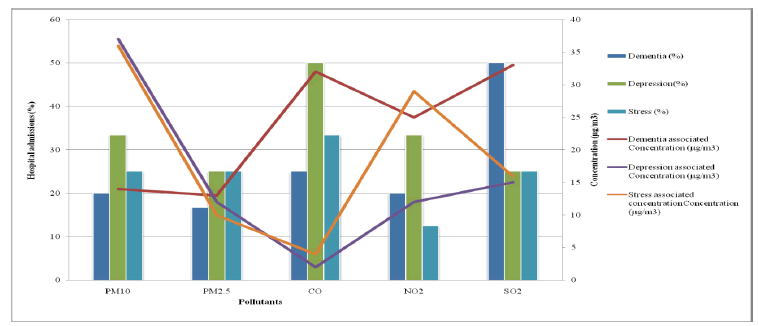
Figure 3 illustrates the pollutants’ effects on hospital admissions of psychological diseases with direct and indirect association of other diseases. CO and SO2 are the main contributors of increasing admissions of dementia (≤ 50%). CO is the prime pollutant that causes maximum number of psychological diseases’ admissions of depression. PM2.5 and SO2 are the second largest contributors of depression (25%). PM10 is the main pollutant concentration which causes nearly 40-50% of psychological diseases. PM2.5 (15%) is the least contributor of increasing psychological diseases. Stress was increased by PM10 (40%), NO2 (30%) and SO2 (≤ 20%) concentrations. CO and SO2 are the main pollutants which causes maximum percentage of Dementia. NO2 is the second largest contributor of depression [8].
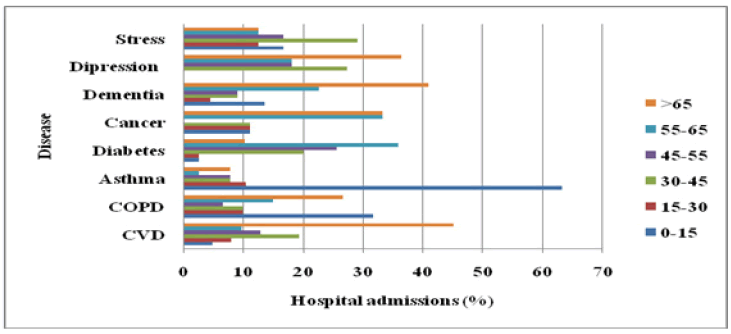
Age is one of the important factors of increasing its effectiveness. Figure 4 reflects the causing capacity of different age groups. The age group ≤15 years is very sensitive mainly for asthma (60%) followed by the cases of COPD (30%) and cancer (10%). Except diabetes, all diseases are prominent in adult group i.e.15-30 year’s age group; however, diabetes (35% in 55-65 age group) and CVD (45% in above 65yrs) are most abundant diseases after 30 years. The cases of cancer (35%) have been observed in the age ≥65 years [9].
Psychological diseases’ causing age is above 65yrs. Dementia is the main disease which occurs (≤ 50%) above 65yrs of age. 30-45yrs is the first highest age group for increasing stress while depression occupies highest percentage above 65 yrs age group, continuous reducing the effects above 45yrs. Stress affects around 30-45 yrs and it was observed that stress level is decreasing as increasing the age (45<55<65<65 above)[10].
Conclusion
The hypothesized analyzing of different pollutant concentrations upon different causing diseases is a clue for further studies on different aspects. The analysis of different age groups with pollutant associated diseases gave an overview to identify the intensity of diseases on susceptible groups. Among all pollutants, CO shows less effectiveness on Cancer and CVD while NO2 represented as a prominent factor for COPD hospitalizations for physiological diseases. Based on the concentrations there is enough study done on the effect of PM10 and PM2.5 pollutants. However, the effects of pollutants on psychological diseases need more rigorous studies on decisive health effects.
References
- Allard G, Nelson CJ, Pallardy SG. Shade effects on growth of tall fescue: II. Leaf gas exchange characteristics. Crop Sci. 1991;31:167-72.
[Crossref], [Google Scholar]
- Aekplakorn W, Loomis D, Vichit-Vadakan N, Shy C, Wongtim S, Vitayanon P. Acute effect of sulphur dioxide from a power plant on pulmonary function of children, Thailand. Int J Epidemol. 2003; 32:854-61.
[Crossref], [Google Scholar], [Indexed]
- Alderete TL, Habre R, Toledo-Corral CM, Berhane K, Chen Z, Lurmann FW, et al. Longitudinal associations between ambient air pollution with insulin sensitivity, β-cell function, and adiposity in Los Angeles Latino children. J 2017; 66:1789-1796.
[Crossref], [Google Scholar], [Indexed]
- Almendra R, Santana P, Vasconcelos J, Silva G, Gonçalves F, Ambrizzi T. The influence of the winter North Atlantic Oscillation index on hospital admissions through diseases of the circulatory system in Lisbon, Portugal. Int J Biometeorol. 2017; 61: 325-333.
[Crossref], [Google Scholar], [Indexed]
- Abe T, Tokuda Y, Ohde S, Ishimastsu S, Nakamura T, Birrer RB. The relationship of short-term air pollution and weather to ED visits for asthma in Japan. Am J Emerg Med.2009; 27: 153-9.
[Crossref], [Google Scholar], [Indexed]
- Ailshire JA, Crimmins Fine particulate matter air pollution and cognitive function among older US adults. Am J Epidemiol. 2014;180:359-66.
[Crossref], [Google Scholar], [Indexed]
- Amitai Y, Zlotogorski Z, Golan-Katzav V, Wexler A, Gross D. Neuropsychological impairment from acute low-level exposure to carbon monoxide. Arch Neurol. 1998; 55:845-848.
[Crossref], [Google Scholar], [Indexed]
- Adams WC, Brookes KA, Schelegle ES. 1987. Effects of NO2 alone and in combination with O3 on young men and women. J Appl Physiol. 1987;62: 1698-1704.
[Crossref], [Google Scholar], [Indexed]
- Alessandrini ER, Stafoggia M, Faustini A, Berti G, Canova C, Togni AD, et al. Association between short-term exposure to PM2.5 and PM10 and mortality in susceptible subgroups: A multisite case-crossover analysis of individual effect modifiers. Am J Emerg Med. 2016;184: 1-11.
[Crossref], [Google Scholar], [Indexed]
- Alwahaibi A, Zeka A. Respiratory and allergic health effects in a young population in proximity of a major industrial park in Oman. J Epidemiol Community Health. 2016; 70:174-180.
[Crossref], [Google Scholar], [Indexed]




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.