Health Status and Lifestyle Habits of US Medical Students: A Longitudinal Study
- *Corresponding Author:
- Dr. Brehm BJ
College of Nursing, University of Cincinnati, 3110 Vine Street, Cincinnati, OH 45221-0038, USA.
E-mail: bonnie.brehm@uc.edu
This is an open access article distributed under the terms of the Creative Commons Attribution?Non Commercial?Share Alike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Abstract
Background: Evidence shows that physicians and medical students who engage in healthy lifestyle habits are more likely to counsel patients about such behaviors. Yet medical school is a challenging time that may bring about undesired changes to health and lifestyle habits. Aims: This study assessed changes in students’ health and lifestyle behaviors during medical school. Subjects and Methods: In a longitudinal study, students were assessed at both the beginning and end of medical school. Anthropometric, metabolic, and lifestyle variables were measured at a clinical research center. Data were collected from 2006 to 2011, and analyzed in 2013–2014 with SAS version 9.3. Pearson’s correlations were used to assess associations between variables and a generalized linear model was used to measure change over time. Results: Seventy‑eight percent (97/125) of participants completed both visits. At baseline, mean anthropometric and clinical measures were at or near healthy values and did not change over time, with the exception of increased diastolic blood pressure (P = 0.01), high‑density lipoprotein‑cholesterol (P < 0.001), and insulin (P < 0.001). Self‑reported diet and physical activity habits were congruent with national goals, except for Vitamin D and sodium. Dietary intake did not change over time, with the exceptions of decreased carbohydrate (percent of total energy) (P < 0.001) and sodium (P = 0.04) and increased fat (percent of total energy) and Vitamin D (both P < 0.01). Cardiovascular fitness showed a trend toward declining, while self‑reported physical activity increased (P < 0.001). Conclusions: Students’ clinical measures and lifestyle behaviors remain generally healthy throughout medical school; yet some students exhibit cardiometabolic risk and diet and activity habits not aligned with national recommendations. Curricula that include personal health and lifestyle assessment may motivate students to adopt healthier practices and serve as role models for patients.
Keywords
Lifestyle, Medical school, Medical students, Nutrition, Prevention
Introduction
According to a recent report by the Institute of Medicine, [1] effective delivery of preventive strategies can improve health outcomes in the US more efficiently than treatment alone. Research has addressed the impact of physicians’ own health and lifestyle habits on their counseling practices related to health promotion and disease prevention. Study findings indicate that physicians’ personal health habits are consistent, important predictors of their patient counseling habits. [2-4] That is, physicians who engage in healthy lifestyles serve as role models and are more likely to counsel and motivate patients to modify unhealthy habits, such as poor diets, physical inactivity, and smoking. With the rising prevalence of chronic diseases, such as obesity and diabetes, it is increasingly important that medical school curricula include learning opportunities in lifestyle management and behavioral counseling for future practitioners. [5-8]
On entering medical school, students generally report healthier lifestyle habits than their peers. [9,10] However, the academic demands and challenges of medical school can make it difficult for physicians-in-training to maintain healthy behaviors over the course of their 4-year program, with potential adverse consequences on their physical and psychological health. [11,12] Studies have suggested a decline in physical activity, diet quality, life satisfaction, and general health during medical school. [11,13,14] In addition to long-term, detrimental effects on the health of these future physicians, there is potential for a greater impact on the health of the general public due to less frequent preventive counseling by physicians who do not “practice what they preach.” [15]
The vast majority of research on the health status and lifestyle habits of medical students comprises cross-sectional studies that rely on self-report surveys rather than clinical measures of cardiometabolic risk such as blood pressure and lipid profile. To the best of our knowledge, there have been no longitudinal studies conducted in the US that provide objective clinical evidence to support the hypothesis that medical school has a negative impact on personal health and lifestyle habits. The aim of this study is to assess changes in anthropometric and metabolic parameters along with nutrition and physical activity habits in students from their 1st to 4th years of medical school. The results will be useful in guiding future curricular changes to improve and sustain the health and lifestyle habits of students throughout medical school.
Subjects and Methods
The study used a prospective, longitudinal design to assess changes in a variety of health indicators in medical students between their first and last quarters of medical school. All participants gave written, informed consent, and the study was approved by the Institutional Review Boards of the institutions conducting the research. During Fall 2006 and Fall 2007, all male and nonpregnant female 1st-year medical students attending a local university were eligible to participate in the study. Participants were recruited through communications to all incoming students. Interested students were scheduled for a visit at a nearby research center. Because some study investigators have a teaching role at the university, students were assured that their decision whether to participate would not affect their grades.
In the first quarter of year 1 (academic years 2006, 2007) and the last quarter of year 4 (academic years 2010, 2011), participants’ clinical parameters were measured by trained clinical research staff. Height, weight, body mass index (BMI), and waist circumference were measured using standard methods described previously. [16] Percent body fat was measured by dual-energy X-ray absorptiometry (Discovery 4500A, Hologic Inc, Bedford, MA, USA). Blood pressure was measured manually twice, after a 5 minutes rest with participants seated; if systolic or diastolic values differed by more than 5 mmHg, a third measurement was taken. Fasting blood was obtained through venipuncture and analyzed in the Centers for Disease Control and Prevention (CDC)-certified laboratory for lipids, glucose, and insulin.
Participants completed the Baecke questionnaire of physical activity, [17] a brief, self-administered tool validated for use in adults to assess usual physical activity. [18] The Baecke questionnaire contains 16 questions divided into three categories: occupational physical activity, leisure-time sports participation, and nonsport leisure time physical activity. Cardiovascular fitness was measured using the Forestry step test, a modified version of the Harvard step test. [19] A fitness score based on the step test results and adjusted for age, weight, and gender was determined using tables developed by Sharkey. [20] Numeric scores were translated into seven fitness categories ranging from superior to very poor. [21]
At the study visit, a registered dietitian instructed each participant how to record their dietary intake. Participants were also given written instructions and a handout describing how to estimate portion sizes. Participants recorded all food, beverage, and supplement intake for 3 days. Completed records were reviewed by the dietitian, and the data were analyzed using Nutrition Data Systems for Research (Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN, USA). The 3 days of intake were averaged together to reflect the usual intake. The 3-day diet record is an appropriate method for assessing intake of energy and macronutrients in adults. [22] The analysis included intake of kilocalories, macronutrients, specific micronutrients, fiber, and alcohol as well as food groups. The Healthy Eating Index (HEI) 2005 is a composite of 12 components that represent both adequacy of diet and moderation of intake. The HEI score was calculated according to established methods, with a maximum score of 100. [23]
Each participant completed the CDC’s health-related quality of life (HR-QOL) survey. This 14-item tool is a validated [24] and reliable [25] instrument that assesses respondents’ perceptions of mental and physical health during the past 30 days. The HR-QOL measures self-reported perception of one’s overall health, physical health, and mental health (with response choices of excellent, very good, good, fair, or poor); physical or mental health symptoms; and number of perceived “healthy days” in the past 30 days.
Statistical methods
To ensure a power of at least 80% and margin of error of 5% at 95% confidence interval, nQuery Advisor®, version 5.0 (Statistical Solutions Ltd, Cork, Ireland) software was used to calculate the minimum sample size required. Data were entered in a password-protected database and analyzed in 2013–2014 using SAS®, version 9.3 (SAS Institute, Cary, NC, USA). The initial univariate analysis involved checking distributions, looking for outliers, and examining deviation from the assumption of normality. A natural logarithmic transformation was used for analysis of triglycerides, physical activity, total caloric intake, total alcohol intake, percent alcohol intake, and Vitamin D. Pearson’s correlations were used to assess the association between measured outcome at either baseline or follow-up, both overall and by gender. A generalized linear model was used to examine the change over time, initially examining the time by gender interaction. If the interaction was nonsignificant (P ≥ 0.05), the model including only the main effects was examined to look at both time and gender differences. Means or least-square means, as appropriate, and associated standard errors (SEs) are reported; for variables analyzed using a natural logarithmic transformation, the geometric means and associated geometric SE are reported. All means and SEs are reported as means (SE). The 95% confidence limits for the mean are also reported, as appropriate. P < 0.05 was considered statistically significant, unless otherwise noted.
Results
A total of 125 medical students (55 males and 70 females; 99 Caucasians, 4 African Americans, and 22 Asians) were enrolled in the study, reflecting 46.5 percent (67/144) of the 1st-year students in 2006 and 40.8 percent (58/142) of the 1st-year students in 2007. Seventy-eight percent (97/125) of the enrolled participants completed both visits. Reasons for attrition included leaving the class or the program (n = 8) and being lost to follow-up, referring to those who were still in the program but did not respond to multiple attempts to schedule a follow-up study visit, or those who scheduled but did not attend the follow-up visit in year 4 (n = 20). On comparing baseline characteristics of participants who completed the study and those who did not, the groups had similar demographic, anthropometric, and metabolic profiles, except plasma triglycerides which were higher among completers. Participant characteristics at baseline (year 1) are shown in Table 1. Males and females differed on four measures: BMI (25.5 [0.5] kg/m2 for males vs. 22.7 [0.4] kg/m2 for females), waist circumference (mean 87.5 [1.4] cm for males vs. 81.2 [1.2] cm for females), body fat (mean 18.1 [0.8] percent for males vs. 27.8 [0.7] percent for females), and high-density lipoprotein (HDL)-cholesterol (mean 48.0 [1.8] mg/dL for males vs. 59.4 [1.5] mg/dL for females) (P < 0.001 for all measures). The age and race composition of our study population was representative of the year 1 class at the UC College of Medicine; however, we had a slight over-representation of female students.
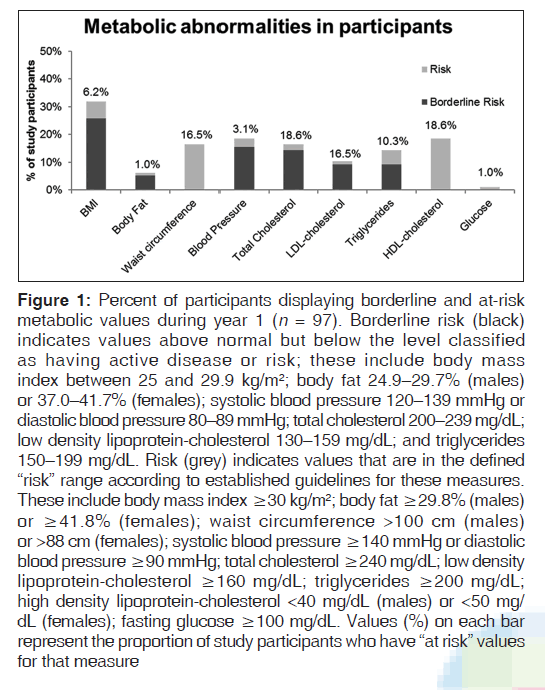
Although mean values for anthropometric and metabolic measures at year 1 were within or near the healthy range, [26-30] a number of students exhibited values indicating cardiometabolic risk [Figure 1]. Changes over the course of medical school are shown in Table 1. There were no statistically significant differences between year 1 and year 4 in body size or composition. Systolic blood pressure did not show a statistically significant change from year 1 to year 4, but diastolic blood pressure increased from 67.6 (0.8) to 70.7 (0.8) mmHg (P = 0.01). HDL-cholesterol increased from 53.6 (1.2) to 59.3 (1.2) mg/dL (P < 0.001) but total cholesterol, low-density lipoprotein (LDL)-cholesterol, and triglycerides did not show any statistically significant change over time. Fasting insulin increased from 11.3 (0.5) to 16.5 (0.5) μU/mL (P < 0.001), while fasting blood glucose did not show any statistically significant change. As would be expected, at each time point, BMI was negatively correlated with HDL-cholesterol and positively correlated with total cholesterol, LDL-cholesterol, triglycerides, blood pressure, waist circumference, glucose, and insulin. BMI and percent body fat were positively correlated by sex at both time points.
| Characteristics | Year 1 | Year 4 | P* |
|---|---|---|---|
| Age (years) | 23.9 (0.24) | 27.9 (0.24) | <0.001 |
| 23.4-24.4 | 27.4-28.4 | ||
| BMI (kg/m2) | 24.1 (0.33) | 24.1 (0.33) | 0.97 |
| 23.4-24.7 | 23.5-24.7 | ||
| Waist | 84.4 (0.92) | 84.6 (0.92) | 0.89 |
| circumference (cm) | 82.6-86.2 | 82.8-86.4 | |
| Body fat (%) | 23.0 (0.51) | 23.1 (0.50) | 0.83 |
| 22.0-24.0 | 22.1-24.1 | ||
| Total cholesterol (mg/dL) | 169.5 (3.75) | 169.3 (3.75) | 0.97 |
| 162.2-176.8 | 161.9-176.6 | ||
| HDL-cholesterol (mg/dL) | 53.6 (1.18) | 59.3 (1.18) | <0.001 |
| 51.3-55.9 | 57.0-61.6 | ||
| Triglycerides (mg/dL)† | 91.4 (1.05) | 81.9 (1.05) | 0.26 |
| 83.1-100.4 | 74.5-90.1 | ||
| LDL-cholesterol (mg/dL) | 93.7 (2.82) | 91.2 (2.81) | 0.52 |
| 88.2-99.3 | 85.7-96.7 | ||
| Fasting glucose (mg/dL) | 85.8 (1.25) | 89.0 (1.24) | 0.07 |
| 83.3-88.2 | 86.6-91.4 | ||
| Fasting insulin (μU/mL) | 11.3 (0.54) | 16.5 (0.54) | <0.001 |
| 10.2-12.4 | 15.5-17.6 | ||
| Systolic blood pressure | 107.4 (1.01) | 109.2 (1.01) | 0.22 |
| (mmHg) | 105.5-109.4 | 107.2-111.2 | |
| Diastolic blood pressure | 67.6 (0.83) | 70.7 (0.83) | 0.01 |
| (mmHg) | 66.0-69.3 | 69.1-72.3 |
Data are reported as mean (SE) 95% confidence limit for the mean. *P value for change in value from year 1 to year 4, note these means are adjusted for sex, †For triglycerides, geometric means and standard errors with appropriate 95% CI are reported. BMI: Body mass index, HDL: High-density lipoprotein, LDL: Low-density lipoprotein, CI: Confidence interval, SE: Standard error
Table 1: Anthropometric and metabolic measures of participants in year 1 and year 4 of medical school (n=97)
Figure 1: Percent of participants displaying borderline and at-risk metabolic values during year 1 (n = 97). Borderline risk (black) indicates values above normal but below the level classified as having active disease or risk; these include body mass index between 25 and 29.9 kg/m2; body fat 24.9–29.7% (males) or 37.0–41.7% (females); systolic blood pressure 120–139 mmHg or diastolic blood pressure 80–89 mmHg; total cholesterol 200–239 mg/dL; low density lipoprotein-cholesterol 130–159 mg/dL; and triglycerides 150–199 mg/dL. Risk (grey) indicates values that are in the defined “risk” range according to established guidelines for these measures. These include body mass index ≥30 kg/m2; body fat ≥29.8% (males) or ≥41.8% (females); waist circumference >100 cm (males) or >88 cm (females); systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg; total cholesterol ≥240 mg/dL; low density lipoprotein-cholesterol ≥160 mg/dL; triglycerides ≥200 mg/dL; high density lipoprotein-cholesterol <40 mg/dL (males) or <50 mg/ dL (females); fasting glucose ≥100 mg/dL. Values (%) on each bar represent the proportion of study participants who have “at risk” values for that measure
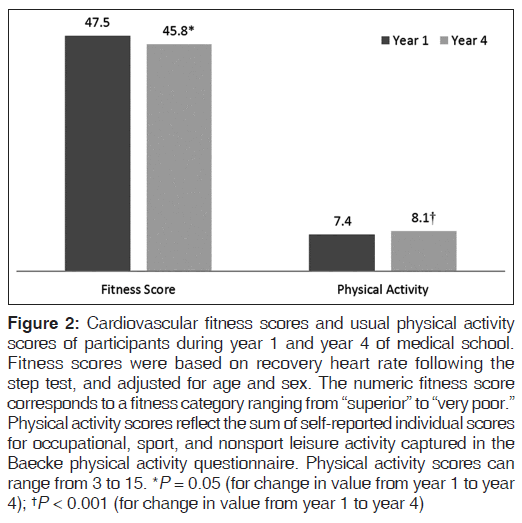
Cardiovascular fitness scores showed a trend toward declining over time (from 47.5 [0.6] to 45.8 [0.6]; P = 0.05); yet, mean scores in both year 1 and year 4 fell within the “Very Good” fitness category for both genders. Conversely, self-reported physical activity increased from year 1 to year 4 (P < 0.001), with a mean score consistent with those reported by similar age groups in other studies [Figure 2]. [31,32]
Figure 2: Cardiovascular fitness scores and usual physical activity scores of participants during year 1 and year 4 of medical school. Fitness scores were based on recovery heart rate following the step test, and adjusted for age and sex. The numeric fitness score corresponds to a fitness category ranging from “superior” to “very poor.” Physical activity scores reflect the sum of self-reported individual scores for occupational, sport, and nonsport leisure activity captured in the Baecke physical activity questionnaire. Physical activity scores can range from 3 to 15. *P = 0.05 (for change in value from year 1 to year 4); †P < 0.001 (for change in value from year 1 to year 4)
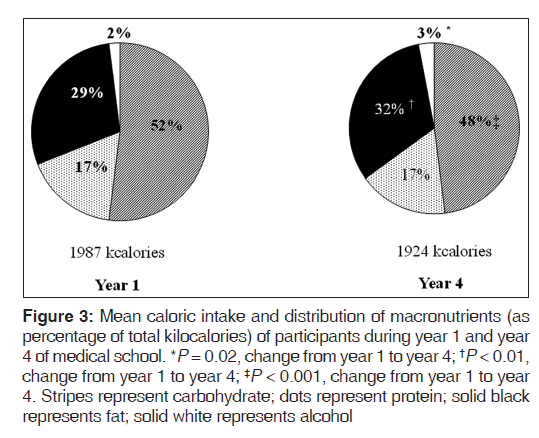
Participants’ energy intake remained constant from year 1 to year 4; however, the macronutrient distribution of energy changed, with the percentage of energy from fat increasing from 29.1 (0.7) to 32.0 (0.7) (P < 0.01), and percentage of energy from carbohydrate decreasing from 52.3 (0.9) to 47.9 (0.9) (P < 0.001) [Figure 3]. Intake of alcohol as a percentage of total energy increased (P = 0.02) from year 1 to year 4 [Figure 3], but the mean intake of alcohol was low. With the exception of Vitamin D and sodium, participants’ mean intake of all micronutrients analyzed met the dietary reference intakes (DRIs) [33] and did not change significantly from year 1 to year 4. The mean HEI score measured in year 1 of 65.6 (1.2) was higher than in the general population of 20–39 year olds (54.2), [34] with no statistically significant change when remeasured in year 4.
Figure 3: Mean caloric intake and distribution of macronutrients (as percentage of total kilocalories) of participants during year 1 and year 4 of medical school. *P = 0.02, change from year 1 to year 4; †P < 0.01, change from year 1 to year 4; ‡P < 0.001, change from year 1 to year 4. Stripes represent carbohydrate; dots represent protein; solid black represents fat; solid white represents alcohol
Significant gender differences were seen for three nutrients. The overall mean intake in Vitamin D increased over time from 192 (43.6) to 272 (43.6) IU/day (P < 0.01) from year 1 to year 4, with an increase from 164 (44.4) to 308 (44.4) IU/day (P < 0.001) among females but no statistically significant change among males. Dietary sodium decreased from 3899 (124.5) to 3528 (124.5) mg/day among all participants (P = 0.04), with intake significantly declining from 4770 (188.3) to 3742 (188.3) mg/day (P < 0.001) among males but no significant change among females. Trans fat intake increased among males from 2.4 (0.2) to 3.4 (0.2) g/day (P < 0.01) over the study period, but did not change significantly among females.
According to the HR-QOL, all participants rated their health as good, very good, or excellent. When asked about their health in the past 30 days, in year 1, the median number of poor physical health days reported by both genders was 0, and the median number of poor mental health days was 3. These HR-QOL measures showed no statistically significant changes from year 1 to year 4.
Discussion
Our results indicate that medical students in this study were generally healthy with relatively few participants exhibiting values associated with clinical risk. Although obesity rates in the US have increased significantly over the past three decades, based on BMI measures only 6.2% (6/97) of participants at the year 1 visit, and 5.1% (5/97) at the year 4 visit were obese. These figures are considerably lower than the 30.3% prevalence rate among young adults in the US. The prevalence rates of overweight among the participants (25.8% [25/97] in year 1 and 27.8% [27/97] in year 4) were slightly below the national rate of 30% among young adults. [35] Participants’ body fat measures were significantly correlated with BMI, by sex. However, body fat measures indicated a slightly lower prevalence of overweight and obesity [29] than BMI measures. As expected, BMI and % body fat were significantly correlated with almost all clinical measures; that is, students with higher BMIs and higher % body fat were more likely to exhibit higher cardiometabolic risk.
Diastolic blood pressure and insulin worsened among participants from year 1 to year 4. Hypertension is diagnosed when systolic blood pressure is ≥140 mmHg, or diastolic blood pressure is ≥90 mmHg. While hypertension is prevalent among 7.3% of Americans aged 18–39 years, [36] there were no participants with blood pressure levels indicating hypertension. Still, 18.5% (18/97) of the study population in year 4 exhibited prehypertension, which is having systolic blood pressure between 120 and 139 mmHg or diastolic blood pressure between 80 and 89 mmHg. Elevated fasting insulin indicates insulin resistance, a risk factor for diabetes and cardiovascular disease. Although insulin levels increased significantly during the study period, mean fasting insulin values in both year 1 and year 4 were within the reference range. [28] However, in year 4, 10 participants had insulin levels exceeding 25 μU/mL. Mean levels of HDL-cholesterol among participants were higher than the adult average [37] and increased over the course of medical school. Lifestyle modification associated with increased HDL-cholesterol includes frequent aerobic activities. Interestingly, participants reported an increase in their physical activity during medical school, which may have been influenced by the opening of a fitness center within the medical college mid-way through the study period.
In our study, participants reported lifestyle habits congruent with national recommendations. Prior research has indicated that medical students report higher physical activity levels than age-matched peers in the general population. [9] However, a recent longitudinal study using objective measures of physical fitness among medical students at the Uniformed Services University showed that muscular endurance and aerobic capacity declined during medical school. [38] Our results concurred with these studies, showing a trend toward declining physical fitness during medical school, despite a reported increase in physical activity.
While college students often adopt unhealthy eating habits related to factors such as stress and lack of time, a recent study of Malaysian medical students by Ganasegeran et al. [39] suggested that most medical students consume relatively healthy diets that meet national dietary guidelines. Similarly, our findings showed that participants’ intake of carbohydrate, protein, and fat was within the acceptable macronutrient distribution ranges, intake of most micronutrients met DRI recommendations, and HEI scores were indicative of a relatively high-quality diet in both years 1 and 4.
Despite the overall quality of the participants’ diets, a few concerns were noted. With the increasing awareness of the essential role of Vitamin D in preventing osteoporosis and the common occurrence of insufficient Vitamin D status in the US, it is not surprising that Vitamin D intake increased during the study, particularly among females. Yet, the mean Vitamin D intake was below the current recommendation of 600 IU/day for both males and females throughout medical school. Similarly, some students may have been motivated to restrict sodium intake due to an emphasis on lowering dietary sodium for the prevention and treatment of hypertension. However, the average sodium intake of all participants remained higher than the American Heart Association recommendation of 1500-2300 mg/day. The role of trans fat in the promotion of cardiovascular disease led the National Heart, Lung, and Blood Institute and the American Heart Association to recommend consuming as little trans fat as possible. Yet, intake of trans fat, found primarily in convenience and processed foods, increased among males during the study period.
In a longitudinal survey of US medical students by Frank et al., [10] almost all students (97%) categorized their health as good, very good, or excellent, with a median of 1 day of poor physical health in the past month. Women reported significantly more days of poor mental health at the end of medical school (i.e. an increase from 1 to 2 days per month), while men reported no days of poor mental health at the start and finish of medical school. Our study results support the prior study’s notion that medical students rate their health highly with very little occurrence of poor physical health. However, in our study, both males and females reported a higher frequency of poor mental health (median of 3 days per month) throughout medical school, perhaps related to multiple stressors such as academic challenges, financial concerns, or life events. [11,12]
The results of several research studies suggest that the integration of nutrition and physical activity topics throughout the curriculum’s didactic and clinical components is needed to positively influence students’ knowledge and behaviors. [4,40,41] During the study, in years 1 and 2 of medical school, the College’s Clinical Foundations courses included nutrition lectures that were delivered by physicians and dietitians. The lecturers addressed dietary guidelines for disease prevention and nutrition therapy for several medical conditions, such as cardiovascular disease, diabetes, obesity, and critical illness. During the 3rd year clerkships, teaching strategies included lectures, case studies, online learning modules, and clinical experiences that addressed clinical nutrition. In addition, optional nutrition-related learning experiences were available to students. Clinical Nutrition, a 2-week elective course, was offered to 4th year students. The Medical Student Scholars Program – Nutrition Pathway was a longitudinal program that offered nutrition-related extracurricular educational, clinical and research experiences to selected members who were admitted as 1st year students.
Limitations
There are inherent limitations to our study. Since all participants were recruited from one medical school, generalizability of results is limited to similar institutions. Enrollment in the study was voluntary and limited; therefore, study participants may not represent our medical student population in terms of health status or lifestyle habits. While we assessed alcohol consumption as part of the overall diet analysis, we did not collect further data on factors such as alcohol consumption patterns, smoking, or other coping behaviors which may have provided more insight into the participants’ health. The longitudinal design and objective measurement of clinical parameters by trained health professionals following specific protocols are strengths of the study. Controversy remains over whether medical school does or does not affect the health status of students. Therefore, future longitudinal studies using similar clinical measures are needed with larger samples of medical students from several universities.
Conclusions
To the best of our knowledge, this is the first longitudinal study that assessed anthropometric and metabolic measures and lifestyle behaviors of medical students. Overall, our findings suggest that students’ health and habits do not decline over the course of medical school; yet some students exhibit at-risk clinical measures, as well as diet and activity behaviors that are not aligned with national recommendations.
Prior research has shown that the health practices of medical students and physicians have the potential to play a highly influential role in counseling patients about disease prevention. Those who engage in healthy lifestyles are more likely to serve as role models and to provide quality counseling on exercise, diet, smoking, and other practices. [4,42] Integration of the behavioral and social components of health (e.g., diet and physical activity) throughout medical school curricula has been recommended for over a decade by the Institute of Medicine [43] and others. [7,8] At the time of the study, the College of Medicine’s inclusion of nutrition-related lectures, case studies, online modules, and clinical experiences throughout the curriculum and the addition of a fitness center are noteworthy. Such curricular initiatives that address essential lifestyle practices may be the first step in enhancing students’ self-awareness, self-efficacy, and motivation to model healthy behaviors for their patients. [40,42] Moreover, integration of behavioral counseling into the curriculum’s didactic and experiential components may advance students’ skills to engage in preventive counseling. Ultimately, such educational efforts may lead to healthier lifestyle habits and positive health outcomes for future physicians and their patients.
Acknowledgments
Amy Shova and Nicole Wrassmann, research assistants, provided valuable assistance with study coordination and data entry. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Financial support and sponsorship
The project was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health, under Award Number UL1TR000077. Approval for the study was granted by the Institutional Review Boards of the University of Cincinnati (IRB 06-07-12-01) and Cincinnati Children’s Hospital Medical Center (IRB 2008-1235).
Conflicts of interest
The salaries of Ms. Summer, Dr. Khoury, and Dr. Heubi are funded either entirely or in part by the National Center for Advancing Translational Sciences of the National Institutes of Health, under Award Number UL1TR000077, the grant which supported this study. Dr. Brehm, Dr. Filak, and Dr. Lieberman have no conflicts of interest related to this study.
References
- Institute of Medicine. For the Public’s Health: Investing in a Healthier Future. Washington, DC: The National Academies Press; 2012.
- Frank E, Segura C, Shen H, Oberg E. Predictors of Canadian physicians’ prevention counseling practices. Can J Public Health 2010;101:390-5.
- Howe M, Leidel A, Krishnan SM, Weber A, Rubenfire M, Jackson EA. Patient-related diet and exercise counseling: Do providers’ own lifestyle habits matter? Prev Cardiol 2010;13:180-5.
- Lobelo F, Duperly J, Frank E. Physical activity habits of doctors and medical students influence their counselling practices. Br J Sports Med 2009;43:89-92.
- Eisenberg DM, Burgess JD. Nutrition education in an era of global obesity and diabetes: Thinking outside the box. Acad Med 2015;90:854-60.
- Phillips E, Pojednic R, Polak R, Bush J, Trilk J. Including lifestyle medicine in undergraduate medical curricula. Med Educ Online 2015;20:26150.
- Kushner RF, Van Horn L, Rock CL, Edwards MS, Bales CW, Kohlmeier M, et al. Nutrition education in medical school: a time of opportunity. Am J Clin Nutr 2014;99 5 Suppl: 1167S-73S.
- Torabi MR, Tao R, Jay SJ, Olcott C. A cross-sectional survey on the inclusion of tobacco prevention/cessation, nutrition/diet, and exercise physiology/fitness education in medical school curricula. J Natl Med Assoc 2011;103:400-6.
- Frank E, Tong E, Lobelo F, Carrera J, Duperly J. Physical activity levels and counseling practices of U.S. medical students. Med Sci Sports Exerc 2008;40:413-21.
- Frank E, Carrera JS, Elon L, Hertzberg VS. Basic demographics, health practices, and health status of U.S. medical students. Am J Prev Med 2006;31:499-505.
- MacLean L, Booza J, Balon R. The impact of medical school on student mental health. Acad Psychiatry 2016;40:89-91.
- Lins L, Carvalho FM, Menezes MS, Porto-Silva L, Damasceno H. Health-related quality of life of students from a private medical school in Brazil. Int J Med Educ 2015;6:149-54.
- Majra J. Do our medical colleges inculcate health-promoting lifestyle among medical students: A pilot study from two medical colleges from Southern India. Int J Prev Med 2013;4:425-9.
- Kjeldstadli K, Tyssen R, Finset A, Hem E, Gude T, Gronvold NT, et al. Life satisfaction and resilience in medical school – A six-year longitudinal, nationwide and comparative study. BMC Med Educ 2006;6:48.
- Frank E, Carrera JS, Elon L, Hertzberg VS. Predictors of US medical students’ prevention counseling practices. Prev Med 2007;44:76-81.
- Brehm BJ, Lattin BL, Summer SS, Boback JA, Gilchrist GM, Jandacek RJ, et al. One-year comparison of a high-monounsaturated fat diet with a high-carbohydrate diet in type 2 diabetes. Diabetes Care 2009;32:215-20.
- Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr 1982;36:936-42.
- Pols MA, Peeters PH, Bueno-De-Mesquita HB, Ocké MC, Wentink CA, Kemper HC, et al. Validity and repeatability of a modified Baecke questionnaire on physical activity. Int J Epidemiol 1995;24:381-8.
- Ryhming I. A modified Harvard step test for the evaluation of physical fitness. Arbeitsphysiologie 1953;15:235-50.
- Sharkey BJ. Physiology of Fitness. Champaign, IL: HumanKinetics; 1984.
- DeVries HA. Laboratory Experiments in Exercise Physiology. Dubuque, Iowa: Wm. C. Brown; 1971.
- Willett W. Nutritional Epidemiology. 3rd ed. Oxford: Oxford University Press; 2013.
- Landy DC, Kurtz JM, Miller TL, Ludwig DA. Statistical program to automate the creation of Healthy Eating Index scores using Nutrition Data System for Research output. J Acad Nutr Diet 2012;112:A14.
- Newschaffer C. Validation of Behavioral Risk Factor Surveillance System (BRFSS) HRQOL Measures in a Statewide Sample. Atlanta, Georgia: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1998.
- Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. J Epidemiol Community Health 2003;57:339-43.
- Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, et al. Executive Summary: Guidelines (2013) for the management of overweight and obesity in adults. Obesity 2014 Jul; 22 Suppl 2:S5-39.
- James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507-20.
- Melmed S, Polonsky KS, Larsen PR, Kronenberg HM. Williams Textbook of Endocrinology. Vol. 12. Philadelphia: Elsevier Saunders; 2011.
- Heo M, Faith MS, Pietrobelli A, Heymsfield SB. Percentage of body fat cutoffs by sex, age, and race-ethnicity in the US adult population from NHANES 1999-2004. Am J Clin Nutr 2012;95:594-602.
- Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol 2014;63:2889-934.
- Mustelin L, Joutsi J, Latvala A, Pietiläinen KH, Rissanen A, Kaprio J. Genetic influences on physical activity in young adults: A twin study. Med Sci Sports Exerc 2012;44:1293-301.
- Camhi SM, Katzmarzyk PT. Total and femoral neck bone mineral density and physical activity in a sample of men and women. Appl Physiol Nutr Metab 2012;37:947-54.
- National Institutes of Health, Office of Dietary Supplements. Nutrient Recommendations: Dietary Reference Intakes. Available from: https://www.ods.od.nih.gov/Health_ Information/Dietary_Reference_Intakes.aspx. [Last accessed on 2016 May 01].
- Ervin RB. Healthy Eating Index-2005 Total and Component Scores for Adults Aged 20 and Over: National Health and Nutrition Examination Survey, 2003-2004. National Health Statistics Reports. Vol. 44; 2011. p. 1-9.
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806-14.
- Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011-2012. NCHS Data Brief 2013;133:1-8.
- Carroll MD, Kit BK, Lacher DA, Shero ST, Mussolino ME. Trends in lipids and lipoproteins in US adults, 1988-2010. JAMA 2012;308:1545-54.
- Stephens MB, Cochran C, Hall JM, Olsen C. Physical fitness during medical school: A 4-year study at the Uniformed Services University. Fam Med 2012;44:694-7.
- Ganasegeran K, Al-Dubai SA, Qureshi AM, Al-abed AA, Am R, Aljunid SM. Social and psychological factors affecting eating habits among university students in a Malaysian medical school: A cross-sectional study. Nutr J 2012;11:48.
- Dacey ML, Kennedy MA, Polak R, Phillips EM. Physical activity counseling in medical school education: A systematic review. Med Educ Online 2014;19:24325.
- Kris-Etherton PM, Akabas SR, Bales CW, Bistrian B, Braun L, Edwards MS, et al. The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation and effectiveness. Am J Clin Nutr 2014;99 5 Suppl: 1153S-66S.
- Frank E, Elon L, Hertzberg V. A Quantitative assessment of a 4-year intervention that improved patient counseling through improving medical student health. MedGenMed 2007;9:58.
- Institute of Medicine. Improving Medical Education: Enhancing the Behavioral and Social Science Content of Medical School Curricula. Washington, DC: The National Academies Press; 2004.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.