Hemophagocytosis on Bone Marrow Aspirate Cytology: Single Center Experience in North Himalayan Region of India
- *Corresponding Author:
- Dr. Harish Chandra
Department of Pathology, Himalayan Institute of Medical Sciences, Swami Ram Nagar, Doiwala, Dehradun - 248 140, Uttarakhand, India.
E-mail: drharishbudakoti31@yahoo. co.in
Abstract
Background: The differentiation of hemophagocytic lymphohistiocytosis (HLH) with other causes of hemophagocytosis is essential as HLH is life‑threatening condition and requires definite clinical and biochemical criteria for its diagnosis. Aim: The present study was conducted to study hemophagocytosis on bone marrow aspirates and to observe if there is any difference on bone marrow examination between HLH and non HLH cases showing hemophagocytosis. Materials and Methods: The study reviewed all the cases of bone marrow aspirate for evidence of hemophagocytosis in which at least three smears and 500 nucleated cells were observed for every case. The cases were provisionally diagnosed as HLH according to the proposed HLH diagnostic criteria, 2009. Results: A total of 80 cases showed hemophagocytosis in the present study with infections followed by HLH being the most common cause. Pancytopenia and erythroid hyperplasis were common hematological presentation. Moderate to severe hemophagocytosis was observed in HLH cases while mild grade in non HLH cases. Conclusion: The study concludes that hemophagocytosis even if observed in single cell should always be documented in the bone marrow reports. It may be the only indicator of subtle infection in the marrow. Pancytopenia and higher grade of hemophagocytosis on bone marrow examination may be helpful in establishing an early differentiation of HLH and non HLH cases.
Keywords
Bone marrow, Hemophagocytic lymphohistiocytosis, Hemophagocytosis, Infection
Introduction
Hemophagocytosis is although a common phenomenon observed in bone marrow but at times it is overlooked and even if it is observed then it is not documented in the reports. Hemophagocytosis is the phagocytosis of erythrocytes, lymphocytes or other hematopoietic precursors by histiocytes or macrophages either in bone marrow, lymph node, liver or spleen. Phagocytosis basically involves attachment and binding of Fc and C3b to receptors on leukocyte membrane, engulfment and fusion of lysosomes with phagocytic vacuoles followed by digestion. [1] The increased histiocyticactivity may be observed in infections, inflammation, bone marrow hyperplasia or ineffective hematopoiesis. [2] Malignancies including leukemia, small cell lung carcinoma and rhabdomyosarcoma etc., have been reported to be associated with hemophagocytosis. [3-5] Hemophagocytic lymphohistiocytosis (HLH) is another important cause for increased hemophagocytosis resulting from prolonged and excessive accumulation of macrophages, histiocytes and CD8+ T-cells. [6] However, its diagnosis involves the consideration of other clinical and biochemical criteria apart from hemophagocytosis as proposed by the histiocyte society. [7] The differentiation of HLH from other causes of hemophagocytosis lies in the fact that HLH is life threatening condition which requires immediate appropriate treatment. [8] The present study was therefore conducted to study the hemophagocytosis on bone marrow aspirates, its causes, clinical correlation and associated features on bone marrow examination and to observe if there is any difference on bone marrow examination between HLH and non HLH cases showing hemophagocytosis.
Materials and Methods
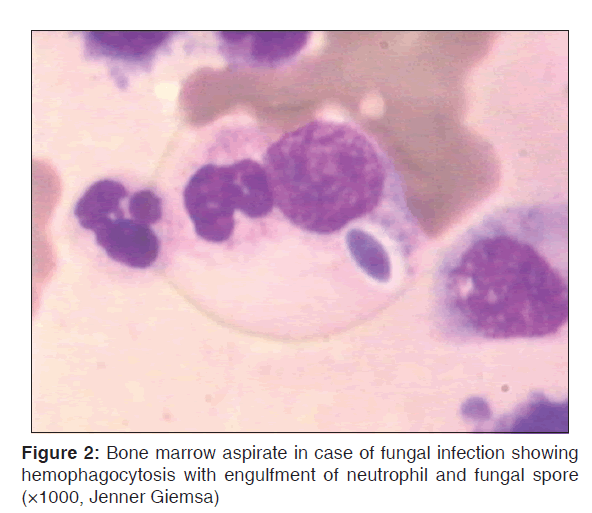
The study was conducted in the Pathology Department of the institute which included review of all the bone marrow aspirate cytology smears for evidence of hemophagocytosis from January 2006 to December 2010. At least three smears and 500 nucleated cells were observed for hemophagocytosis for every case. Hemophagocytosis was graded on bone marrow aspirate by using the criteria as: (0) Absent; (1) mild <2 histiocytes with hemophagocytosis/slide; (2) moderate-2-5 histiocytes with hemophagocytosis/slide; (3) severe >5 histiocytes with hemophagocytosis/slide. [9] The smears showing even a single cell with hemophagocytosis were considered positive. Clinical details and relevant investigations were noted for every case. The cases were provisionally diagnosed as HLH according to the proposed HLH diagnostic criteria, 2009. [6] The diagnosis of leukemia, lymphoma and multiple myeloma were confirmed on bone marrow examination. Cytochemistry, immunophenotyping and serum protein electrophoresis were performed where-ever possible for definite diagnosis and typing. Hypocellular marrow/aplastic anemia were confirmed on bone marrow trephine biopsy. Metastasis was confirmed on bone marrow examination (aspirate, imprint and biopsy) by demonstration of metastatic cells from solid tumors in bone marrow. The diagnosis of fungal infection and leishmaniasis were made by direct demonstration of fungal spores/hyphae and LD bodies on bone marrow. Viral infections were confirmed by relevant serology. The diagnosis of tuberculosis was made by demonstration of acid fast bacilli on Ziehl Neelsen staining or necrosis and granuloma on bone marrow. All the tubercular cases were known cases of primary tuberculosis. The study was approved by the research committee of the institute.
Results
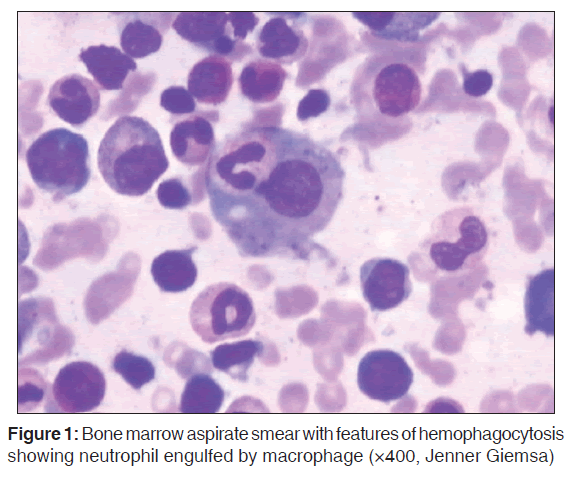
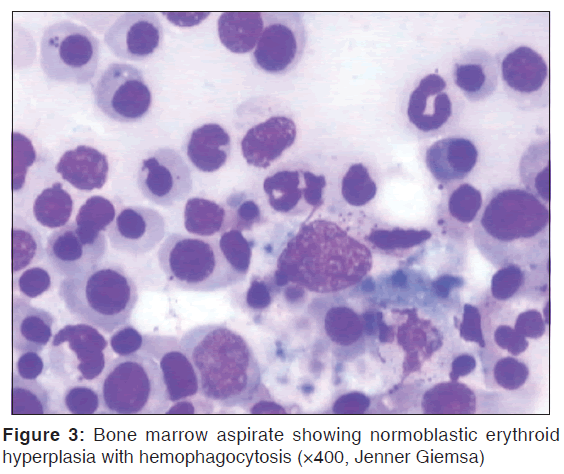
A total of 80 cases showed hemophagocytosis on bone marrow aspirate cytology in the present study. Table 1 shows the different cases which showed hemophagocytosis on bone marrow aspirate cytology. Infections and HLH was the most common cause associated with hemophagocytosis [Figures 1 and 2]. Nearly 8.7% 7/80 out of total cases showing hemophagocytosis showed evidence of leishmaniasis with HLH. The grading of hemophagocytosis was 1+ (mild) in 47 cases and all these cases were non HLH cases. 2+ (moderate) grade was observed in 17 cases and out of it 4 were HLH cases. 3+ (severe) grade was observed in 16 cases and all were HLH cases. Table 2 shows the clinical features observed in cases showing hemophagocytosis. Fever, hepatomegaly and splenomegaly were commonly observed clinical features. Table 3 shows the related hematological findings observed in peripheral blood and bone marrow in cases showing hemophagocytosis. Pancytopenia was commonly observed in peripheral blood while normoblastic erythroid hyperplasia was the common findings observed in bone marrow [Figure 3]. Table 4 shows the parameters of HLH according to proposed HLH diagnostic criteria, 2009. [6] X-linked lymphoproliferative syndrome and molecular diagnosis of HLH was not possible in any case. Table 5 shows comparison of parameters between HLH and non HLH cases showing hemophagocytosis. It shows that hemophagocytosis was mild (1+) in non HLH cases while it was of moderate to severe grade (2+ to 3+) in HLH cases and 73.3% HLH cases showed pancytopenia in comparison to 33.3% cases in non HLH cases.
| Diagnosis | Number of cases | Percentage of total cases |
|---|---|---|
| Infections | 10 | 12.5 |
| Viral | 3 | - |
| Tuberculosis | 3 | - |
| Fungal | 2 | - |
| Malarial | 2 | - |
| HLH | 10 | 12.5 |
| Leukemia | 7 | 8.7 |
| NHL | 8 | 10 |
| Hodgkin’s disease | 2 | 2.5 |
| Nutritional anemia | 9 | 11.2 |
| Anemia of chronic disorder | 4 | 5 |
| Metastasis | 3 | 3.7 |
| Idiopathic thrombocytopenia purpura | 4 | 5 |
| Leishmaniasis with HLH | 7 | 8.7 |
| Leukemia with HLH | 2 | 2.5 |
| NHL with HLH | 1 | 1.2 |
| Multiple myeloma | 3 | 3.7 |
| Hypocellular/aplastic anemia | 3 | 3.7 |
| Miscellaneous | 7 | 8.7 |
| Total | 80 | 100 |
HLH: Hemophagocytic lymphohistiocytosis, NHL: Non-Hodgkin’s lymphoma
Table 1: Cases showing hemophagocytosis on bone marrow aspirate cytology
| Clinical features | Number of cases | Percentage of total cases |
|---|---|---|
| Fever | 25 | 31.2 |
| Hepatomegaly | 24 | 30 |
| Splenomegaly | 20 | 25 |
| Symptoms related to anemia | 20 | 25 |
| (weakness, loss of appetite, lassitude) | ||
| Lymphadenopathy | 11 | 13.7 |
| Generalized pain | 8 | 10 |
| Hemorrhage or bleeding gums | 3 | 3.7 |
| Others (gastritis, nausea etc.) | 3 | 3.7 |
Table 2: Clinical features of cases showing hemophagocytosis
| Characteristics | Number of cases | Percentageof total cases |
|---|---|---|
| Pancytopenia | 15 | 18.7 |
| Normoblastic erythroid hyperplasia | 15 | 18.7 |
| Normal marrow | 7 | 8.7 |
| Dysplasia in marrow | 7 | 8.7 |
| Hypocellular marrow | 5 | 6.2 |
| Plasmacytosis | 3 | 3.7 |
| Eosinophillia in marrow | 3 | 3.7 |
| Perl’s iron stain in marrow | ||
| Reduced or nil | 39 | 48.7 |
| Increased | 15 | 18.7 |
| Normal | 10 | 12.5 |
Table 3: Related hematological characteristics observed in peripheral blood and bone marrow in cases showing hemophagocytosis
| Parameter | No. of cases | Percentage of total HLH cases |
|---|---|---|
| Molecular diagnosis of HLH or X-LP (or) | None | 0 |
| At least 3 of 4 | ||
| Fever | 9 | 45 |
| Splenomegaly | 6 | 30 |
| Cytopenias | 11 | 55 |
| Hepatitis (and) | 3 | 15 |
| At least 1 of 4 | ||
| Hemophagocytosis | 20 | 100 |
| Ferritin (≥500 µg/L) | 8 | 40 |
| ↑ soluble IL-2 receptor | None | 0 |
| Absent or ↓ NK cell function | None | 0 |
| Other results supportive of HLH diagnosis | ||
| Fasting triglycerides (≥265 mg/dL) | 9 | 45 |
| Hypofibrinogenemia (≤1.5 g/L) | 6 | 30 |
| Hyponatremia | 2 | 10 |
HLH: Hemophagocytic lymphohistiocytosis, X-LP: X-linked lymphoproliferative
Table 4: Parameters of HLH cases according to proposed HLH diagnostic criteria, 2009[6]
| Parameters | HLH cases | Non-HLH cases |
|---|---|---|
| Age (mean in years) | 42.3 | 37.0 |
| Sex (male: female ratio) | 1.75:1 | 1.50:1 |
| Fever (no. of cases) | 9 | 16 |
| Hepatosplenomegaly (no. of cases) | 12 | 23 |
| Average grading of bone marrow | 2+to 3+ | 1+ (mild) |
| hemophagocytosis | (moderate | |
| to severe) | ||
| Pancytopenia (% of cases) | 73.3 | 26.6 |
| Serum ferritin (mean) µgm/L | 605 | 115 |
| Serum triglycerides (mean) mg/dL | 315 | 100 |
| Fibrinogen level (mean) g/L | 1 | 2.1 |
| Na+level (mean) meq/L | 115 | 139 |
| Outcome of patients | ||
| Responded to treatment | 85% (17) | 98.3% (59) |
| Succumbed to illness | 10% (2) | 0 |
| Loss of follow-up | 5% (1) | 1.7% (1) |
HLH: Hemophagocytic lymphohistiocytosis
Table 5: Comparison of parameters between HLH and non-HLH cases showing hemophagocytosis
Discussion
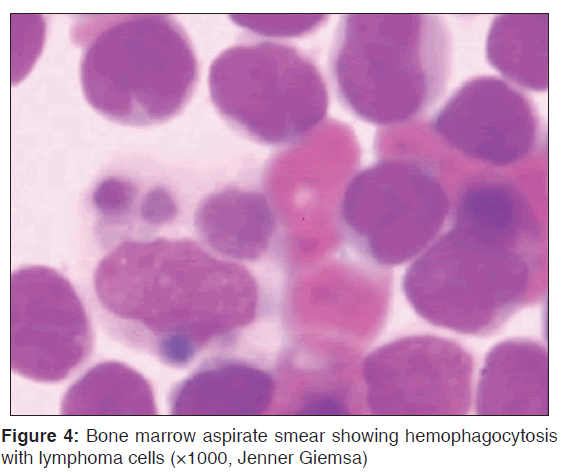
Hemophagocytosis is although an interesting finding that is observed in the bone marrow but at times it is overlooked or is not documented in the reports. However, the presence of hemophagocytosis may be associated with variety of conditions including infections, neoplasm or specific therapy. [2,3,10] The present study observed that hemophagocytosis was commonly associated with infections including viral, tubercular, fungal and malarial infections. It was also observed in the study that in certain cases of fungal infection and leishmaniasis, hemophagocytosis was the only finding seen initially that indicated an infection in the marrow. Thus, it is suggested that at times hemophagocytosis may be the only indicator of infection and vigilant examination of such marrow is essential to identify the causative organism in the marrow. HLH was another common condition associated with hemophagocytosis in the study. It is highly stimulated but ineffective immune response that may be familial or acquired and is life-threatening condition. [8] The hypersecretion of pro-inflammatory cytokines such as interferon γ, tumor necrosis factor α along with CD8 T-cells are crucial in the pathogenesis of HLH. [8,11] It is essential to distinguish whether the hemophagocytosis present in the marrow is only an isolated finding or is associated with HLH syndrome. HLH requires other clinical, biochemical and genetic criteria for diagnosis which have been proposed to be modestly modified in 2009. [6,7] The differentiation of hemophagocytosis triggered due to infection or any other cause with hemophagocytosis due to HLH is important as HLH is life-threatening condition and only the pathogen directed therapy is usually not sufficient to control severe hyper-inflammation in HLH. [8] The treatment of HLH requires combination of proapoptotic chemotherapy, immunosuppressive drugs or definitive treatment by hematopoietic cell transplantation HLH. [6] It should be started in clinically suspected cases even when results of few diagnostic criteria are pending. [6] This itself lays the importance of documenting the presence of hemophagocytosis in every case on bone marrow examination reports. Another interesting feature that was observed in the study was that all the cases of leishmaniasis were associated with HLH. Case reports have been rarely documented in the literature of association of visceral leishmaniasis with HLH. [12] This increased association of leishmaniasis with HLH in the study may be due to the reason that authors considered more modest criterions for diagnosis of HLH as proposed by Histiocyte Society 2009. [6] It was also observed that five out of these seven cases responded well to amphotericin further suggesting that leishmaniasis with HLH can respond well to amphotericin. HLH has also been reported to be associated with acute myeloid leukemia, aplastic anemia and tuberculosis. [13-15] The present study also showed the association of HLH with leukemia and Non-Hodgkin’s lymphoma [Figure 4]. Pancytopenia was the most common hematological finding observed in the study while hepatosplenomegaly and fever common clinical findings. Clinical features and presence of cytopenia are important diagnostic criteria for HLH and can be helpful in discriminating hemophagocytosis due to infection and other causes from hemophagocytosis due to HLH. Another point to be highlighted in the study is that greater number of cases with HLH (73.3%) 11/15 cases showed pancytopenia in comparison to 26.6% (4/15) of non HLH cases out of total cases with pancytopenia. Associated bone marrow findings observed in the study including dysplasia, normoblastic erythroid hyperplasia or hypocellular marrow which may be due to the primary disease. An important finding that was observed in the study was that hemophagocytosis was of moderate to severe grade (2+ to 3+) in HLH cases showing hemophagocytosis on bone marrow examination and may prompt for other investigations to confirm HLH. Gupta et al. have observed in their study that 58% of patients with HLH had at least one hemophagocytosis per 500 nucleated cells and concluded that the number of hemophagocytosis at initial bone marrow aspirate is low and variable and should be reported. [16]
Conclusion
The study concludes that hemophagocytosis which is an interesting but commonly overlooked finding observed in bone marrow should always be documented in the reports. It may be the only clue leading to vigilant search of infection in the marrow. It is also essential to distinguish hemophagocytosis due to HLH or hemophagocytosis due to other causes as HLH is life-threatening condition. This distinction requires appropriate clinical features and relevant investigations for every case showing hemophagocytosis. Pancytopenia and grade of hemophagocytosis may be helpful in this regard. Higher grade of hemophagocytosis (2+ to 3+) in cases with HLH may help in establishing an early differentiation of HLH from non HLH cases. Further studies involving quantification of cells showing hemophagocytosis and its relation to severity of the disease may also be carried out.
References
- Kumar V, Abbas AK, Fausto N, editors. Acute and chronic inflammation. In: Robbins and Cotran Pathologic Basis of Disease. 7th ed. Pennsylvania: Saunders; 2006. p. 59-61.
- Bain BJ, Clark DM, Wilkins BS, editors. Infection and reactive changes. In: Bone Marrow Pathology. 4th ed. Oxford: Wiley Blackwell Publishing; 2010. p. 137-44.
- Unal S, Cetin M, Kutlay NY, Elmas SA, Gumruk F, Tukun A, et al. Hemophagocytosis associated with leukemia: A striking association with juvenile myelomonocytic leukemia. Ann Hematol 2010;89:359-64.
- Molad Y, Stark P, Prokocimer M, Joshua H, Pinkhas J, Sidi Y. Hemophagocytosis by small cell lung carcinoma. Am J Hematol 1991;36:154-6.
- Tsoi WC, Feng CS. Hemophagocytosis by rhabdomyosarcoma cells in bone marrow. Am J Hematol 1997;54:340-2.
- Filipovich AH. Hemophagocytic lymphohistiocytosis (HLH) and related disorders. Hematology Am Soc Hematol Educ Program 2009;127-31.
- Henter JI, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer 2007;48:124-31.
- Janka G, zur Stadt U. Familial and acquired hemophagocytic lymphohistiocytosis. Hematology Am Soc Hematol Educ Program 2005;82-8.
- Singh ZN, Rakheja D, Yadav TP, Shome DK. Infection-associated haemophagocytosis: The tropical spectrum. Clin Lab Haematol 2005;27:312-5.
- Wilson PA, Ayscue LH, Jones GR, Bentley SA. Bone marrow histiocytic proliferation in association with colony-stimulating factor therapy. Am J Clin Pathol 1993;99:311-3.
- Jordan MB, Hildeman D, Kappler J, Marrack P. An animal model of hemophagocytic lymphohistiocytosis (HLH): CD8+T cells and interferon gamma are essential for the disorder. Blood 2004;104:735-43.
- Rajagopala S, Dutta U, Chandra KS, Bhatia P, Varma N, Kochhar R. Visceral leishmaniasis associated hemophagocytic lymphohistiocytosis–Case report and systematic review. J Infect 2008;56:381-8.
- Yilmaz M, Vural F, Tobu M, Ertan Y, Buyuk F. Hemophagocytic syndrome with erythrocyte phagocytosis by the myeloid precursors in a patient with AML-M2. Turk J Hematol 2008;25:42-4.
- Celkan T. Aplastic anemia presenting as hemophagocytic lymphohistiocytosis. Turk J Hematol 2010;27:38-42.
- Hindupur S. Hemophagocytosis in hemophagocytic lymphohistiocytosis. Am J Hematol 2005;80:299-300.
- Gupta A, Tyrrell P, Valani R, Benseler S, Weitzman S, Abdelhaleem M. The role of the initial bone marrow aspirate in the diagnosis of hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer 2008;51:402-4.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.