Hepatitis E Virus Infection in the Perspective of Acuteon-chronic Liver Failure
2 Department of Medical Microbiology and Parasitology, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Malaysia, Email: niazlin_mt@gmail.com
Citation: Hudu SA. Hepatitis E Virus Infection: in the Perspective of Acute-on-chronic Liver Failure. Ann Med Health Sci Res. 2017; 7: 271-275
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Hepatitis E virus is a non-enveloped virus measuring 27 to 34nm, which belongs to the hepeviridae family. Its transmission is predominantly fecal oral and it is a common cause of acute viral hepatitis worldwide. Hepatitis E virus may cause serious disease, leading to high mortality in chronic liver disease patients, leading to the development of acute-on-chronic liver failure. Objective: This review aimed at summarizing the role played by HEV on the exacerbation of chronic hepatitis B and the pathophysiology of acute-on-chronic liver failure. Evidence acquisition: Peer-reviewed journal articles search were conducted using the university Putra Malaysia online subscribed databases in the area of Health Sciences and Medicine via Medline, SCOPUS and Google Scholar search engine. This review aims to summarize the impact of hepatitis E virus in acute-on-chronic liver failure pathogenesis. Development: Acute-onchronic liver failure has been considered an acute deterioration of liver function and clinical status in chronic hepatitis or cirrhotic patients. The transition from chronic hepatitis to cirrhotic as well as acute-on-chronic liver failure is mainly via pro-inflammatory cytokines; the clinical picture is similar to that of septic shock and multi-organ failure. Conclusion: Hepatitis E virusinfected patients may worsen and deteriorate to acute-on chronic infection, which constitutes two concurrent insults: acute and chronic with qualitatively different degrees of insult, leading to increased mortality as a result of organ failure with subsequent progression to multi-organ failure and being a leading cause of cirrhotic decompensation.
Keywords
Hepatitis E virus; Pro-inflammatory cytokines; Acute-on-chronic liver failure; Organ failure
Introduction
Hepatitis E virus (HEV) is the most recently discovered hepatropic virus, as its genome was identified in 1991 [1]. It is non-enveloped virus belonging to hepevirus in the family of hepeviridae, measuring 27 to 34 nm in size [2,3]. To date, four different HEV have been identified, of which genotypes 3 and 4 are increasingly being recognised in high income countries. In the developed world, autochthonous transmission of the virus causes both asymptomatic infections in healthy individuals as well as fulminant hepatitis in mostly immunocompromised patients. It commonly causes acute viral hepatitis worldwide and is transmitted predominantly via the faecal oral route; it causes large scale epidemics as well as sporadic cases in Africa and Asia [4,5]. HEV has a short incubation period of four to ten weeks. The virus is known to involve acute infection, with most of those who have contracted HEV infection showing clinical symptoms. However, studies have shown that, in endemic countries, the rate of infection is high, ranging from 50 to 60%, with the majority of patients having no symptoms [6]. On the other hand, HEV sero-prevalence in non-endemic countries was reported to be low, ranging from 1% to 10% and most are asymptomatic [7]. Acute viral hepatitis due to HEV is a self-limiting acute infection with similar clinical features with hepatitis A induced viral hepatitis. However, in two situations, HEV may cause serious disease, leading to high mortality: when acute viral hepatitis occurs in pregnant women which may rapidly worsen leading to acute liver failure, and when it occurs in chronic liver disease patients which may worsen to acute-onchronic liver failure (ACLF) [8].
The global medical and public health communities have begun to appreciate the significance of HEV infection, but there are still obstacles in global control of the impact of HEV and its mortality, such as scientific, cultural, economic and administrative obstacles. HEV remains relatively neglected despite its well documented and established global burden. Lack of awareness and credible robust laboratory and medical infrastructures are said to be hindering surveillance; hence, it is vital to improve global access equipment and services required for prompt and effective HEV identification, both in sporadic or nascent outbreak. Clinical and field surveillance as well as laboratory investigations will advance our understanding of HEV virulence, genotypes, sub-genotypic variation and global epidemiology. Both laboratory and clinical-based studies of patients infected with HEV have yielded exciting insight into its pathogenesis; however, more work is still needed for a better understanding of its chronic and extrahepatic infections leading to acute-onchronic liver failure. Hence, this review aimed at summarizing the role played by HEV on the exacerbation of chronic hepatitis B and the pathophysiology of acute-on-chronic liver failure.
Evidence acquisition
Peer-reviewed journal articles search were conducted using the university Putra Malaysia online subscribed databases in the area of Health Sciences and Medicine via Medline, SCOPUS and Google Scholar search engine. All searches were limited to, publication from 2000 to 2015 except where necessary an older publication was used. All publications were in English, and the final articles searched were those published till 31 May 2015, duplicates, conference abstract, comments and short communications were removed. The initial search result gave us 3,584 articles which were screened based on the title relevance, retaining 371 full text review articles out of which we cited 55 articles in this review.
Development
Hepatitis E infection
Infection with hepatitis E virus induces acute infection characterized by fever, jaundice, anorexia, and vomiting, which manifest at the onset of the initial exposure, coinciding with alanine transaminase (ALT) upsurge. The ALT level usually normalized during convalescence, but the symptoms may persist for months. It may be difficult to detect hepatitis E viraemia in patients that need clinical attention, but RNA can be detected in both stool and serum in early infection. Serological makers like anti-HEV IgM increases rapidly and decline following infection and some weeks after, while anti-HEV IgM continues to gradually rise during the period of gradual recovery (convalescent) and continue to be detectable for months or years.
Hepatitis E virus Transmission
Fecal oral transmission
The majority of HEV epidemics were found to be sourced from contaminated drinking water that is via the fecal oral route, similar to hepatitis A, but no person to person transmission has been reported as in hepatitis A. However, some vague transmissions occur in sporadic cases which are poorly understood. On the other hand, transmission of a Hepatitis E-like virus from animals or insect vectors has been reported in swine [9]. There is minimal transmission through blood and blood products because there is no chronic carrier state in HEV infection.
Vertical transmission
Hepatitis E virus can be transmitted vertically, as reported in previous studies,[10-12]. although the actual incidence remained unknown due to the small number of reported cases. For instance, in India, ten women were reported as having HEV in the third trimester, of which six developed fulminant liver failure, and three died; eight infants were delivered, of which five had HEV RNA-positive cord blood with elevated liver enzymes, and were HEV IgM positive at birth, which is strong evidence of vertical transmission. However, two of the neonates died and the autopsy results revealed massive hepatic necrosis [13].
Hepatitis E immune response
Hepatitis E infection is an acute self-limiting and causes liver failure; the clinical manifestations are due to immune response and not viral damage to hepatocytes. This is characterised by an increase in anti-HEV with a decrease in viral load, all coinciding with the onset of icteric symptoms and indicating immune system-mediated pathogenesis rather than virus-induced [6]. In a previous study of patients with HEV-induced acute liver failure, anti-HEV, interleukin-2, interleukin-10, interferon gamma and tumour necrosis factor alpha were found to be elevated [14]. At the onset of symptoms in infected patients, HEV-specific IgM and IgG appear in the sera, at the beginning of convalescence, the IgM declines sharply and can only be detected within two to three months,[15]. while IgG, on the other hand, persists for several years in infected individuals, for more than 14 years in about 47% of patients [16].
Acute-on-chronic liver failure
Acute-on-chronic liver failure is characterised by acute deterioration in liver function in cirrhotic patient as a result of secondary superimposed hepatic injury or due to extra-hepatic precipitation factors like infection, resulting in increased mortality due to multi-systemic organ failure as a result of acute deterioration of pre-existing chronic liver diseases [17]. In the Asian region, HBV reactivation has an important role in acuteon- chronic liver failure development [18]. Hepatitis A, B and E viruses are the predominant cause of infection in developing countries and the geographical variation depends on prevalent hepatotropic viruses.
Acute-on-chronic liver failure pathophysiology
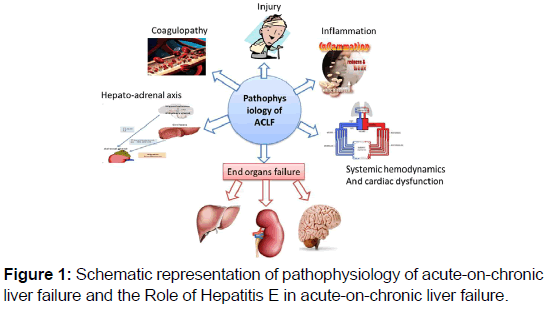
Acute-on-chronic liver failure pathophysiology occurs following established liver cirrhosis, with background precipitating events which may directly exaggerate liver injury. These events include co-infection with other viral hepatitis, ischemic hepatitis, alcoholic hepatitis, and drug-induced hepatitis and extra-hepatic insults such as trauma, variceal bleeding, infections or surgery may lead to hepatic decompensating [Figure 1]. However, in some patients there may be no precipitating events identified. Studies have shown that superimposed viral hepatitis and surgery are the best precipitating factors of ACLF development [19]. HEV has also been reported in southern China, central Asia, Africa and India as an important cause of ACLF leading to acute hepatic decompensation and death, with mortality being higher in patients with HEV super-infection than non-cirrhosis [Table 1].
| Prevalence of ACLF due to HEV (%) | Mortality rate (%) | Place/City | Year | Reference |
|---|---|---|---|---|
| 44 | 14 | Lucknow | 2004 | [39] |
| 75 | 100 | China | 2006 | [40] |
| 28 | 43 | Delhi | 2007 | [22] |
| 21 | 0 | Delhi | 2008 | [40] |
| 15 | - | Delhi | 2009 | [41] |
| 22 | 13 | Dhaka | 2009 | [42] |
| 66 | 44 | Lucknow | 2009 | [43] |
| 4 | 50 | Chandigarh | 2010 | [44] |
| 72 | 34 | China | 2010 | [23] |
| 10 | 33 | Chandigarh | 2011 | [45] |
| 13 | 23 | Egypt | 2011 | [46] |
| 64 | 35 | Lucknow | 2012 | [47] |
| 15 | 64 | Delhi | 2012 | [48] |
| 14 | 60 | Jaipur | 2013 | [49] |
| 15 | 50 | Chandigarh | 2013 | [50] |
Table 1: Prevalence and mortality rate of hepatitis E associated acute-on chronic liver failure in selected countries.
Patients with chronic liver diseases superimposed with hepatitis E infection were reported to be associated with hepatic decompensation for the first time in a study conducted in Pakistan in 2002 [20,21]. Since then, several studies have reported HEV as one of the leading causes of hepatic decompensation in cirrhosis from Asia and Africa, which are endemic for HEV [7,22]. in most of these studies, APASL definition for APALS was used and 72% of ACLF was found to be precipitated by HEV infection leading to hepatic decompensation. These findings were contrary to the findings in western countries, where hepatic decompensation is rarely caused by HEV in ACLF patients. However, this might be due to the low prevalence of HEV in such countries compared to Africa and Asia, where the largest number of studies that report HEV having acute insult on ACLF were from China [23].
Inflammatory cytokines role in acute-on-chronic liver failure
Pro-inflammatory cytokines as a result of systemic inflammatory response are responsible for stable cirrhosis transition to acuteon- chronic liver failure [24]. These necrosis, fibrosis, cholestasis and apoptosis mediators of inflammation, such as the proinflammatory cytokines nitric oxide, and oxidative stress, have shown increasing evidence of modulating the effects of hyperammonaemia in precipitin encephalopathy [25]. It has been shown in previous studies that patients with HEV infection have decreased peripheral CD4 with increased CD8 levels, thereby altering the CD4/CD8 ratio [26,27]. Similarly, the elevation of helper-2 associated cytokines like interleukin 4, 5, 10 and 13 were also reported [28-30].
Clinical features of ACLF
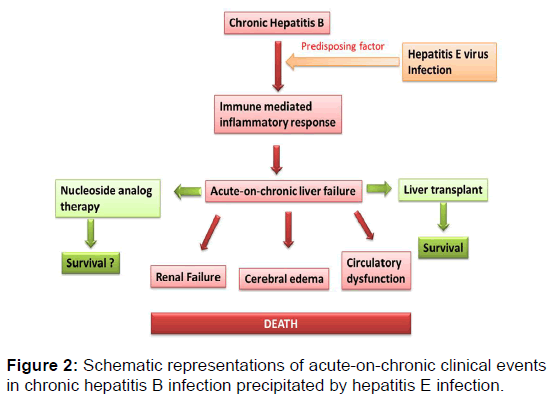
The manifestation of ACLF is as a result of altered function of the organs involved, primarily the liver, kidney, brain and circulatory system. Systemic inflammatory response when develop is said to be a poor prognostic factor which is associated with developing encephalopathy, hence reducing the chances of organ transplantation [31]. Therefore, the resulting cellular immune dysfunction and inflammatory responses in the liver can lead to circulatory, cerebral and renal dysfunction [Figure 2]; the presence of hyperbilirubinaemia with clinical jaundice is inevitable. The hepatic synthetic function is also reduced, leading to hypoalbuminaemia which will subsequently result to oedema and ascites. Hemorrhagic diathesis may result due to thrombocytopenia. The center stage of ACLF development is due to circulatory changes. The development of acute hepatic decompensation is a result of alterations in hepatic perfusion, leading to generalized haemodynamic changes that result in dehydration, gastrointestinal bleeding and sepsis. In ACLF, some of the changes that occur in cirrhosis become exaggerated; these include dilated hypo-responsive peripheral circulation, increased cardiac output, increased Porto-systemic shunting, increased portal pressure and decreased renal blood flow, all of which are reversible with liver transplants [32,33].
Laboratory investigation of ACLF
At the onset of HEV infection symptoms, the HEV antibodies, IgM and IgG appear early and subsequently respectively in the sera of infected patients. There is a sharp decline in IgM, which may be detected for only two to three months at the beginning of convalescence [34]. On the other hand, IgG persists in infected individuals for several years, more than 14 years in 47% of patients [16]. Therefore, testing for HEV antibodies can reveal acute infection by detecting IgM or chronic infection by detecting IgG in addition to HEV antigen.
The first step of investigating ACLF is to screen for the cause of infective aggravating factors, in this case viral hepatitis viruses such as hepatitis B, and E and viral load should be assessed where serology is positive to confirm the cause of the hepatic insult. After establishing the cause, the extent of hepatic injury should be determined by screening for makers of hepatic synthetic function such as prothrombin time, albumin and creatinine, the nature of the hepatic injury should be determined by the level of transaminases and alkaline phosphatase. Full blood count is needed to determine the features of hyperspleenism such as thrombocytopenia and leukopenia. The risk of sepsis should be ruled out by blood cultures. In patients presenting with ascites, there is a need for an ascites tap for microscopic culture and sensitivity and biochemical analysis. In the initial patient evaluation, abdominal ultrasound with Doppler plays an important role.
Management of hepatitis E Associated ACLF
Patients with ACLF require early interventions which are critical in reducing or correcting the injury, preventing further deterioration of liver function, supporting failing organs and reversing precipitating factors [17]. To achieve this, it required intensive care management and a team of experts in both hepatology and critical care [19]. Major decisions to be taken during the management of patient with ACLF depend on the patient’s clinical condition. In patients with hepato-renal syndrome, it is recommended to give volume expanders like albumin and vasoconstrictors aiming at decreasing serum creatinine to less than 1.2mg/dl. If a patient has increased intraabdominal pressure as a result of massive ascites, there is a need for large volume paracentesis in combination with albumin replacement therapy.
In hepatic encephalopathy, the main stay of treatment is the use of non-ascribable antibiotics and lactulose; correction and coagulopathy is not routine in the absence of active bleeding, as it can only be done when there is an associated significant complication such as transfusion, associated lung injury, circulatory overload and reaction [35]. Normal protein diet from 0.8 to 1.2 g/kg is recommended, except in critically ill cirrhotic patients, in which the protein requirement may be reduced based on the degree of metabolism and renal failure [17]. There is also no “tight” glucose control needed. However, maintaining blood sugar between 7.8 to 10 mmol /L is recommended in cirrhosis [17]. In patients with suspected infection, broad spectrum antibiotics can be given early, within one hour of admission, in line with early goal-directed therapy guidelines [17]. All ACLF patients admitted to intensive care unit should be consulted by live transplant expert to determine whether the patient is a suitable candidate for liver transplant. Acute HEV infection has no established treatment;[7]. however; PEGylated interferon alpha has been used successfully for treating chronic HEV in transplant recipient patients [36]. Ribavirin has also shown to induce a sustained virological response in chronically infected patients by inhibiting HEV RNA replication [36,37]. A preliminary study in India has shown that ribavirin may be a safe and effective drug for the treatment of HEV-associated ACLF [38].
Conclusion
In conclusion, hepatitis E virus infection in chronic liver disease patients may get worse and deteriorate to acute-on chronic infection, leading to an increase in mortality as a result of organ failure with subsequent progression to multi-organ failure and leading cause of cirrhotic decompensation in endemic regions. Treatment is aimed at preventing additional liver function deterioration, supporting failing organs and reversing precipitating factors.
Conflict of Interest
To the best of our knowledge no conflict of interest, financial or other, exists.
REFERENCES
- Reyes GR, Yarbough PO, Tam AW, Purdy MA, Huang C-C, Jung-suh PK, et al. Hepatitis E virus (HEV): the novel agent responsible for enterically transmitted non-A, non-B hepatitis. Gastroenterol Jpn.1991;26:142-147.
- Anderson NW, Buchan BW, Ledeboer NA. Light microscopy, culture, molecular, and serologic methods for detection of herpes simplex virus. J. Clin. Microbiol. 2014;52:2-8.
- Buchan BW, Ledeboer NA. Emerging technologies for the clinical microbiology laboratory. Clin Microbiol Rev. 2014;27:783-822.
- Szretter KJ, Balish AL, Katz JM. Influenza: propagation, quantification, and storage. Curr Protoc Stem Cell Biol. 2006:15G. 1.1-G. 1.22.
- Masalova O, Klimova R, Chichev E, Fediakina I, Loginova SY, Borisevich S, et al. Development of monoclonal antibodies to highly pathogenic avian influenza H5N1 virus and their application to diagnostics, prophylaxis, and therapy. Acta Virol. 2011;55:3.
- Krain LJ, Nelson KE, Labrique AB. Host immune status and response to hepatitis E virus infection. Clin Microbiol Rev. 2014;27:139-65.
- Pérez-Gracia MT, Suay B, Mateos-Lindemann ML. Hepatitis E: An emerging disease. Infection, Genet. Evol. 2014;22:40-59.
- Aggarwal R. Clinical presentation of hepatitis E. Virus Res. 2011;161:15-22.
- Emerson SU, Purcell RH. Hepatitis E virus. Rev Med Virol. 2003;13:145-154.
- Singh S, Mohanty A, Joshi Y, Deka D, Mohanty S, Panda S. Mother-to-child transmission of hepatitis E virus infection. Indian J Pediatr. 2003;70:37-39.
- Krain LJ, Atwell JE, Nelson KE, Labrique AB. Fetal and neonatal health consequences of vertically transmitted hepatitis E virus infection. Am J Trop Med Hyg. 2014;90:365-370.
- Xia J, Liu L, Wang L, Zhang Y, Zeng H, Liu P, et al. Experimental infection of pregnant rabbits with hepatitis E virus demonstrating high mortality and vertical transmission. J. Viral Hepat. 2015.
- Khuroo M, Kamili S. Clinical course and duration of viremia in vertically transmitted hepatitis E virus (HEV) infection in babies born to HEV‐infected mothers. J. Viral Hepat. 2009;16:519-523.
- Zhao W-D, CHEN J, LIU F-G, WANG M, LI J-M. Poster Abstracts–Liver. Chin J Dig Dis. 2005;6:A31-A51.
- Suman-Chauhan N, Webdale L, Hill DR, Woodruff GN. Characterisation of[3 H]. gabapentin binding to a novel site in rat brain: homogenate binding studies. Eur J Pharm-Molec Ph. 1993;244:293-301.
- Clayson ET, Myint KSA, Snitbhan R, Vaughn DW, Innis BL, Chan L, et al. Viremia, fecal shedding, and IgM and IgG responses in patients with hepatitis E. J. Infect. Dis. 1995;172:927-933.
- Olson JC, Kamath PS. Acute-on-chronic liver failure: concept, natural history, and prognosis. Curr Opin Crit Care. 2011;17:165-9 10.1097/MCC.0b013e328344b42d.
- Sarin SK, Kumar A, Almeida JA, Chawla YK, Fan ST, Garg H, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the study of the liver (APASL). Hepatol Int. 2009;3:269-282.
- Jalan R, Gines P, Olson JC, Mookerjee RP, Moreau R, Garcia-Tsao G, et al. Acute-on chronic liver failure. J Hepatol. 2012;57:1336-1348.
- Bosan A, Qureshi H, Bile KM, Ahmad I, Hafiz R. A review of hepatitis viral infections in Pakistan. J Pak Med Assoc. 2010;60:1045-1058.
- Wlodarczyk BJ, Palacios AM, George TM, Finnell RH. Antiepileptic drugs and pregnancy outcomes. Am J Med Genet A. 2012;158A:2071-2090.
- Kumar Acharya S, Kumar Sharma P, Singh R, Kumar Mohanty S, Madan K, Kumar Jha J, et al. Hepatitis E virus (HEV) infection in patients with cirrhosis is associated with rapid decompensation and death. J Hepatol. 2007;46:387-394.
- Zhang X, Ke W, Xie J, Zhao Z, Xie D, Gao Z. Comparison of effects of hepatitis E or A viral superinfection in patients with chronic hepatitis B. Hepatol Int. 2010;4:615-620.
- Yudkin JS, Kumari M, Humphries SE, Mohamed-Ali V. Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis. 2000;148:209-214.
- Wasmuth HE, Kunz D, Yagmur E, Timmer-Stranghöner A, Vidacek D, Siewert E, et al. Patients with acute on chronic liver failure display ‘sepsis-like’immune paralysis. J Hepatol. 2005;42:195-201.
- Prabhu S, Gupta P, Durgapal H, Rath S, Gupta S, Acharya S, et al. Study of cellular immune response against Hepatitis E Virus (HEV). J Viral Hepat. 2011;18:587-594.
- Mowafi F. Chemokines and chemokine receptors during viral infections in man: Institutionen för mikrobiologi, tumör-och cellbiologi/Department of Microbiology, Tumor and Cell Biology; 2007 Nov 8.
- Pal R, Aggarwal R, Naik SR, Das V, Das S, Naik S. Immunological alterations in pregnant women with acute hepatitis E. J Gastroenterol Hepatol. 2005;20:1094-1101.
- Deshmane SL, Kremlev S, Amini S, Sawaya BE. Monocyte chemoattractant protein-1 (MCP-1): an overview. J Interferon Cytokine Res. 2009;29:313-326.
- Liew FY, Pitman NI, McInnes IB. Disease-associated functions of IL-33: the new kid in the IL-1 family. Nat Rev Immunol. 2010;10:103-110.
- Rolando N, Wade J, Davalos M, Wendon J, Philpott‐Howard J, Williams R. The systemic inflammatory response syndrome in acute liver failure. Hepatology. 2000;32:734-739.
- Bosch J, García-Pagán JC. Complications of cirrhosis. I. Portal hypertension. J Hepatol. 2000;32:141-56.
- Newby DE, Jalan R, Masumori S, Hayes PC, Boon NA, Webb DJ. Peripheral vascular tone in patients with cirrhosis: role of the renin–angiotensin and sympathetic nervous systems. Cardiovasc Res. 1998;38:221-228.
- Chauhan A, Dilawari J, Chawla Y, Jameel S, Kaur U, Ganguly N. Hepatitis E virus transmission to a volunteer. The Lancet. 1993;341:149-150.
- Munoz SJ, Reddy KR, Lee W, Group ALFS. The coagulopathy of acute liver failure and implications for intracranial pressure monitoring. Neurocrit Care. 2008;9:103-107.
- Kamar N, Rostaing L, Abravanel F, Garrouste C, Lhomme S, Esposito L, et al. Ribavirin therapy inhibits viral replication on patients with chronic hepatitis E virus infection. Gastroenterology. 2010;139:1612-1618.
- Kamar N, Rostaing L, Legrand‐Abravanel F, Izopet J. How Should Hepatitis E Virus Infection Be Defined in Organ‐Transplant Recipients? Am J Transplant. 2013;13:1935-1936.
- Goyal R, Kumar A, Panda SK, Paul SB, Acharya SK. Case reports-Ribavirin therapy for hepatitis E virus-induced acute on chronic liver failure: A preliminary report. Antivir Ther. 2012;17:1091.
- Kumar A, Aggarwal R, Naik S, Saraswat V, Ghoshal UC, Naik S. Hepatitis E virus is responsible for decompensation of chronic liver disease in an endemic region. Indian J. Gastroenterol. 2004;23:59-62.
- Ke W-M, Li X-J, Yu L-N, Lai J, Li X-H, Gao Z-L, et al. Etiological investigation of fatal liver failure during the course of chronic hepatitis B in southeast China. J Gastroenterol. 2006;41:347-351.
- Kumar A, Das K, Sharma P, Mehta V, Sharma B, Sarin S. Hemodynamic Studies in Acute-on-Chronic Liver Failure. Dig Dis Sci. 2009;54:869-878.
- Mahtab M-A, Rahman S, Khan M, Karim MF. Hepatitis E virus is a leading cause of acute-on-chronic liver disease: experience from a tertiary centre in Bangladesh. Hepatobiliary Pancreat Dis Int. 2009;8:50-52.
- Radha Krishna Y, Saraswat VA, Das K, Himanshu G, Yachha SK, Aggarwal R, et al. Clinical features and predictors of outcome in acute hepatitis A and hepatitis E virus hepatitis on cirrhosis. Liver Int. 2009;29:392-398.
- Duseja A, Chawla YK, Dhiman RK, Kumar A, Choudhary N, Taneja S. Non-hepatic Insults Are Common Acute Precipitants in Patients with Acute on Chronic Liver Failure (ACLF). Dig Dis Sci. 2010;55:3188-3192.
- Lal J, Thapa BR, Rawal P, Ratho RK, Singh K. Predictors of outcome in acute-on-chronic liver failure in children. Hepatol Int. 2011;5:693-697.
- El Sayed Zaki M, Othman W. Role of hepatitis E infection in acute on chronic liver failure in Egyptian patients. Liver Int. 2011;31:1001-1005.
- Jagadisan B, Srivastava A, Yachha SK, Poddar U. Acute on Chronic Liver Disease in Children From the Developing World: Recognition and Prognosis. J. Pediatr. Gastroenterol. Nutr. 2012;54:77-82.
- Garg H, Kumar A, Garg V, Sharma P, Sharma BC, Sarin SK. Clinical profile and predictors of mortality in patients of acute-on-chronic liver failure. Dig Liver Dis. 2012;44:166-171.
- Jha A, Nijhawan S, Rai R, Nepalia S, Jain P, Suchismita A. Etiology, clinical profile, and inhospital mortality of acute-on-chronic liver failure: a prospective study. Indian J. Gastroenterol. 2013;324:108-114.
- Duseja A, Choudhary NS, Gupta S, Dhiman RK, Chawla Y. APACHE II score is superior to SOFA, CTP and MELD in predicting the short-term mortality in patients with acute-on-chronic liver failure (ACLF). J Dig Dis. 2013;14:484-490.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.