Impacted Laryngeal Foreign Body in a Child: A Diagnostic and Therapeutic Challenge
- *Corresponding Author:
- Dr. Shraddha Jain
Department of Otorhinolaryngology and Head and Neck Surgery, Jawahar Lal Nehru Medical College, DMIMSU, Sawangi, Wardha,Maharashtra - 442 004, India.
E-mail: sjain_med@yahoo.co.in
Citation: Jain S, Kashikar S, Deshmukh PT, Gosavi SN, Kaushal A. Impacted laryngeal foreign body in a child: A diagnostic and therapeutic challenge. Ann Med Health Sci Res 2013;3:464-6.
Abstract
Impacted laryngeal foreign body could lead to catastrophic consequences if appropriate diagnostic and therapeutic procedures are not promptly instituted. A case of 4‑year‑old child who presented with a 4‑day history of probable ingestion or aspiration of a pen part and history of occasional noisy breathing on exertion and swallowing is reported. On examination, the child appeared asymptomatic on general examination. CT scan of larynx and chest revealed foreign body in the larynx. A conical plastic foreign body in the laryngotracheal junction was retrieved by rigid bronchoscopy. The asymptomatic nature of the foreign body was related to the presence of a lumen within the foreign body permitting ventilation and the inert nature of the material. The case demonstrates the importance of the history, CT scan in case of suspicion, and the need for urgent bronchoscopy with appropriate anesthetic technique.
Keywords
Foreign body, Larynx, Lumen, Trachea
Introduction
Foreign body aspiration with asphyxiation is one of the leading causes of accidental deaths among children younger than 4 years.[1,2] Laryngeal foreign bodies are a rare occurrence in pediatric age group in comparison to bronchial foreign bodies.[3] The presentation of a laryngeal foreign body depends upon the size, shape, site, nature of foreign body, and the degree of obstruction leading to a great variability in symptoms.[2‑4] Complication rates for bronchoscopy and the laryngotracheal foreign body itself increase with the duration of the foreign body in situ.[5]
The present case is interesting to report due to the asymptomatic nature of a large impacted conical plastic laryngotracheal foreign body with a probable history of swallowing a foreign body. The diagnosis and management are discussed. The case highlights the importance of history even in the absence of physical signs in early diagnosis of laryngotracheal foreign bodies.
Case Report
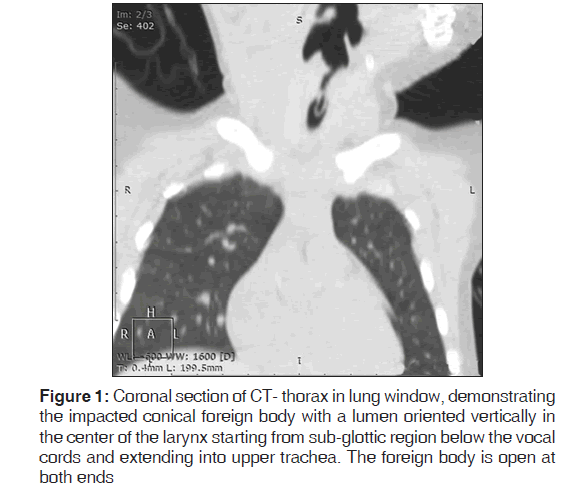
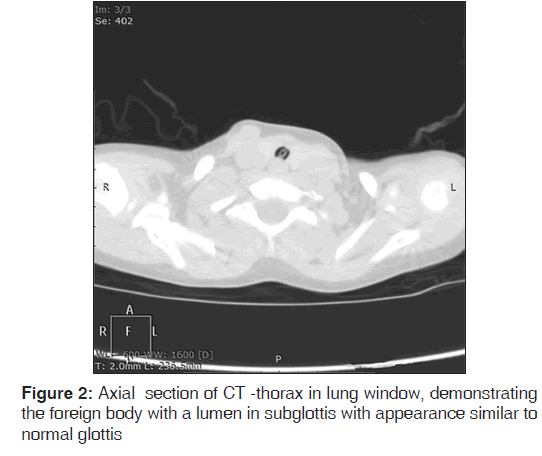
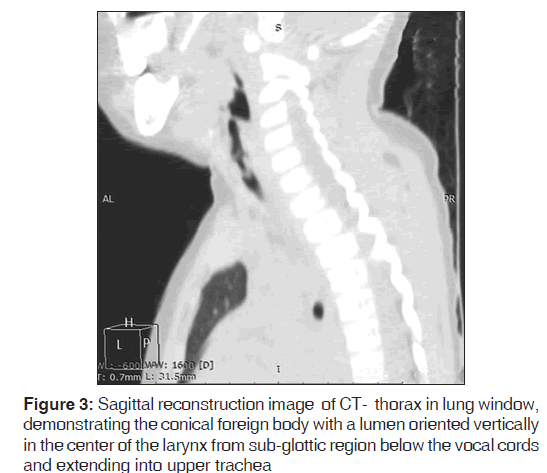
A 4‑year‑old boy was brought to otolaryngology emergency of our hospital to rule out suspected foreign body, a plastic pen anterior detachable segment, in his aero‑digestive tract. The history was given only by the child himself to the parents that a kid had forced him to swallow a pen cap in his play school, 4 days back. The surprising part was that apart from history of occasional respiratory wheeze on exertion and while swallowing, the child was totally comfortable and had no cough, change in voice, or respiratory distress. Respiratory system examination at rest was normal. An high resolution computed tomographic scan of neck with chest was advised and revealed a conical foreign body with a lumen just below the level of vocal cords [Figures 1‑3].
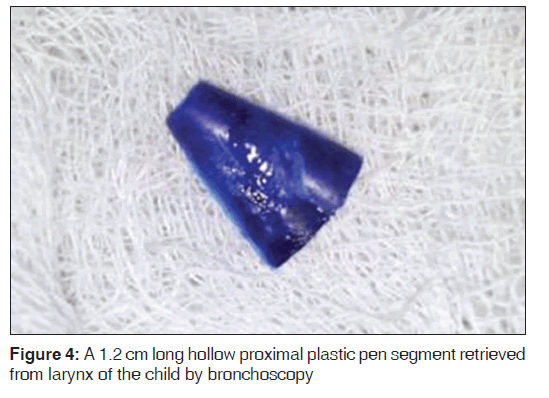
The patient was taken for urgent bronchoscopy. Injection glycopyrrolate, midazolam, and pentazocine were given as premedication. In addition, he received intravenous anesthesia (propofol and sevoflurane) with scoline as muscle relaxant. Intermittent apnea technique was employed, in which foreign body removal was attempted with a pediatric bronchoscope (Karl Storz ventilating rigid bronchoscope; size 4 mm) in the apnea period of 2‑3 minutes duration. As soon as patient came on spontaneous ventilation or saturation fell down, again injection scoline and atropine were given, and manual controlled ventilation was given with 100% oxygen. A blue‑colored conical foreign body was removed with forceps by trailing method in head low position with slight difficulty as it was impacted below the cords at the laryngotracheal junction [Figure 4]. The foreign body was a 1.2 cm long hollow proximal part of a plastic pen and was slightly flattened. Child was immediately extubated and kept in pediatric intensive care unit for 48 hours with injectable steroids for 3 days.
Before coming to our hospital, due to the lack of obvious symptoms, absent chest findings, and normal chest x‑ray, the foreign body was missed.
Discussion
The sub‑glottic region in children rapidly develops edema, but the foreign body in our case caused no respiratory distress. Tracheal foreign bodies are known to cause more severe symptoms with rapid deterioration as compared to bronchial foreign bodies.[2] Asymptomatic bronchial foreign bodies are much more common. Few cases of asymptomatic tracheal inorganic foreign bodies have been reported. One was a case of a hollow metallic cylindrical foreign body in mid‑trachea and other that of a plastic foreign body in trachea with a lumen.[2,6] Both these cases had foreign bodies with a lumen. The presence of a lumen within the foreign body permitting ventilation and the inert nature of the foreign body are factors responsible for relative lack of symptoms. The symptomatology of laryngeal foreign bodies depends on whether it produces complete or incomplete airway obstruction. In complete airway obstruction, the presentation is with catastrophic respiratory distress leading to apnea, cyanosis, loss of consciousness, and sudden death if foreign body is not dislodged. However, incomplete laryngeal obstruction may present with less severe symptoms and possible misdiagnosis or delay in diagnosis.[4] A history of choking and vocal changes is usually associated with laryngeal foreign bodies.[3] Other common presenting symptoms are stridor, wheezing, sternal retractions, and cough. They may be treated as croup or reactive airway disease poorly responding to medical line of management.[7] Laryngeal foreign bodies have been misdiagnosed as recurrent laryngitis or asthma for long duration in few instances.[8,9] Our patient had a plastic pen part with a lumen and completely obstructed the laryngotracheal junction. The history given by the child and occasional respiratory wheeze heard by the parents were the only clue to the diagnosis.
3 - dimensional CT scan is a more sensitive diagnostic modality for foreign body aspiration in comparison with conventional radiography and is increasingly becoming the imaging of choice, especially for radiolucent foreign bodies like plastic materials.[1,10] An inexpert radiologist can miss a laryngeal foreign body with a lumen on CT as the circular shadow of the foreign body in the airway can be confused with normal glottis. False‑positive findings can occur due to mucous plugs, tumors, or other obstructive lesions and decrease the specificity of CT.[1,10] CT – imaging has disadvantages of radiation exposure and can be done only in stable and co‑operative children as an unstable object can potentially acutely obstruct the airway with grave consequences.
The anesthetic technique most favored for rigid bronchoscopic removal of laryngotracheal foreign bodies is controlled ventilation with intermittent apnea technique combined with intravenous drugs and paralysis.[1] While performing rigid bronchoscopy, large laryngotracheal foreign bodies may be lost during extraction through the narrow sub‑glottic area. Uncontrolled, they may quickly migrate back to the carina, change axis from vertical to horizontal or oblique, and produce airway obstruction, cardiopulmonary arrest, and cerebral hypoxia. Removal of a foreign body of this region is challenging and may need a tracheostomy as a route for bronchoscopic retrieval if bronchoscopy through the mouth is not possible due to an edematous larynx.[11] In case of complete airway obstruction in case the foreign body gets stucked up in larynx or trachea, it may need to be pushed back into the right mainstem bronchus to provide an airway for ventilation through the left mainstem bronchus till the time tracheostomy is being performed.
Conclusion
A large foreign body occupying laryngotracheal region without any symptoms is a rare occurrence. A suspected history of ingestion or aspiration of a foreign body in the absence of physical signs is enough to warrant a high‑resolution CT‑scan of neck and chest with 3‑dimensional reconstruction to rule out a foreign body. Urgent bronchoscopic removal with arrangements ready for tracheostomy is indicated.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: A literature review of 12,979 cases. Anesth Analg 2010;111:1016-25.
- Mathiasen RA, Cruz RM. Asymptomatic near-total Airway obstruction by a Cylindrical Tracheal foreign body. Laryngoscope 2005;115:274-7.
- Bloom DC, Christenson TE, Manning SC, Eksteen EC, Perkins JA, Inglis AF, et al. Plastic laryngeal foreign bodies in children: A diagnostic challenge. Int J Pediatr Otorhinolaryngol 2005;69:657-62.
- Robinson PJ. Laryngeal foreign bodies in children: First stop before the right main bronchus. J Paediatr Child Health 2003;39:477-9.
- Zaytoun GM, Rouadi PW, Bali DH. Endoscopic management of foreign bodies in the tracheobronchial tree: Predictive factors for complications. Otolaryngol Head Neck Surg 2000;123:311-6.
- Davis SJ, Madden G, Carapiet D, Nixon, Dennis S, Pringle M. Delayed presentation of paediatric tracheal foreign body. Eur Arch Otorhinolaryngol 2007;264:833-5.
- Esclamado RM, Richardson MA. Laryngotracheal foreign bodies in children. A comparison with bronchial foreign bodies. Am J Dis Child 1987;141:259-62.
- Atmaca S, Unal R, Sesen T, Kili�arslan H, Unal A. Laryngeal foreign body mistreated as recurrent laryngitis and croup for one year. Turk J Pediatr 2009;51:65-6.
- Chavoshzadeh Z, Golnabi A, Rezaei N, Mehdizadeh M. Laryngeal foreign body aspiration misdiagnosed as asthma: Two case reports and a review of the literature. B-ENT 2011;7:137-40.
- Hong SJ, Goo HW, Roh JL. Utility of spiral and cine CT scans in pediatric patients suspected of aspirating radiolucent foreign bodies. Otolaryngol Head Neck Surg 2008;138:576-80.
- Swensson EE, Rah KH, Kim MC, Brooks JW, Salzberg AM.Extraction of large tracheal foreign bodies through a tracheostoma under bronchoscopic control. Ann Thorac Surg 1985;39:251-3.




 The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.
The Annals of Medical and Health Sciences Research is a monthly multidisciplinary medical journal.